RESEARCH ARTICLE
Doi: 10.5578/tt.60781
Tuberk Toraks 2018;66(1):00-00

Pakistan, Hazara B?lgesinde akciğer t?berk?lozu hastalarının
birinci basamak tedavilerinde Mycobacterium tuberculosis ila? direnci paterni
Faheem JAN1,2, Shahid WALI1, Sadia1, Muhammad Taj AKBAR3, Hafiz Sajid AKBAR4, Waqas AHMAD5, Manzoor AHMAD2, Anwar KHALID2,6
1 DR-TB ?nitesi Ayub Eğitim Hastanesi, Abbottabad KPK, Pakistan
1 DR-TB Unit Ayub Teaching Hospital, Abbottabad KPK, Pakistan
2 Hazara ?niversitesi, Biyokimya Anabilim Dalı, Mansehra KPK, Pakistan
2 Department of Biochemistry, Hazara University, Mansehra KPK, Pakistan
3 Hazara ?niversitesi, Mikrobiyoloji Anabilim Dalı, Mansehra KPK, Pakistan
3 Department of Microbiology, Hazara University, Mansehra KPK, Pakistan
4 Abbottabad Bilim ve Teknoloji ?niversitesi Eczacılık B?l?m?, Abbottabad, Pakistan
4 Department of Pharmacy, Abbottabad University of Science and Technology, Abbottabad, Pakistan
5 Sargodha ?niversitesi Eczacılık Fak?ltesi, Sargodha, Pakistan
5 Faculty of Pharmacy, University of Sargodha, Sargodha, Pakistan
6 ?ğrenci İşleri COMSATS ?niversitesi Islamabad, Abbottabad Kamp?s?, Pakistan
6 Student Affairs, COMSATS University Islamabad, Abbottabad Campus, Pakistan
?ZET
Pakistan, Hazara B?lgesinde akciğer t?berk?lozu hastalarının birinci basamak tedavilerinde Mycobacterium tuberculosis ila? direnci paterni
Giriş: En azından rifampisin ve izoniazide birlikte diren? olması olarak tanımlanan ?ok ilaca diren?li t?berk?loz (?İD-TB) son yıllarda hızla yayılmaktadır. Yeni akciğer t?berk?lozu olgularında, ?İD-TB'nin hızlı yayılması ve XİD-TB, Ulusal TB kontrol programlarının etkinliğini ?zellikle d?ş?k gelir d?zeyi olan ?oğu ?lkelerde zorlaştırmaktadır. Bu araştırma yeni olgu, tedavi olmuş olgu, tedavi başarısızlığı, relaps, tedavisi tamamlanmış, tedavisi değerlendirilmemiş ve birinci kuşak antit?berk?loz ila?lara diren? ş?phesi olan olgularda Mycobacterium tuberculosis diren? paternini belirlemeyi ama?lamaktadır.
Materyal ve Metod: Bu araştırmaya 2013-2016 yılları arasında akciğer t?berk?lozu ile infekte olan 148 hasta dahil edildi. Ardışık ?? balgam ?rneği alınmış ve ila? analizi i?in alındıktan sonra ?? g?n i?inde +4?C'de tutularak Hayatabad Medikal kompleks i?inde Peshawar (HMCP) TB laboratuvarına g?nderildi. Standart orantı y?ntemi kullanılarak 132 (%89.2) balgam ?rneği ile rifampisin (R), isoniazid (H), pirazinamid (Z), etambutol (E) ve streptomisin (S) i?in ila? duyarlılığı testi uygulandı.
Bulgular: Tek ila? direnci prevalansı 5 (%3.4) olarak bulundu. En y?ksek tek ila? direnci oranı 3 (%2) ile E, sırasıyla 1 (%0.7) ile H ve 1 (%0.7) ile R'ye karşı bulundu. On d?rt (%9.5) hastada iki ilaca diren?, 3 (%2) hastada polirezistans ve 112 (%93.3) hastada ?İD-TB saptandı.
Sonu?: Etkin bir rejimi oluşturmak i?in ila? diren? mekanizmalarını bilmek ?nemlidir. ??nk? diren? ?zellikleri zaman ve yere bağlı olarak değişmektedir.
