REVIEW
Doi: 10.5578/tt.2245
Tuberk Toraks 2016;64(4):289-298

Kronik obstr?ktif akciğer hastalığında komorbiditelerin hastalık ?zerine etkileri
Neşe DURSUNOĞLU1, Nurdan K?KT?RK2, Ayşe BAHA3, Ahmet Kaya BİLGE4, Şermin B?REK?İ5, Fatma ?İFT?İ6,
Makbule GEZMEN KARADAĞ7, Ebru ?ALIK K?T?K??8, Ayşın NOYAN9, Mehmet POLATLI10, Zeynep Pınar ?NEN6,
Sevin? SARIN?11, Sema UMUT5, Esra UZASLAN12, Ayşe KUBAT ?Z?M13, ?znur AKKOCA YILDIZ6,
Turkish Thoracic Society- COPD Comorbidity Group
1 Department of Chest Diseases, Faculty of Medicine, Pamukkale University, Denizli, Turkey
2 Department of Chest Diseases, Faculty of Medicine, Gazi University, Ankara, Turkey
3 Department of Chest Diseases, Faculty of Medicine, Ufuk University, Ankara, Turkey
4 Department of Cardiology, Faculty of Istanbul Medicine, Istanbul University, Istanbul, Turkey
5 Department of Chest Diseases, Faculty of Istanbul Medicine, Istanbul University, Istanbul, Turkey
6 Department of Chest Diseases, Faculty of Medicine, Ankara University, Ankara, Turkey
7 Department of Nutrition, Faculty of Medicine, Gazi University, Ankara, Turkey
8 Department of Physical Therapy, Faculty of Medicine, Hacettepe University, Ankara, Turkey
9 Department of Phyciatry, Faculty of Medicine, Ege University, Izmir, Turkey
10 Department of Chest Diseases, Faculty of Medicine, Adnan Menderes University, Aydin, Turkey
11 Department of Chest Diseases, Faculty of Medicine, Hacettepe University, Ankara, Turkey
12 Department of Chest Diseases, Faculty of Medicine, Uludag University, Bursa, Turkey
13 Department of Internal Medicine, Faculty of Istanbul Medicine, Istanbul University, Istanbul, Turkey
?ZET
Kronik obstr?ktif akciğer hastalığında komorbiditelerin hastalık ?zerine etkileri
Kronik obstr?ktif akciğer hastalığı (KOAH), akciğer etkilenimi ve ?eşitli komorbidetelerden kaynaklanan yıkıcı sonu?ları olan kompleks bir hastalıktır. Komorbiditeler, semptomları, yaşam kalitesini, komplikasyonları, hastalığın y?netimini, ekonomik y?k?n? ve mortalitesini etkilemektedir. Komorbiditelerin ?nemi, KOAH'ın sonu?ları ?zerine olan etkilerinden kaynaklanmaktadır. KOAH'ta g?r?len en sık komorbiditeler, kardiyovask?ler, endokrinolojik, m?sk?loskeletal ve psikolojik olanlar ve akciğer kanseridir. KOAH olgularının en az %50'sinde ?? veya daha fazla komorbidite bulunmaktadır. Yeni GOLD kılavuzu komorbiditelerin proaktif olarak araştırılmasını ve tedavisini ?nermektedir. Ancak bu komorbiditelerin aktif tedavisinin, KOAH'ın sonu?larını etkilediğine dair kesin bir kanıt yoktur. ?te yandan kardiyovask?ler hastalıklar ve akciğer kanseri gibi komorbiditeler, KOAH mortalitesi ?zerinde ?nemli etkiye sahiptir. ?eşitli ?alışmalar, Charlson komorbidite indeksinin veya KAOH spesifik komorbidite indeksinin (COTE) KOAH mortalitesi ile ilişkili olduğunu g?stermiştir. Bu kısa derleme, KOAH ?zerindeki etkileri ile beraber en sık g?r?len komorbiditeleri ?zetlemeyi ama?lamıştır.
