LETTER TO THE EDITOR
Doi: 10.5578/tt.24132
Tuberk Toraks 2017;65(4):351-353

Bronchial atresia in an adult misdiagnosed as pulmonary mass
Melike DEMİR1, Mahşuk TAYLAN1, S?reyya YILMAZ1, Elif DURSUN1, Cengizhan SEZGİ1, Recep IŞIK1
1 Department of Chest Diseases, Faculty of Medicine, Dicle University, Diyarbakir, Turkey
1 Dicle ?niversitesi Tıp Fak?ltesi, G?ğ?s Hastalıkları Anabilim Dalı, Diyarbakır, T?rkiye
To The Editor,
Bronchial atresia is a congenital anomaly where lobar or segmental bronchi end bluntly upon an interruption and which is accompanied by mucoid impaction in the periphery and hyperinflation in the obstructed lung segment (1). It is observed generally in the upper lobar bronchus and frequently in the apicoposterior segment of the left upper lobe (2). It is mostly asymptomatic and more common among males (2).
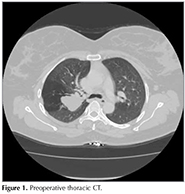
A 40-year-old female patient presented to the polyclinic with complaints of coughing and shortness of breath that were present in the past two months, but exacerbated further in severity in the past week. The physical examination showed more pronounced rhoncus in the right side. The patient had received treatment for non-specific infections at other centers. Furthermore, the results of positron emission tomography/computer-assisted tomography (PET-CT) obtained by reason of the request of another centre were compiled in a report which indicated the absence of pathologic uptake. Thoracic CT resulted in the observation of a 3 x 3 x 5 cm low-density mass lesion adjacent to the major fissure in the posterior segment of the upper lobe of the right lung with no indication of the bronchus of the same lobar segment and the indication of trapped air in the periphery of the lesion (Figure 1). Fiberoptic bronchoscopy (FOB) showed that the inlet mucosa in the posterior segment of the right upper lobe had been narrowed down due to external pressure and all other lobar and segmental inlets were open. The patient was diagnosed radiologically and clinically with atresia in the posterior segment of the upper lobe of the right lung. As the patient's complaints did not recede despite bronchodilator therapy, the thoracic surgery department was consulted and the patient underwent an operation. The operation removed fluid-filled cystic lesion and the pathological examination indicated it to be lung tissue featuring emphysematous changes. Post-operative thoracic CT indicated smaller dimensions for the low-density mass when compared to that in the pre-operative phase (Figure 2). The patient has been on follow-up at our polyclinic for the past two years and currently has no complaints.
Bronchial atresia is a rare anomaly of the bronchial tree. The separated part is filled with bronchial secretion and expands into a cystic structure and/or mucocele (3). It mostly creates a mass- or nodule-like image in the chest radiography. The symptoms? generally result from infection or compression exerted by, mucocele and/or cystic structure on the bronchi. The present patient also had localized rhoncus and shortness of breath due to compression of upper lobe bronchus. A study evaluating eighty-six bronchia atresia cases has determined recurrent infections in 21%, shortness of breath in 12% and coughing in 5% of the cases and reported 58% of the cases to be asymptomatic (1). The localization is frequently observed to be in the left upper lobe in 64%, in the left lower lobe in 14% and in the lower lobe in 8% of cases (4-6). The literature reports increased incidence in the male sex, among new-borns or in middle-aged individuals (1,2). Our patient was female and the atresia was located in the posterior segment of the right upper lobe.
The coexistence of typical findings such as mucocele, segmental hyperinflation and hypervascularity are diagnostically determinative (5). Most cases exhibit hyperinflation and hilar mass together. The cause of hyperinflation is the accumulation of the air inhaled through the collateral paths in peripheral areas of the lung (4). The patient had a mass due to the formation of mucocele and trapped air in the pulmonary areas immediately behind the mass. FOB led to the observation that the inlet of the posterior segment had been narrowed down due to the external compression, but other bronchial systems were open and normal. Similar to the cases of Gohil et al., pathologic FDG uptake of the lesion was not determined in PET-CT of our patient. Bronchial atresia may resemble a number of pathologies including tumours, allergic bronchopulmonary aspergillosis (ABPA), arteriovenous malformations, pulmonary sequestration and bronchogenic cysts (8). Magnetic resonance imaging (MRI) is quite useful in differentiation of atresia from vascular lesions. ABPA and arteriovenous malformations are not associated with increased aeration in the periphery of the lesion (2). Asymptomatic bronchial atresia is generally followed up without any course of treatment. The choice of treatment for symptomatic patients is surgery. The present patient was also subject to surgical treatment due to the persistent nature of the symptoms.
In conclusion, it should be considered that lesions radiologically observed as masses do not necessarily have to be malignant tumours. The being lesion of bronchial atresia may be diagnosed with the observation of increased aeration around the periphery of mass-like lesions in thoracic CT and lack of pathologic FDG uptake in PET-CT. Therefore, these diagnostic tools may prevent unnecessary invasive procedures.
REFERENCES
- Jederlinic PJ, Sicilian LS, Baigelman W, Gaensler EA. Congenital bronchial atresia. A report of 4 cases and a review of the literature. Medicine (Baltimore) 1987;66:73-83.
- Suemitsu R, Yoshino I, Tomiyasu M, Fukuyama S, Koto H, Sugimachi K. Asymptomatic atresia of the lobar bronchus of the lung: a case report. Ann Thorac Cardiovasc Surg 2001;7:301-3.
- Wang Y, Dai W, Sun Y, Chu X, Yang B, Zhao M. Congenital bronchial atresia: diagnosis and treatment. Int J Med Sci 2012;9:207-12.
- Matsushima H, Takayanagi N, Satoh M, Kurashima K, Kanauchi T, Hoshi T, et al. Congenital bronchial atresia: radiologic findings in nine patients. J Comput Assist Tomogr 2002;26:860-4.
- Beigelman C, Howarth NR, Chartrand-Lefebvre C, Grenier P. Congenital anomalies of tracheobronchial branching patterns: spiral CT aspects in adults. Eur Radiol 1998;8:79-85.
- Murat A, Ozdemir H, Yildirim H, Kursad Poyraz A, Artas H. Bronchial atresia of the right lower lobe. Acta Radiol 2005;46:480-3.
- Gohil H, Muthukrishnan A. Bronchial atresia on FDG PET/CT: imaging characteristics of a rare pulmonary pseudonodule. Clin Nucl Med 2012;37:86-7.
- Mori M, Kidogawa H, Moritaka T, Ueda N, Furuya K, Shigematsu S. Bronchial atresia: report of a case and review of the literature. Surg Today 1993;23:449-54.
Yazışma Adresi (Address for Correspondence)
Dr. Melike DEMİR
Dicle ?niversitesi Tıp Fak?ltesi,
G?ğ?s Hastalıkları Anabilim Dalı,
Diyarbakır - T?rkiye
e-mail: melikedoktor@hotmail.com
Geliş Tarihi/Received: 11.03.2016 ? Kabul Ediliş Tarihi/Accepted: 19.06.2016