Anahtar kelimeler: Mycobacterium tuberculosis, İla? direnci paterni, ?ok ilaca diren?li t?berk?loz, İla? duyarlılık testi
SUMMARY
Drug resistance pattern in Mycobacterium tuberculosis to the first line drugs of pulmonary tuberculosis patients at Hazara Region, Pakistan
Introduction: Multidrug resistant TB (MDR-TB), defined as resistance to at least rifampicin and isoniazid together, has been rapidly spreading in recent years. In new pulmonary tuberculosis patients, rapid spread of MDR-TB and XDR-TB challenging the effectiveness of national TB control programs especially in many low-income countries. This study was aimed to determine the resistance pattern of Mycobacterium tuberculosis among new cases, cured, failure, relapse, defaulted, treatment completed, treatment not evaluated and suspect to be resistant to first line antitubercular drugs of pulmonary tuberculosis (PTB).
Materials and Methods: The study was conducted during 2013-2016 in which 148 patients were enrolled infected with pulmonary TB. Three sputum samples were consecutively collected and transported for drug analysis to the Provincial Reference Laboratory (PRL) at Hayatabad Medical complex Peshawar (HMCP) TB laboratory, within three days of collection at +4?C in a cold box. Using the standard proportion method, drug susceptibility test was performed on 132 (89.2%) sputum samples for rifampicin (R), isoniazid (H), pyrazinamide (Z), ethambutol (E), and streptomycin (S).
Results: Prevalence of resistance to one drug was 5 (3.4%). The highest proportion of mono-drug resistance was observed against E, 3 (2%), followed by H, 1 (0.7%), and R, 1 (0.7%). Pattern of resistant to two drugs was 14 (9.5%). The proportion of poly resistant was 3 (2%). 112 (93.33%) diagnose patients were MDR-TB.
Conclusion: To formulate an effective regimen, it is important to know drug resistant pattern because drug resistant pattern varies from different period of time also from one place to another.
Key words: Mycobacterium tuberculosis, Drug resistant pattern, Multidrug resistance tuberculosis, Drug sensitivity testing
Geliş Tarihi/Received: 22.09.2017 - Kabul Ediliş Tarihi/Accepted: 20.02.2018
INTRODUCTION
Tuberculosis (TB) is an infectious disease caused by bacterial strains belonging to the Mycobacterium tuberculosis complex. Various implications for management and treatment may be carried out by difference in drug resistant pattern (1). For the purposes of monitoring, on the basis of drug sensitivity testing (DST) in clinical isolates of M. tuberculosis, drug-resistant cases were categorized as multidrug resistance (MDR); resistance to rifampicin and isoniazid together, extensive drug resistance (XDR); when there is resistance to one of the second line injectable, to any fluoroquinolone and multidrug resistance (2) and rifampicin resistance (RR); genotypic and phenotypic detection of rifampicin resistance, without or with development of resistance to any other anti-tuberculosis drugs. Includes mono-drug resistance, poly-drug resistance, MDR or XDR (3). Multidrug resistant TB (MDR-TB), defined as resistance to at least rifampicin and isoniazid together, has been rapidly spreading in recent years. In 2012, globally assessed that incidence of MDR-TB was 3.6% and 20% cases of MDR-TB, having variation in prevalence with evident geography (4). The rate of MDR-TB ranges from 1.4% to 11.6% while resistance to one or more anti tubercular drugs ranges 3% to 37.3% in Africa (5-8). In new pulmonary tuberculosis patients in many low-income countries rapid spread of MDR-TB and XDR-TB challenging the effectiveness of national TB control programs (8,4). To strengthen the treatment outcomes and to control spread of resistant strains of M. tuberculosis especially MDR-TB. Early diagnosis, treatment, expanding diagnostic capacity for mycobacterial culture and drug susceptibility test (DST) are very important (4). This study was aimed to determine the resistance pattern of M. tuberculosis among new cases, cured, failure, relapse, defaulted, treatment completed, treatment not evaluated and suspect to be resistant to first line antitubercular drugs of pulmonary tuberculosis (PTB).