Anahtar kelimeler: KOAH, komorbidite
SUMMARY
Comorbidities and their impact on chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a complex disease that is associated with devastating outcomes resulting from lung involvement and several comorbidities. Comorbidities could impact on symptomology, quality of life, the complications, the management, economic burden and the mortality of the disease. The importance of comorbidities originates from their impact on the outcome of COPD. The most frequent comorbidities in COPD are cardiovascular, endocrinological, musculoskeletal, phycological disorders and lung cancer. Almost 50% of the COPD patients have 3 or more comorbidities. The recent Global Initiative of Obstructive Lung Disease (GOLD) Guideline suggested proactive search and the treatment of the comorbidities. However, there is no certain evidence demonstrating that active treatment of comorbidities improve the outcomes of COPD. However, it is well known that several comorbidities such as cardiovascular disease and lung cancer have greater impact on mortality caused by COPD. Several studies have shown that Charlson Comorbidity index or more recenty COPD Specific Comorbidity Index (COTE) has been found to be related with mortality of COPD. This concise review intended to summarize the most frequent comorbidities in association with their impact on COPD.
Key words: COPD, comorbidity
Geliş Tarihi/Received: 18.02.2016 • Kabul Ediliş Tarihi/Accepted: 14.05.2016
INTRODUCTION
COPD is a complex disease that is associated with devastating outcomes resulting from lung involvement and several comorbidities (1,2). The medical dictionaries describe comorbidity as "the coexistence of concomitant but pathologically unrelated diseases". In practice the term of comorbidity is used for the coexistence of two or more diseases regardless of the pathogenic interlink". COPD has greater number (3.7) of comorbidities than non COPD subjects (1.8) (3-5). Studies showed that 94% of COPD patients had at least one comorbidity and up to 46% had three or more (3). The common etiological factors such as smoking, aging and reduced physical activities or shared inflammatory pathways can be the explanation of that relationship (1-3). The importance of comorbidities originates from their impact on the outcome of COPD. Comorbidities could cause additional impairment of patient's health quality of life, morbidity, health economy and mortality (1,3,6).
Gastroesophagial reflux disease (GERD), depression, anxiety, cardiovascular disease, and pulmonary embolism are associated with increased number of COPD exacerbations (6,7). The impact of comorbidities in exacerbations whether they mimic exacerbations or they precipitate the intensity of exacerbation is still a matter of debate (6). Comorbidities related with COPD Specific Comorbidiy Test (COTE) index revealed an increased risk of mortality (2.2 fold) (8). Toward a Revolution in COPD Health (TORCH) and Understanding Potential Long-term Impacts on Function with Tiotropium (UPLIFT) studies showed the almost 70% of causes of deaths in COPD were non-respiratory and the major non-respiratory etiology of mortality was cancer and cardiovascular diseases particularly in mild to moderate disease (9,10). Recent guidelines recommend actively searching and effectively treating common comorbidities (1.) However, there is no enough evidence to suggest that treatment of COPD would reduce comorbidities, the treatment of comorbidities improves COPD and, that the presence of COPD alters the treatment modalities of comorbidities. The best suggested approach in reduction of comorbidities in COPD is reduction of common risk factors such as smoking, obesity and physical inactivity (Table 1).
COPD and RESPIRATORY SYSTEM?
ACOPD can coexist with several respiratory disorders. Asthma, bronchiectasis, lung cancer and pulmonary fibrosis are among them.?
Asthma
Distinguishing asthma from COPD could be problematic in adult patients especially in smokers. (11). Physician diagnosed Asthma COPD Overlap Syndrome (ACOS) has a prevalence of 20% of patients with obstructive lung diseases (asthma or COPD). The coexistence of both diseases has worse outcome then either disease alone. Those patients should not be put on either LABA or LAMA alone and inhaled steroids should be placed besides the bronchodilator therapy (11).
Lung Cancer
Ageing, smoking, family history and host susceptibility have been identified as key risk factors for both COPD and lung cancer (12). Several large scale studies showed that emphysema and airflow obstruction increased the risk of lung cancer (Hazard Ratio: 2.8) (12-14). COPD has been found to coexistin 9% to 50% of lung cancer population (8,15). Lung cancer can be found incidentally in COPD patients while dealing with obstructive pneumonia or untractable COPD exacerbation. Lung cancer is a major comorbidity that can cause mortality in COPD patients (16). COPD may limit the chance of surgery in patients with lung cancer while increasing postoperative complications and finally increasing the likelihood of mortality due to COPD complications (3,6,17).
