RESEARCH ARTICLE
Doi: 10.5578/tt.53938
Tuberk Toraks 2017;65(1):1-8

Organize pn?monili olguların retrospektif değerlendirilmesi:
Kriptojenik organize pn?moni sekonder organize pn?moniden farklı mıdır?
Saliha YILMAZ1, Berna AKINCI ?ZY?REK1, Yurdanur ERDOĞAN1, Burcu CİRİT KO?ER1, Funda DEMİRAĞ2,
Yeliz DADALI3, Serta? B?Y?KYAYLACI ?ZDEN1
1 Clinic of Chest Diseases, Ankara Ataturk Chest Diseases and Chest Surgery Training and Research Hospital,
Ankara, Turkey
1 Ankara Atat?rk G?ğ?s Hastalıkları ve G?ğ?s Cerrahisi Eğitim ve Araştırma Hastanesi, G?ğ?s Hastalıkları Kliniği,
Ankara, T?rkiye
2 Clinic of Pathology, Ankara Ataturk Chest Diseases and Chest Surgery Training and Research Hospital, Ankara, Turkey
2 Ankara Atat?rk G?ğ?s Hastalıkları ve G?ğ?s Cerrahisi Eğitim ve Araştırma Hastanesi, Patoloji Kliniği, Ankara, T?rkiye
3 Division of Radiology, Ahi Evran University Training and Research Hospital, Kirsehir, Turkey
3 Ahi Evran ?niversitesi Eğitim ve Araştırma Hastanesi, Radyoloji B?l?m?, Kırşehir, T?rkiye
?ZET
Organize pn?monili olguların retrospektif değerlendirilmesi: Kriptojenik organize pn?moni sekonder organize pn?moniden farklı mıdır?
Giriş: Organize pn?moni (OP) akciğer hastalıkları i?erisinde nadir g?r?len klinik opatolojik bir durumdur. Ger?ek insidansı ve prevalansı bilinmemektedir. Altta yatan hastalık ya da neden belli değilse kriptojenik organize pn?moni (KOP) olarak adlandırılır. Bu ?alışmamızda son 10 yılda hastanemizde tanı alan organize pn?moni olgularının retrospektif olarak, etyolojik ve klinik ?zelliklerinin değerlendirilmesi ve kriptojenik ve sekonder OP hastalarının birbiri ile karşılaştırılması ama?lanmıştır.
Materyal ve Metod: Bu ?alışmaya Ağustos 2003-Ağustos 2013 tarihleri arasında patolojik doku tanısı OP gelen 165 hasta dahil edildi. Hasta bilgileri retrospektif olarak hastane dosyalarından incelendi.
Bulgular: ?alışmaya patolojik olarak OP tanısı konulmuş 165 hasta dahil edildi. Hastaların 89 (%53.9)'una transtorasik ince iğne aspirasyon biyopsisi (TTİAB), 52 (%31.5)'sine cerrahi y?ntemle (lobektomi, wedge rezeksiyon, segmentektomi), 24 (%14.5)' ?ne transbronşiyal biyopsi (TBB) ile tanı konulmuştu. 100 (%60.6) hastanın KOP, 65 (%39.4) hastanın da sekonder OP olduğu belirlendi. En yaygın g?r?len semptomlar; ?ks?r?k, halsizlik, dispne idi. Elli beş (%44.7) hastada restriktif, 26 (%21.2) hastada obstr?ktif solunum fonksiyon bozukluğuna rastlandı. ?alışmamızda sekonder organize pn?moniye sebep olan bilinen etyolojik ajanlara ek olarak antrokozise ve kist hidatiğe bağlı olarak gelişen organize pn?moni olguları saptadık. Altmış dokuz hastada OP'un tipik radyolojik g?r?n?m? olan yamalı vasıfta bilateral multipl opasiteler, 76 hastada fokal lezyonlar (solid kitle, kaviter kitle), 6 hastada da infiltratif opasiteler izlendi.