MATERIALS and METHODS
Samples Collection and Transportation
The samples were collected and transported in sterile conditions as recommended by WHO, three sputum samples (spot, morning, and spot) were consecutively collected from each study participant (9). Ziehl-Neelsen (ZN) positive samples were collected and transported to the Provincial Reference Laboratory (PRL) at Hayatabad Medical complex Peshawar (HMCP) TB laboratory for DST, within the three days of collection at +4?C in a cold box. At HMCP, for each patient the sputum samples were pooled into 50 mL sterile screw capped bottle and processed within 24 hours for mycobacterial culture (10).
This study was conducted at Programmatic management of Drug Resistant Tuberculosis unit, Ayub Teaching Hospital (PMDT-ATH) Abbottabad, Pakistan. The study population included 148 patients.
Exclusion Criteria and Inclusion Criteria
Patients with extrapulmonary or having history of second line antituberculosis treatment were excluded.
All those patients were included in the study who had conformed rifampicin resistant through GeneXpert, Ziehl-Neelsen staining positive for acid fast bacilli, having strong suspect to be drug resistant, previous history of antitubercular treatment (Category I and Category II) and from their radiographic examination.
Ethical Approval
The study was approved by the institutional review board (IRB), of Ayub Medical Institute, Abbottabad, Pakistan.
Isolation and Detection of M. tuberculosis
2.5-10 mL volume sample of sputum was digested, homogenized and decontaminated using standard method as reported by Kent and Kubica (11). The samples were concentrated by centrifugation for 15 minutes at 3000 rpm, and remove the supernatants. Sediments were reconstituted with Sterile saline phosphate buffer (PBS). Initially the pellets of the sediments were inoculated on Lowenstein Jensen (LJ) slants (contain glycerol (0.75%) and pyruvate (0.6%) and incubated for 8 weeks at 35-37?C and then growth was measured and conformed by ZN staining and microscopy (12).
Drug Susceptibility Testing
Using indirect proportion method on LJ media, drug susceptibility testing was performed for rifampin (R, 1 g/mL), isoniazid (H, 0.2 g/mL), ethambutol (E, 5 g/mL), pyrazinamide (PZA) and streptomycin (S, 2 g/mL) (13). Bacterial suspensions were prepared and inoculated on L.J Slants containing the drugs. Subsequently, the L.J slants were incubated at 35-37?C. Isolates were considered resistant by observing growth on slants.
RESULTS
Sociodemographic Characteristic
Sociodemographic characteristics of the entire patients are presented in Table 1. A total of 148 sputum samples were collected from new pulmonary tuberculosis patients. Comprised of 65 (44%) were male while 83 (56%) were females, of whom 91 (61.5%) were married, having the literacy rate 95 (64.2%). One twenty-one (81.8%) of these patients belonging to the rural area while most of these patients were house wives 75 (50.7%). The mean age of patients was 32.47 (SD + 15.99).
Drug Susceptibility Pattern
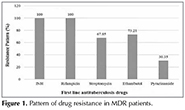
Drug susceptibility testing (DST) of M. tuberculosis isolates for 148 sputum samples were performed on first line anti tuberculosis drugs (H, R, Z, E and S). Drug susceptibility test showed that 12 (8.1%) sputum samples were sensitive to all the tested drugs. As of the total patients 120 (94.6%) showed drug resistance to at least one or more of the first line drugs by different patterns while out of the tested samples 16 (10.8%) cultures were reported as contaminated or did not reveal any growth. Prevalence of overall resistance to one drug was 5 (3.4%). The highest proportion of mono resistance was observed against E, 3 (2%), followed by H, 1 (0.7%), and R, 1 (0.7%). Pattern of combined resistant towards two drugs was 14 (9.5%). The proportion of poly resistant was 3 (2%). A comprehensive detail of the mono and poly drug resistance pattern is given in Table 2. Furthermore, 112 patients were diagnosed as MDR-TB. Drug susceptibility testing among MDR patients is shown in Figure 1, in which 100% resistance was shown by the cultures against isoniazid and rifampicin. During the study period, performance of the Drug Resistant Tuberculosis unit, Ayub Teaching Hospital (PMDT-ATH) Abbottabad, Pakistan was also analyzed with respect to facilitation and treatment of the patients. During this period, total 5.4% new TB cases were registered, while 17.6% were cured, 60 (40.54%) of failure cases were attributed to previous ATT history as depicted in figure 2, but 7.43% patients were successfully treated.
