LETTER TO THE EDITOR
Doi: 10.5578/tt.24111
Tuberk Toraks 2017;65(3):255-257

Successfully chest irradiation for an advanced squamous
cell lung cancer patient with predialysis renal insufficiency
Tomohiro TAMURA1, Gen OHARA1, Katsunori KAGOHASHI1, Hiroaki SATOH1
1 Division of Respiratory, Mito Medical Center, Tsukuba University, Mito, Japan
1 Tsukuba ?niversitesi Mito Tıp Merkezi, Solunum B?l?m?, Mito, Japonya
Thoracic irradiation is one of the treatment choices for advanced squamous cell lung cancer patients having comorbid disease that cannot be tolerable of chemotherapy (1). We present a patient with squamous cell carcinoma undergoing chest irradiation who had unexpected improvement of renal function one year after the therapy.
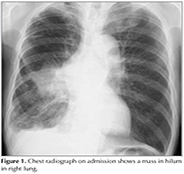
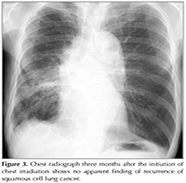
A mass was detected in a 64-year-old man with haemodialysis independent renal impairment undergoing a routine chest X-Ray (Figure 1). Thirteen years ago, the patient had renal biopsy for the correct diagnosis of nephrotic syndrome, and diagnosed as having IgA nephropathy. He treated the disease with prednisolone for ten years. The patient had cough and dyspnea on effort for three months. He smoked one pack-year for 25 years. Chest computed tomography revealed a mass in the right lung with ipsilateral mediastinal lymphadenopathy. There was small amount of pleural fluid in the right hemithorax, which was evaluated as a malignant pleural fluid clinically (Figure 1). Laboratory testing revealed blood ureanitrogen (BUN) 46.0 mg/dL and creatinine (Cre) 2.86 mg/dL. Histopathological analysis obtained by transbronchial biopsy showed squamous cell cancer (Figure 2). A brain computed tomography, abdominal echogram and bone scintigram revealed nodistant metastasis. Due to his impaired renal function, the patient received thoracic irradiation (2 Gy/day, total 50 Gy). He had no additional chemotherapy. On chest radiograph and CT scan three months after the initiation of chest irradiation, volume loss of the right lung due to post-irradiation change was observed, but no apparent finding of recurrence of squamous cell lung cancer was found (Figure 3). During the follow-up period, the patient developed pneumonia twice and herpes zoster in his left back. At these times, his renal function was tentatively deteriorated with BUN 83.0 mg/dL and Cre 5.35 mg/dlL. Fortunately, however, his renal function unexpectedly returned to the revel with BUN 25.0 mg/dL and Cre 2.07 mg/dL 15 months after the thoracic irradiation for the tumor. The patient is now followed up in our outpatient office.
It is not apparent whether there is relationship between this medical history and the development of lung cancer. Some previous researchers reported cases with nephrotic syndrome due to IgA-nephropathy and lung cancer (2-6). In patients with membranaous nephropathy, lung cancer developed in several years later (7-10). Polenakovic and Grcevska reported a patient with bronchial adenocarcinoma 11 years after the onset of membranous nephropathy (7). Our patient had renal biopsy for the correct diagnosis of nephrotic syndrome, and diagnosed as having IgA nephropathy 13 years before the development of lung cancer associated with chlorambucil therapy. As the present case was treated with corticosteroid for ten years before the development of lung cancer, it is possible that there was a certain relationship between the preceding renal disease and lung cancer. In addition, the possibility that long-term prednisolone therapy accelerated the development of lung cancer cannot be excluded.