Sonu?: OP'un kriptojenik ve sekonder formlarında OP'a ilişkin klinik, radyolojik ve laboratuvar ?zellikler a?ısından fark yoktur. ?lkemizde sekonder OP tanısı konulan hastalarda, etyolojide kist hidatik ve antrokoziste akılda tutulmalıdır.
Anahtar kelimeler: Organize pn?moni, antrakozis, kist hidatik, kriptojenik organize pn?moni
SUMMARY
Retrospective evaluation of patients with organizing pneumonia: is cryptogenic organizing pneumonia different from secondary organizing pneumonia?
Introduction: Organizing pneumonia (OP) is an uncommon clinic opathological situation among lung diseases. If no underlying cause can be detected, it is named as cryptogenic OP (COP). In this study, the etiologic and clinical characteristics of patients diagnosed as OP in our hospital in the last ten years were evaluated retrospectively. It was also aimed to make a comparison between COP and secondary OP patients.
Materials and Methods: One hundred sixty-five patients diagnosed as OP pathologically in the 10 year period from August 2003 to August 2013 were included into that study. Patients' data were evaluated retrospectively from the medical records.
Results: One hundred sixty five patients pathologically diagnosed as OP were included. Diagnostic methods were trans-thoracic fine-needle biopsy (TTFNB) in 89 (53.9%) patients, open lung biopsy (lobectomy, wedge resection, segmentectomy) in 52 (31.5%) patients and transbronchial biyopsy (TBB) in 24 (14.5%) patients. One hundred (60.6%) of the patients were defined as COP and 65 (39.4%) as secondary OP. Cough, fatigue and dyspnea were the most common symptoms on admission. We detected OP cases secondary to anthracosis and cyst hydatic besides other well known etiologies. In 61 patients, the main radiologic manifestation was multiple bilateral patchy consolidation typical for OP. In 76 patients focal lesions (solid mass, cavitating mass lesion) and in 6 patients infiltrative opacities were detected radiologically.
Conclusion: There is no difference between properties of OP from clinical, laboratory and radiologic finding sin the criptogenic and seconder form of OP. Although it is not asserted, cyst hidatic and anthracosis could be kept in mind for the list of underlying ethiologies for secondary OP.
Key words: Organizing pneumonia, anthracosis, cyst hydatic, cryptogenic organizing pneumonia
Geliş Tarihi/Received: 24.04.2016 • Kabul Ediliş Tarihi/Accepted: 31.03.2017
INTRODUCTION
Organizing pneumonia (OP) is an histopatologic entity characterized by granulation tissue plugs (Masson bodies) formed by fibroblasts, miyofibroblasts, collagen and fibrinated exudate within respiratory bronchioles, alveolar ducts and alveoli. Once OP is defined pathologically, underlying cause must be investigated. OP is classified as primary (cryptogenic-COP) or secondary OP. The OP caused by infections, connective-tissue disorders, malignancies, drugs, inflammatory bowel diseases, solid organ transplantations, radiotherapy, aspiration, etc. is defined as secondary OP. After a detailed examination, if no underlying reason or disease is detected, the diagnosis of COP is made.
Clinical manifestations are similar in both situations. Symptoms are usually non-specific. Cough, dyspnea, weight loss, chills, sweating, fever and myalgia is common. Occasionally hemoptysis is occurred. The onset of symptoms is usually less than 3 months. Men and women are equally affected. The patients are usually aged between 50-60 years. It is rarely seen in children.
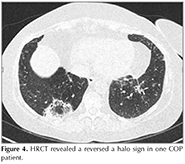
Three main radiologic patterns distinguished in OP are typical, solitary-focal and infiltrative forms. Multiple masses nodules, cavitating nodules, bronchocentric consolidation, band-like opacities, perilobuler opacities, reversed halo sign, pneumatocele and pleurisy are other radiographic appearances.