DISCUSSION
The high magnitude of MDR-TB was found among the poor, lower economic class people and illiterate. In earlier studies these factors were also reported (14,15). Economic status of the patients revealed that TB was converted to MDR-TB mostly in females (56.08%). In Pakistan females are more immune-compromised and limited to home in most of their life span, so the restricted environment, improper ventilation and poor hygienic conditions are responsible for such type of infections. Findings of this study agreed with previous published reports (16-18) who reported more prevalence in female population. In Balochistan Pakistan it is also revealed by previous study report that ratio of male to female was 1:14 in case of tuberculosis as reported by Dogar et al. (19) is a great matter of concern. In western province of Pakistan women are also neglected in term of treatment as they are mostly restricted to be household women, which will maximize the likelihoods of more contacts with infected one. Disease in this study was found in all age groups equally but was highest in productive and mature age group of 21-40 years which is (46.76%). Finding of this study was in line with previous study by (20-22) who reported that tuberculosis is a disease of adult productive 20-50 years age group.
In this study, total 148 samples were subjected for culture which were sputum positive out of which 132 (89.2%) samples had growth at end of 8 weeks, while the rest 16 (10.8%) samples did not reveal any growth. For all first line antitubercular drugs such as rifampicin, isoniazid, ethambutol, streptomycin and pyrazinamide drug sensitivity testing (DST) were carried out. 12 specimens (8.1%) were observed sensitive to all first line antitubercular drugs, while in remaining 120 (81.08%) of the cases resistance to one or more drugs was seen. MDR were obtained in 112 (75.7%) strains of M. tuberculosis. Resistance of mono and poly drugs was found in 5 (3.4%) and 3 (2.02%) isolates respectively. Variable patterns of resistance were observed in 112 MDR-TB isolates, out of which the most resistant pattern was against HRES 41 (36.6%) followed by HREZS 20 (17.9%) respectively. The observed resistance to two or more than two drugs was 77.7%.
Several risk factors were investigated to assess the association of drug resistance development. In development of drug resistant TB one of the strongest risk factor is the previous history of pulmonary TB. In the presence study MDR-TB development is significantly contributed by illiteracy and low socioeconomic status. In TB due to poor compliance which is related directly to financial burden on the family and illiteracy leads to higher prevalence of MDR-TB.
Conclusion
In this study the observed high rate of acquired drug resistance shows that National TB control program is not effective and during recent years improper/irregular use of antituberculosis drugs have led to multiplication and accumulation of drug resistant strains of M. tuberculosis.
For the control of TB disease, a compounding factor is MDR-TB. MDR-TB is a man-made problem and efforts should be taken to prescribe the suitable regimen for the prescribed duration of the treatment. To formulate an effective regimen, it is important to know drug resistant pattern because drug resistant pattern varies from different period of time also from one place to another.
REFERENCES
- Iseman MD. Treatment of multidrug-resistant tuberculosis. N Engl J Med 1993;329(11):784-91.
- WHO. Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis. In: Companion handbook to the WHO guidelines for the programmatic management of drug-resistant tuberculosis 2014.
- Jaramillo E. Guidelines for the programmatic management of drug-resistant tuberculosis. World Health Organ 2008.
- WHO. Global tuberculosis report 2013. World Health Organ.
- Glynn JR, Crampin AC, Traore H, Yates MD, Mwaungulu FD, Ngwira BM, et al. Mycobacterium tuberculosis Beijing genotype, northern Malawi. Emerg Infect Dis 2005;11(1): 150-3.
- Kassa-Kelembho E, Bobossi-Serengbe G, Takeng E, Nambea-Koisse T, Yapou F, Talarmin A. Surveillance of drug-resistant childhood tuberculosis in Bangui, Central African Republic. Int J Tuberc Lung Dis 2004;8(5):574-8.