Lung Cancer Screening has been reccommended in several guidelines. According to the National Lung Screening Trial, (NLST) current or former cigarette smokers within the past 15 years, 55 to 74 years of age, with at least 30 pack-years of smoking patients are the high risk criteria for the lung cancer. However, those criteria are still not sensitive enough and still can miss up to 39% of cancer patients. Therefore, several authors suggest adding emphysema to NLST is beneficial for improving detection rate (18).
Pulmonary Fibrosis
The combined apprearance of pulmonary fibrosis and empysema (CPFE) was first described in 2005 (19).? This phenomenon would be a different entity than simple gathering two smoking associated diseases (20). There is upper lobes emphysema and lower lobe fibrosis with low carbon monoxide diffusion capacity (DLCO) and high risk of pulmonary hypertension and lung carcinoma (19). The symptoms of CPFE are more likely to resemble IPF showing progressive dyspnea and dry cough (21). Paraseptal emphysema is typical for CPFE (19,21). It is currently unknown whether pirfenidone or nintedanib are efficacious in CPFE (21). Lung transplantation is the only therapeutic option (6).
COPD and ENDOCRINOLOGY and METABOLISM
Weight loss and muscle wasting are present in 20%-70% of COPD patients (22). Aging, malnutrition, inactivity, smoking, hypoxemia, hypercapnia, administration of glucocorticoids and chronic comorbidities are associated with downregulation of anabolic states (22). This results in decreased testesteron levels, diminished bone density and muscle mass. COPD can cause late onset hypogonadism. However, replacing testesteron is no clear indication in COPD (22). Studies showed that adrenal axis was also affected by COPD. The cortisol/DHEAS ratio was greater among patient with low muscle mass. However, there is no evidence that DHEA administration has a significant benefit in COPD (23-25).
Body Mass and COPD
Metabolic Syndrome and abdominal obesity is more prevalent in mild to moderate COPD (16-24%) than severe disease (6%) (26). In early COPD, obesity can induce cardiovascular mortality but in the late stages of disease, the cachexia takes place and associated with increased mortality (27).
Diabetes Mellitus
The prevalence of diabetes in patients with COPD is 10-18.7% (28). Glucose metabolism is more disturbed in COPD patients than non-COPD patients. Shared risk factors and common inflammatory pathophysiology could be reason behind that relation.? TNF-alpha, IL-6, IL-1B, CRP and fibrinogen are most studied. Advanced age, hereditary factors, smoking, low birth weight are the shared risk factors of both diabetes and COPD (29). DM can cause pulmonary microangiopathy that results in reduced diffusion capacity of carbon monoxide (30). Hence, DM can cause phrenic neuropathy that results in diaphragm dysfunction (29). DM is also associated with increased risk of infectious exacerbations relating increased morbidity and mortality (31). Hyperglicemia can induced by chronic systemic CS usage. DM can develop in 11% of those patients (32,33). There is evidence that particularly high dose inhaled steroids can increase the risk of type 2 diabetes and can worsen the glycemic control (33,34).
COPD and Vitamin D
Vitamin D hypovitaminosis is a common problem all over the world. There has been interest in a possible link between vitamin D hypovitaminosis and COPD pathogenesis, progression, exacerbations and associated comorbidities. The desired vitamin D level is above 30 ng/mL. Vitamin D deficiency is described as if the 25(OH) vitamin D level under 20 ng/mL. Insufficiency is between 20-29 ng/mL (35). COPD patients had significantly lower vitamin D levels when compared to controls (36). Low food intake, aging, staying indoors, increased vitamin D catabolism due to glucocorticosteroids, impaired activation by renal dysfunction, lower storage capacity in muscles or fat tissues due to wasting could be the etiology for vitamin D hypovitaminosis in COPD (36,37). Vitamin D deficiency is related with osteoporosis, muscle weakness, infection and cardiovascular events in COPD. Several studies showed that Vitamin D deficiency is related with COPD onset, COPD progression and exacerbation.