In this study, we aimed to evaluate the etiologic, clinical and radiologic properties of the patients diagnosed as OP in the last 10 years in our hospital and compare the clinical and radiologic properties between COP and secondary OP patients.
MATERIALS and METHODS
One hundred sixty-five patients diagnosed as OP pathologically in the 10 year period from August 2003 to August 2013 were included in this study. Patient information was retrospectively evaluated from the medical records. Approve from the Hospital Ethic Commission was obtained. Each patients hemogram; hemoglobin (Hb), leucocyte count, eosinophil count, platelet count, biochemical markers; C-reactive protein (CRP), alkaline phospatase (ALP), gamma glutamyl transferase (GGT), connective tissue markers, p-ANCA, c-ANCA, ANA, anti ds-DNA, RF, CCP, anti SS-A, anti SS-B results were recorded. HRCT scans at time of diagnosis were re-evaluated. Radiologically OP diagnosis was reported as typical (bilateral patchy infiltrations with air bronchograms), focal (solid mass, cavitating mass), infiltrative and other (multiple nodules, band formation and reversed halo sign). Since patient information was retrospectively evaluated from the medical records, we were not able to obtain enough data concerning treatment and follow-up period.
Statistical analysis was carried out with Statistical Package for the Social Sciences (SPSS) for Windows (version 18.0, Chicago, IL, USA). Non-parametric Mann-Whitney U and chi-square tests, and parametric Student's t tests were performed. p values less than 0.05 were considered as statistically significant.
RESULTS
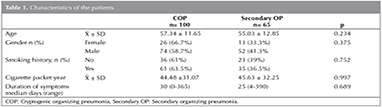
Data from 165 patients pathologically diagnosed as OP were evaluated. The mean age of the patients was 56.4 ? 12.15 years. The mean age of COP and secondary OP patients was 57.34 ? 11.65 and 55.03 ? 12.85 respectively. There were 39 (23.6%) female patients and 126 (76.4%) male patients. Ninety six (61.9%) patients had smoking history. Mean duration of smoking was calculated as 44.9 ? 31.34 packet year. Characteristics of the patients wegivenin Table 1. The laboratory and clinical findings of 7 patients were missing. Fifty-three (39%) of the patients had asbestosis exposure and 51 (37.5%) had biomass exposure. No statistically significant difference has been detected between COP and secondary OP groups according to those features.
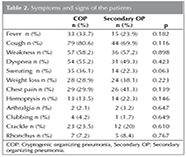
The median time for onset of symptoms was 30 days; 30 days and 25 days in the COP and secondary OP groups, respectively. No statistically significant difference was found between the groups. The most common symptoms seen on admission was cough, fatigue, dyspnea, fever, weight loss. Hemoptysis and arthralgia were less common. In COP group, symptoms were seen more frequently when compared with the secondary OP group but the difference was not statistically significant (Table 2).
Eighty-nine (53.9%) patients were diagnosed by transthoracic fine needle biopsy (TTFNB), 52 (31.5%) by open lung biopsy (lobectomy, wedge resection, segmentectomy) and 24 (14.5%) by transbronchial biopsy (TBB). One hundred (60.6%) of the patients were defined as COP and 65 (39.4%) as secondary OP.
In secondary OP patients, malignancies, infections, anthracosis, connective tissue diseases, hypersensitivity pneumonitis, aspiration pneumonia and radiotherapy were the accompanying conditions suggested to play a role in etiology. The distribution of etiologic factors were given in Table 3.
In physical examination, the oscultation was revealed cracklesin 35 (22.2%) patients, rhonchus in 12 (7.6%) patients, and 14(8.9%) patients had hypoxemia measured via pulse oximeter (plusMED Pulse Oximeter, model: plus-50 DL).