- Kuaban C, Bercion R, Noeske J, Cunin P, Nkamsse P, Ngo Niobe S. Anti-tuberculosis drug resistance in the West Province of Cameroon. Int J Tuberc Lung Dis 2000;4(4):356-60.
- Lin J, Sattar A, Puckree T. An alarming rate of drug-resistant tuberculosis at Ngwelezane Hospital in northern KwaZulu Natal, South Africa. Int J Tuberc Lung Dis 2004;8(5):568-573.
- WHO. Guidelines for surveillance of drug resistance in tuberculosis 2009.
- Urassa W, Mugusi F, Villamor E, Msamanga G, Moshiro C, Bosch R, et al. Primary antimicrobial resistance among Mycobacterium tuberculosis isolates from HIV seropositive and HIV seronegative patients in Dar es Salaam Tanzania. BMC Res Notes 2004;1(1):58.
- Kent PT, Kubica GP. Public health mycobacteriology: a guide for the level III laboratory. US Department of Health and Human Services, Public Health Service, Centers for Disease Control 1985.
- Huard RC, de Oliveira Lazzarini LC, Butler WR, van Soolingen D, Ho JL. PCR-based method to differentiate the subspecies of the Mycobacterium tuberculosis complex on the basis of genomic deletions. J. Clin Microbiol 2003;41(4):1637-50.
- Canetti G, Fox W, Khomenko AA, Mahler H, Menon N, Mitchison D, et al. Advances in techniques of testing mycobacterial drug sensitivity, and the use of sensitivity tests in tuberculosis control programmes. Bull World Health Organ 1969;41(1):21.
- Portaels F, Rigouts L, Shamputa I, Van Deun A, Abdel Aziz M. Tuberculosis drug resistance in the world. Reichman and Hershfield's Tuberculosis; A Comprehensive, International Approach. 3rd ed. 2006.
- Oliva V, Cez?rio G, Cocato R, Marcondes-Machado J. Pulmonary tuberculosis: hematology, serum biochemistry and the relation with the disease duration. J Venom Anim Toxins Incl Trop Dis 2008;14(1):71-81.
- Ayaz S, Nosheen T, Khan S, Khan SN, Rubab L, Akhtar M. Pulmonary tuberculosis: still prevalent in human in Peshawar, Khyber Pakhtunkhwa, Pakistan. Pakistan Journal of Life Sciences 2012;10:39-41.
- Baloch S, Devrajani B, Rahman A. The prevalence of smear positive pulmonary tuberculosis in Hyderabad, Sindh, Pakistan. Elixir Human Physio 2013;60:16447-50.
- Ullah S, Shah SH, Rehman A, Kamal A, Begum N, Khan G. Extrapulmonary tuberculosis in Lady Reading Hospital Peshawar, NWFP, Pakistan: survey of biopsy results. J Ayub Med Coll Abbottabad 2008;20(2):43-6.
- Dogar OF, Shah SK, Chughtai AA, Qadeer E. Gender disparity in tuberculosis cases in eastern and western provinces of Pakistan. BMC Infect Dis 2012;12(1):244.
- Sutherland I, Fayers PM. The association of the risk of tuberculous infection with age. Bull Int Union Tuberc Lung Dis 1974;50(1):70-81.
- Shafee M, Abbas F, Ashraf M, Mengal MA, Kakar N, Ahmad Z, et al. Hematological profile and risk factors associated with pulmonary tuberculosis patients in Quetta, Pakistan. Pak J Med Sci 2014;30(1):36.
- Ahmad T, Jadoon MA, Khattak MNK, et al. Prevalence of sputum smear positive pulmonary tuberculosis at Dargai, District Malakand, Pakistan: A four year retrospective study. Egypt J Chest Dis Tuberc 2016;65(2):461-4.
Yazışma Adresi (Address for Correspondence)
Anwar KHALID
Department of Biochemistry,
Hazara University, Mansehra KPK
MANSEHRA - PAKISTAN
e-mail: anwar_khalid147@yahoo.com