Direct sun exposure without sunscreen is needed for skin to produce Vitamin D3. The recent Endocrinology Guideline in vitamin D deficiency recommends that adults above age 50 require daily 600-800 IU vitamin D for bone and muscle health. However, in order to raise blood vitamin D level over 30 mg/dL 1500-2000 IU/d vitamin D will be needed (35).
COPD and MUSCULOSKELETAL DYSFUNCTIONS
Common musculoskeletal problems seen in patients with chronic obstructive pulmonary disease (COPD) are skeletal and respiratory muscle dysfunction, postural impairments, decreased flexibility and range of motion (38). Skeletal muscle dysfunction directly affects exercise performance, is associated with poor health status, and is an independent predictor of healthcare utilization and mortality (39,40).? Skeletal muscle weakness is characterized by reduced muscle strength, reduced muscle endurance and the presence of muscle fatigue (41). The quadriceps muscle weakness is a common feature in patients within all stages of COPD and reduced quadriceps strength is found to be a useful predictor for mortality in patients with COPD (42,43). Also, postural abnormalities seen in patients with COPD are important due to negative impact on respiration and both components should be assessed individually. Changes in body and respiratory mechanics and acute/chronic cervical, thoracic or costal joint pains may occur with postural deviations (38,44).
There are several risk factors in COPD that may contribute to skeletal muscle weakness. These include smoking, corticosteroids, hypoxia, hypercapnia, inflammation, oxidative stress, reduced daily physical activity, vitamin D deficiency, nutritional deficitis and age (45).
The estimated overall prevalence of skeletal muscle weakness in patients with COPD was shown to be 20%-30% (46,47).
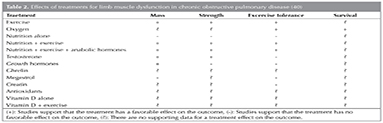
Management of musculoskeletal dysfunction in COPD patients, pharmacological (testosterone replacement therapy and vitamin D and calcium supplementation) and non-pharmacological (exercise training, prevention of falls and balance training and nutritional counseling) treatments are applied. (40,45). Their respective effects on limb muscles are summarized in Table 2.
COPD and OSTEOPOROSIS
Osteoporosis is defined a systemic disease by World Health Organization, characterized by a low bone mineral density and/or microarchitectural deterioration of bone tissue, leading to increased bone fragility and fracture risk (48). Osteoporosis prevalence increases with the severity of COPD (49-51).
Osteoporosis is common in both male and female patients with COPD (41). The prevalence of osteoporosis in COPD varies between 4% and 59%, depending on the diagnostic methods used and the severity of the COPD population (52). More than half of the patients with COPD recruited for the large TORCH trial had osteoporosis or osteopenia as determined by DEXA scan (53). Potential contributors to osteoporosis in COPD are corticosteroid use, inflammation, vitamin deficiency, anemia, smoking, and hypogonadism (41,43).
Prevention and treatment of osteoporosis involves both pharmacologic and nonpharmacologic interventions. Initially smoking cessation should be instituted into non-pharmacological interventions. Also overuse and overdose of ICS in COPD must be avoided (54). Pharmacological interventions consist of calcium and vitamin D supplementation and anti-resorptive therapy Oral or intravenous bisphosphanates are considered as the first line treatment for osteoporosis together with vitamin D and calcium supplementation. Also teriparatide and denosumab are the options.
COPD and GASTROESOPHAGEAL REFLUX DISEASE
The prevalence of gastroesophageal reflux disease (GERD) among COPD patients is significantly higher than in the normal population and a potential risk factor for exacerbation of COPD. The prevalence of GERD in COPD patients ranged between 7.7-30%. Also 58% of the COPD patients with GERD have asymptomatic reflux disease (55). In COPD patients with GERD associated risk factors are old age, female gender, many COPD medications except inhaled muscarinic antagonists (56).
Lifestyle modification and medical and surgical management have all been used to treat GERD. Treatment of the GERD in COPD, no alteration to standard acid suppression therapy is not required (56).