Pulmonary function test (PFT) results were available for 125 of 165 patients. In 42 patients (34.1%), the PFT results were in normal limits. In 55 (44.7%) patients, restrictive pattern and in 26 (21.2%) patients, obstructive pattern was observed. The 92.3% of the patients with obstructive pattern had smoking history. For 27 patients, lung diffusing capacity for carbon monoxide (DLco) measurement records could be reached. The results were as decreased in 18 (66.7%) and as normal in 9 (33%) .
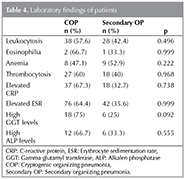
Leucocytosis (leucocyte count > 10.000/mL) was detected in 66 (40.5%); anemia (hemoglobin < 12 g/dL) in 17 (10.4%) and peripheral eosinophilia (eosinophil count > 700/mL) in 3 (1.8 %) patients. No statistically significant difference has been detected between the groups for laboratory results. The patients laboratory results were shown in Table 4. Fifty-one patients had auto-antibody test results; in only 1 patient c-ANCA positivity was detected. For this patient, Wegener granulomatosis was defined as underlying reason for secondary OP.
In 83.4% of the patients who underwent fiberoptic bronchoscopy (FOB), no abnormality was detected. In 9 (6.7%) patients, anthracosis, in 8 (6%) increased in secretion, in 5 (3.7%) endobronchial lesion (EBL) was observed. The pathologic examination of the biopsies from EBL revealed both malignancy and OP. In these patients, lung malignancy was accepted as secondary OP reason.
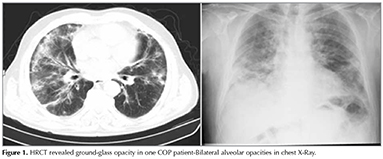
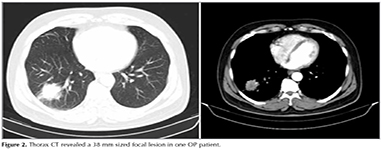
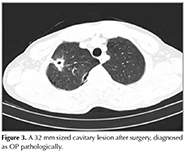
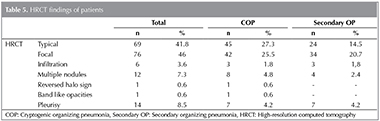
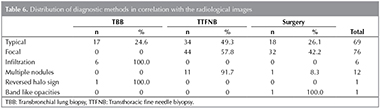
In HRCT scans; 69 (41.8%) patients had the typical multiple patchy bilateral opacities, 76 (46%) had focal lesions (solid mass, cavitating mass) and 6 (3.6%) had infiltrative opacities (Figure 1, 2, 3). Other features of OP including multiple nodules (12 patients, 7.2%), band- like opacities (1 patient, 0.6%), reversed halo sign (1 patient, 0.6%) were also reportedon HRCT scans (Figure 4). Pleurisy was seen in 14 patients. Evaluation of COP and secondary OP patients according to their radiological patterns were givenin Table 5. Eighty-nine (53.9%) patients were diagnosed by TTFNB, 52 (31.5%) by open lung biopsy (lobectomy, wedge resection, segmentectomy) and 24 (14.5%) by TBB. Diagnostic methods according to the radiological appearance were given in Table 6.
DISCUSSION
Organizing pneumonia is a clinic opathological situation among lung diseases. The exact prevalance and incidence is still not known. If no underlying cause can be detected, it is named as cryptogenic (primary) OP (COP).
In our study, we defined anthracosis in 9 patients and cyst hydatic in 4 patients and suggested them assecondary OP reasons, besides other well known ethiologies. In the patients with anthracosis detected by FOB, we assume that OP might be secondary to obstruction or as a reaction to anthracosis. In the literature, there is no evidence about OP secondary to antracosis. Since Turkey is endemic for cyst hydatic, it should be kept in mind among secondary OP ethiology (3). In the study of Sakamato and Gutierrez, OP was one of the pulmonary complications seen among the pediatric cyst hydatic patients (ages between 1 and 15 years) (4).