There have been reports which showed effective treatment for advanced lung cancer patients undergoing hemodialysis (11-13). However, no case report has been reported about successful treatment for advanced lung cancer patients with renal impairment, who had not received hemodialysis yet. Therefore, the recommended therapy for such patients is not established. This case presents two aspects of special interest. One, in spite of the advanced squamous lung cancer of the patient, a long-term survival more than one year was achieved by thoracic irradiation alone. It is controversial whether chest irradiation is indicative for lung cancer patients with pleural fluid. Majority of medical oncologists insist that the therapy is not indicative because it is only a local therapy. On the other hand, however, chest physicians select the therapy as palliative one because it may be effective for local control of the disease in order to prevent obstruction of trachea and main bronchus even the patients had pleural fluid. Our patient had both narrowing of the right main bronchus and pleural fluid in the hemithorax. To prevent obstruction of the airway, we performed chest irradiation with its field only including the main tumor and ipsilateral mediastinal lymph nodes.Cancer cells were not found in cytological specimens from pleural fluid. Considering this good clinical course, it was possible that pleural fluid was not due to cartinomatous pleuritis but only a reactive pleural fluid as a result of impairment of ipsilateral hilar bloodstream. There is another interesting point. Improvement of renal function was obtained after the long-term follow up of the disease. Precise mechanism is unknown. One explanation might be that a decrease in quantity of total body muscle occurred because of cachexy with the progression of lung cancer, and, as a result, serum values in BUN and creatinine might decrease. Renal impairment due to paraneoplastic syndrome might be considered as other possibility. Although the relationship is beyond our knowledge, it is interesting that our patient suffered nephritic syndrome almost 10 years before the development of symptoms due to lung cancer.
We show herein anadvanced squamous lung cancer patient with impairment of renal function treated only with thoracic irradiation had survival more than one year. The patient showed decreased serum BUN and creatinine levels.? Precise mechanism is unknown, but we do believe that this is an important case that gave some suggestion for the treatment of the advanced lung cancer with same situation.
REFERENCES
- Smith SL, Palma D, Parhar T, Alexander CS, Wai ES. Inoperable early stage non-small cell lung cancer: comorbidity, patterns of care and survival. Lung Cancer 2011;72:39-44.
- Masutani K, Fujisaki K, Maeda H, Toyonaga J, Inoshima I, Takayama K, et al. Tubulointerstitial nephritis and IgA nephropathy in a patient with advanced lung cancer treated with long-term gefitinib. Clin Exp Nephrol 2008;12:398-402.
- Tomoda K, Hamada K, Fukuoka K, Tsukaguchi K, Tsujimoto M, Mikasa K, et al. Small cell lung cancer associated with nephrotic syndrome: remission after chemotherapy. Nihon Kokyuki Gakkai Zasshi 1998;36:541-4.
- Yacoub G, Kosseifi SG, Shah LS, Byrd RP Jr, Roy TM. IgA nephropathy and small cell lung carcinoma. Tenn Med 2008;101:35-7, 40.
- Sch?tte W, Ohlmann K, Koall W, R?sch B, Osten B. Paraneoplastic IgA nephritis as the initial symptom of bronchial carcinoma. Pneumologie 1996;50:494-5.
- Mustonen J, Helin H, Pasternack A. IgA nephropathy associated with bronchial small-cell carcinoma. Am J Clin Pathol 1981;76:652-6.
- Polenakovic M, Grcevska L. Development of bronchial adenocarcinoma 11 years after the onset of membranous nephropathy associated with chlorambucil therapy. Nephron 1995;69:335-6.
- Moorthy AV. Minimal change glomerular disease: a paraneoplastic syndrome in two patients with bronchogenic carcinoma. Am J Kidney Dis 1983;3:58-62.
- Burstein DM, Korbet SM, Schwartz MM. Membranous glomerulonephritisand malignancy. Am J Kidney Dis 1993:22:5-10.
- Ohara G, Satoh H, Kurishima K, Ohtsuka M, Hizawa N. Paraneoplastic nephrotic syndrome in patients with lung cancer.Intern Med 2009;48:1817-20.
- Inoue A, Saijo Y, Kikuchi T, Gomi K, Suzuki T, Maemondo M, et al. Pharmacokinetic analysis of combination chemotherapy with carboplatin and etoposide in small-cell lung cancer patients undergoing hemodialysis. Ann Oncol 2004;15:51-4.
- Haraguchi N, Satoh H, Ogawa R, Hashimoto Y, Sekizawa K. Chemotherapy in a patient with small-cell lung cancer undergoing haemodialysis. Clin Oncol (R Coll Radiol) 2005;17:663.
- Oguri T, Shimokata T, Inada M, lto I, Ando Y, Sasaki Y, et al. Pharmacokinetic analysis of carboplatin in patients with cancer who are undergoing hemodialysis. Cancer Chemother Pharmacol 2010;66:813-7.
Yazışma Adresi (Address for Correspondence)
Dr. Hiroaki SATOH
University of Tsukuba, Division of Respiratory Medicine,
Mito Medical Center,
Mito - Japan
e-mail: hirosato@md.tsukuba.ac.jp
Geliş Tarihi/Received: 08.03.2016 - Kabul Ediliş Tarihi/Accepted: 19.06.2016