COPD and MALNUTRITION
In COPD, patients are usually said to be malnourished when their BMI is 20 kg/m2. Malnutrition is present in 25-40% of severe COPD patients. Aging, tissue hypoxia, decreased physical activity, increased resting metabolic rate, chronic inflammatory processes, impaired anabolic mechanisms, increased work of breathing and energy expenditure, decreased appetite cause malnutrition in COPD patients (57). Decreased weight and muscle mass effect COPD patients undesirably and malnutrition is related with increased mortality and morbidity. Energy consumption for respiration is 36-76 kkal in healthy individuals and 430-720 kkal in COPD patients respectively. Moreover, low intake and steroid therapy increase muscle wasting. Impaired muscle strenght worsens respiratoy failure, treatment response during exacerbations and prolongs weaning time from mechanical ventilation. Therefore, decreased fat free mass is more important than weight loss in COPD patients. And also electrolyte imbalance contributes muscle weakness (57). Undernourished COPD patients have longer hospital stays and more readmissions than nourished COPD patients.
Oral nutritional supplements (as powders, puddings or liquids) can be used to supplement the diet when nutrient requirements cannot be satisfied through normal food and drink. Enteral (nasogastric, naso-jejunal, gastrostomy) or parenteral nutrition can be used for COPD patients without oral intake (58).
COPD and CARDIOVASCULAR DISEASE
Cardiovascular disease is the most significant nonrespiratory contributor to both morbidity and mortality in COPD. Ischemic heart disease, heart failure, systemic hypertension and atrial fibrillation are the most common cardiovascular comorbidities in COPD.
COPD and ischemic heart disease (IHD) are both highly prevalent and share common risk factors, such as exposure to cigarette smoke, older age and sedentarism (59). The prevalence of IHD in COPD patients ranges between 16%-53%.
Chronic obstructive pulmonary disease (COPD) and heart failure (HF) frequently coexist in clinical practice (60). COPD and heart failure share some risk factors including cigarette smoking, advanced age, and systemic inflammation. The prevalence of COPD among individuals with HF ranges from 20% to 32% of cases, and 10% of hospitalized HF patients also suffer COPD (61). Heart failure has been demonstrated to worsen the prognosis of COPD (62).
Hypertension is very common in COPD patients, but is not associated with increased mortality (63). Although the pathophysiological relationship between of COPD and hypertension are not yet clear described. It seems feasible that accelerated aging, loss of connective tissue and increased arterial stiffness may predispose patients to systemic hypertension and an increased risk of cardiovascular disease in COPD patients (63).
Atrial fibrillation and COPD are often coexisted (64). The pathogenesis of atrial fibrillation in COPD is multifactorial and includes risk factors such as hypoxemia, acidosis and reduced FEV1 (64). The prevalence of atrial fibrillation in COPD patients has been reported to 23.3% (65).
Although having similar disease mechanisms, there are differences between IHD and COPD in their current treatment strategies, and the most significant difference is use of beta-agonists in COPD and beta blockers in heart disease (66). The researchs have shown that cardioselective beta blockers may be beneficial in COPD patients with IHD (67). Angiotensin-converting enzyme (ACE) inhibitors have been associated with reduced exacerbations and mortality in COPD (68).
COPD and SLEEP DISORDERS
Patients with COPD have higher prevalences of sleep problems such as insomnia, significant disturbance in sleep quality, nightmares and daytime sleepiness than the general population (69). Moreover, co-existence of obstructive sleep apnea (OSA) and COPD is also common and all negative effects of sleep do not have an adverse effect in healthy individuals but may cause problems in patients with COPD (70). Sleep is typically fragmented with diminished slow wave and rapid-eye-movement (REM) sleep, which likely represents an important contributing factor to daytime symptoms such as fatigue and lethargy. Furthermore, normal physiological adaptations during sleep, which result in mild hypoventilation in normal subjects, are more pronounced in COPD, which can result in clinically important nocturnal oxygen desaturation (NOD). The co-existence of OSA and COPD is also common, principally because of the high prevalence of each disorder, and there is little convincing evidence that one disorder predisposes to the other (70).
Proposed mechanisms for NOD are ventilation/perfusion mismatch, hypoventilation, increased upper airway resistance, reduced chemoresponsiveness, REM related muscle atonia and greater reduction in functional residual capacity during sleep. Hypoxic pulmonary vasoconstriction is considered a major driver of the development of pulmonary hypertension and cor pulmonale in COPD, and NOD also could cause nocturnal cardiac arrhythmias, nocturnal sudden cardiac death (71).?