In our study, 53 (39%) of the patients had asbestosis exposure and 51 (37.5%) had biomass exposure. There is no datarelated with biomass exposure in OP patients exceptone case report of OP secondary to asbestosis exposure (5). We suggest that biomass and asbestosis exposure could also be considered among secondary OP reasons.
OP patients are usually aged between 50-60 years (6,7). Men and women are equally affected. Smoking is not associated with OP (8). COP is seen more frequent in non-smokers and ex-smokers, especially in female patients (9). In contrast to the literature, our patients were predominantly (76.4%) male (10-13).Ninety-six of our patients (61.9%) had smoking history. There wasno difference on smoking history between COP and secondary OP groups, similar with the result in the study by Drakopanagiotakis et al. (1).
OP is a subacute disease. Onset of symptoms is usually less than 3 months (14). Since the median duration of symptoms prior to diagnosis was 30 days in our study, it might be said that ourpatients were diagnosed earlier.
Dry cough, fever, fatigue, and dyspnea are the most commonly seen symptoms. Hemoptysis, chest pain, arthralgia, night sweats are seen occasionally (14). Cough, fatigue and dyspnea were the most frequent symptoms in our patients. In our study, symptoms ashemoptysis, chest pain, night sweats were uncommon. Chest pain was present in 34.4% of our patients. In OP patients chest pain is expected to be seldom seen. In the study of Drakopanagiotakis et al.? and Oymak et al., chest pain had high percentage (1,11). In our study chest pain was found to be associated with pleurisy and nodules nearto pleura.
In physical examination of the lungs, inspiratory crackles can be heard in 74% of OP patients (15). Wheezing is uncommon. The rate of digital clubbing is less than 5% (16). Although there was no difference between the physical examination findings of COP and secondary OP patients; more findings (especially crackles) were present in COP patients. It might be because typical radiologic pattern of OP (multiple bilateral patchy opacities) was seen more frequent in COP patients.
Mild to moderate restrictive pattern is usually seen in OP patients and DLco is decreased (8,17). In 44.7% of our patients, restrictive pattern and in 21.2% of our patients, obstructive pattern was detected. Similar with the study of King et al. 92.3% of our patients with obstructive pattern had smoking history (12). DLco was decreased in 66.7% of the patients in whom the results could ve be reached. In 8.9% of our patients hypoxemia was present in whom extensive bilateral radiologic involvement was seen.
Radiologically there are 3 main types of images in OP: typical, focal and infiltrative (9,18). Although there was no statistically significant difference, typical patern was seen more frequently in COP patients when focal patern was seen in secondary OP patients more dominantly. Bronchosentric consolidation, band-like opacities, multiple nodules, multiple mass, perilobuler opacities, progressive fibrosis- reticulation and reversed halo sign are other seldomly seen radiological appearances (7). In our study, 12 patients had multiple nodules and one had band-like opacities and reversed halo sign. Pleurisy is seen occasionally (1). We detected pleurisy in 14 (8.5%) of our patients. In 9 ofthose patients, the etiology could not be detected and in 5 patients it was secondary to empyema or lung cancer.
No specific laboratory test is present for OP. Elevated erythrocyte sedimentation rate (ESR) and CRP is reported in 70-80% of patients (15,16). Eosinophilia is not an expected finding. In the follow up period, high ALT and GGT values were shown to be associated with relapses (19). In approximately 50% of patients, leucosytosis is reported (15). In our patients, similar to literature,elevated ESR, high CRP, and leucosytosis at the time of diagnosis was detected. In 3 patients, eosinophilia was present. Thrombocytosis, anemia, high GGT and ALP values were also present. Barosso et al. detected elevation in GGT in 10% and ALP in 13% of 33 COP patients; whereas Lazor et al. could not establish a relationship between relapses (19,20). In our study, we could not evaluate the relationship between relapses because of lack of sufficient follow-up.
The diagnosis of OP requires tissue diagnosis. Surgical procedures (open lung biopsies, VATS), TBB and TTFNB are used in diagnosis. Histopathologyare the gold standart in diagnosis (1). Diagnosis can be achieved by TBB in patients with typical radiological lesions and by TTFNB in those with focallesions. Larger samples can be obtained via TTFNB than TBB. Although it is more helpful in diagnosis, studies concerning TTFNB is limited (9). In our study, 89 patients were diagnosed by TTFNB, 52 by open lung biopsy, and 24 by TBB. In 70% of patients diagnosed by TBB typical radiological appearance was present while in 51% of those diagnosed by surgical procedures focal lesion was present. We suggest TTFNB as an alternative to surgery in patients with focal lesion and multiple nodular lesion.
In a retrospective studydone by Lohr et al., the authors have evaluated 74 pathologically proven OP patients, and no difference between COP and secondary OP patients could be detected clinically, radiologically or pathologically (21). In a study of 78 OP diagnosed patients by Cazzato et al. from Italy, COP was observed in 68% of the patients (22). No clinical or radiologic difference between COP and secondary OP patients was present. In our study, we evaluated 165 pathologically diagnosed OP patients. We detected that similarly the study of Oymak et al., 100 (60.6%) of these were COP (11). There was no radiologic or clinical differences between the two groups similar with literature.
A few limitations should be noted as follow up results and treatment options were not known in this retrospective study.
CONCLUSION
Cyst hidatic and anthracosis should be kept in mind in OP ethiology. Moreover, asbestosis and biomass exposure should be questioned.
Comorbid diseases, medication and operation history and? symptoms should be? questioned by all means for discrimination between COP and secondary OP.
Although there isno difference between properties of OP from clinical, laboratory and radiologic findings in the criptogenic and seconder form of OP that patients with COP are more symptomatic.
Radiologically, typical? pattern dominance is seen in COP patients rather than secondary OP patients. Leucocytosis and elevated CRP is seen more often in COP patients. In patients with no response to nonspecific antibiotherapy, those who have no patognomonic findings for alternative diagnosis and who have multiple nodules and focal lesions on thorax CT; TTFNB can be used as an alternative diagnostic tool to surgery for OP diagnosis.
ETHICS COMMITTEE APPROVAL
Ethics committee approval was received for this study from the ethics committee of Atat?rk Chest Diseases and Chest Surgery Training and Research Hospital.
CONFLICT of INTEREST
No conflict of interest was declared by the authors.
FINANCIAL DISCLOSURE
The authors declared that this study has received no financial support.
REFERENCES
- Drakopanagiotakis F, Paschalaki K, Abu-Hijleh M, Aswad B, Karagianidis N, Kastanakis E, et al. Cryptogenic and secondary organizing pneumonia clinical presentation, radiographic findings, treatment response, and prognosis. Chest 2011:139:893-900.
- Maldonado F, Daniels CE, Hoffman EA, Yi ES, Ryu JH. Focal organizing pneumonia on surgical lungbiopsy: causes, clinico radiologic features, and outcomes. Chest 2007;132:1579-83.
- Craig PS, Manus DP, Lightowlers MW, Chabalgoity JA, Garcia HH, Gavidia CM, et al. Preventionand control of cystic echinococcosis. Lancet Infect Dis 2007;7:385-94.
- Sakamoto T, Gutierrez C. Pulmonary complications of cystic echinococcosis in children Urguay. Pathol Int 2005;55:497-503.
- Cavazza A, Nigrisoli E, De Marco L, Paci M, Annessi V, Agostini L, et al. Bronchiolitis obliterans-organizing pneumonia (BOOP) containing asbestos bodies: clinico-pathological study of a case. Pathologica 2001;93:681-4.
- Vasu TS, Cavallazzi R, Hirani A, Sharma D, Weibel SB, Kane GC. Clinical and radiologic distinctions between secondary bronchiolitis obliterans organizing pneumonia and cryptogenic organizing pneumonia. Respir Care 2009;54:1028-32.
- Epler GR. Bronchiolitis obliterans organizing pneumonia: definition and clinical features. Chest 1992;102(Suppl):S2-6.
- Alasaly K, Muller N, Ostrow DN, Champion P, FitzGerald JM. Cryptogenic organizing pneumonia. A report of 25 cases and a review of the literature. Medicine (Baltimore) 1995;74:201-11.
- Cottin V, Cordier JF. Cryptogenic organizing pneumonia. Semin Respir Crit Care Med 2012;33:462-75.
- Gul A, Yilmazbayhan D, Buyukbabani N, Lie JT, Tunaci M, Tunaci A, et al. Organizing pneumonia associated with pulmonary artery aneurysms in Behcet's disease. Rheumatology (Oxford) 1999;38:1285-9.
- Oymak FS, Demirbaş HM, Mavili E, Akgun H, Gulmez I, Demir R, et al. Bronchiolitis obliterans organizing pneumonia. Clinical and roentgenological features in 26 cases. Respiration 2005;72:254-62.
- King TE Jr, Mortenson RL. Cryptogenic organizing pneumonitis. The North American experience. Chest 1992;102(Suppl 1):S8-S13.
- Izumi T, Kitaichi M, Nishimura K, Nagai S. Bronchiolitis obliterans organizing pneumonia. Clinical features and differential diagnosis. Chest 1992;102:715-9.
- Travis W, Costabel U, Hansell DM, King TE, Lynch DA, Nicholson AG, et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med 2013;188:733-48.
- King TE Jr. Organizing pneumonia. In: Interstitial lung disease, 5, Schwarz MI, King TE Jr. (Eds), People's Medical Publishing House, Shelton CT 2011;981.
- Cordier J. Cryptogenic organizing pneumonitis. Bronchiolitis obliterans organizing pneumonia. Clin Chest Med 1993;14: 677-92.
- Cordier JF. Organising pneumonia. Thorax 2000;55:318-28.
- Erdoğan Y, Ozyurek BA, Ozmen O, Demirci NY, Duyar SS, Dadalı Y, et al. The evaluation of FDG PET/CT scan findings in patients with organizing pneumonia mimicking lung cancer. Molecular Imaging and Radionuclide Therapy 2015;24:60-5.
- Lazor R, Vandevenne A, Pelletier A, Leclerc P, Court-Fortune I, Cordier JF. Cryptogenic organizing pneumonia. Characteristics of relapses in a series of 48 patients. The Groupe d'Etudes et de Recherche sur les Maladles "Orphelines" Pulmonaires (GERM"O"P). Am J Respir Crit Care Med 2000;162:571-7.
- Barroso E, Hernandez L, Gil J, Garcia R, Aranda I, Romero S. Idiopathic organizing pneumonia: a relapsing disease. 19 years of experience in a hospital setting. Respiration 2007;74:624-31.
- Lohr RH, Boland BJ, Douglas WW, Dockrell DH, Colby TV, Swensen SJ, et al. Organizing pneumonia. Features and prognosis of cryptogenic, secondary, and focal variants. Arch Intern Med 1997;157:1323-9.
- Cazzato S, Zompatori M, Baruzzi G, Schiattone ML, Burzi M, Rossi A, et al. Bronchiolitis obliterans-organizing pneumonia: an Italian experience. Respir Med 2000;94:702-8.
Yazışma Adresi (Address for Correspondence)
Dr. Berna AKINCI ?ZY?REK
Ankara Atat?rk G?ğ?s Hastalıkları ve
G?ğ?s Cerrahisi Eğitim ve Araştırma Hastanesi,
G?ğ?s Hastalıkları Kliniği,
ANKARA - TURKEY
e-mail: drberna_1982@yahoo.com