General consensus statements suggest screening for sleep disordered breathing in COPD patients who complain of symptoms typically associated with sleep-disordered breathing such as excessive daytime somnolence and frequent nocturnal arousals from sleep (1).
The first management principle of sleep-related breathing disturbances in COPD should be to optimise oxygenation. But the concentration of added oxygen should be carefully titrated to bring the arterial oxygen tension (PaO2) up into the mildly hypoxaemic range in order to minimise the tendency towards carbon dioxide retention, particularly during sleep (72). In addition to correction of hypoxaemia is particularly important and in recent years, considerable interest has focussed on the potential benefits of noninvasive ventilation (NIV). Nocturnal positive pressure ventilation (NPPV) is the delivery of mechanically assisted breaths without placement of an artificial airway, usually with the use of a fitted nasal mask. According to consensus report, indications for usage of NPPV include: (a) symptoms (e.g. fatigue, dyspnea, or morning headache); (b) physiologic criteria (PaCO2 > 55 mmHg or 50-54 mmHg with NOD), or (c) PaCO2= 50-54 mmHg with recurrent hospitalization related to episodes of hypercapnic respiratory failure. Sleep quality and diurnal PaO2 and PaCO2 levels are better with NIV plus supplemental oxygen than with oxygen alone (73).
ANXIETY and DEPRESSION IN COPD
Depression and axiety are more prevalent in COPD than other diseases and than general population, while anxiety and depression increase the worse prognosis in COPD, COPD increases the risk of depression (RR= 1.69). There is a bidirectional relation between anxiety (RR= 1,83) depression (RR= 1.27) and COPD (74). It is not easy to diagnose depression in COPD patients because of the overlapping symptoms between COPD and depression. However, the six-item Hamilton Depression Subscale (HAM-D-6) appears to be a useful screening tool (75). Pulmonary rehabilitation programs have also been described for COPD patients for co-morbid anxiety and depression. By means of progressive exercise, training of respiratory function, and psycho-education, patients obtained better exercise tolerance, less dyspnea, and better quality of life (76).
COPD and ANEMIA
Fatigue and dyspnea are the major symptoms of anemia, and these can be related to reduced oxygen carrying capacity of blood. Furthermore, this symptom complex in patients with COPD will inevitably contribute the morbidity and mortality associated with impaired quality of life and reduced exercise capacity. The prevalence of anemia in patients with COPD varies from 7.5% to 33%. Anemia of chronic disease (ACD) is probably the most common type of anemia associated with COPD. ACD is driven by COPD-mediated systemic inflammation anemia in COPD is associated with greater healthcare resource utilization, impaired quality of life, decreased survival, and a greater likelihood of hospitalization (77).
CONCLUSION
Nighty three % of the COPD patients have at least one comorbidity. It is well known that the number of the comorbidities has an inverse relation with the outcome of COPD. Some of the comorbidities are related with mortality in COPD. Lung Cancer and cardiovascular diseases are the best known prognostic ones.? Some of the comorbidities are known as an impactor of disease management and exacerbations. Diabetes mellitus is a best example of it. Osteoporosis and the imbalance of body composition have great impact on quality of life. Depression and anxiety are often overlooked and are well related with the rate of exacerbation and symptom management. Therefore, eventhough the evidence is not well established, the current guidelines recommend the active search of the common comorbidities in COPD.
REFERENCES
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Pocket quide to COPD diagnosis, management and prevention. Updated 2015. Available: http://www.goldcopd.org/
- Decramer M, Wim Janssens, Marc Miravitlles. Chronic obstructive pulmonary disease. Lancet 2012;379:1341-51.
- Hillas G, Perlikos F, Tsiligianni I, Tzanaki N. Managing comorbidities in COPD. International Journal of COPD 2015;10:95-109.
- Divo MJ, Casanova C, Marin JM, Pinto-Plata VM, de-Torres JP, Zulueta JJ. Chronic obstructive pulmonary disease comorbidities network. Eur Respir J 2015;46:640-50.
- Celli BR, Barnes PJ. Exacerbations of chronic obstructive pulmonary disease. Eur Respir J 2007;29:1224-38.
- Smith MC, Wrobel JP.? Epidemiology and clinical impact of major comorbidities in patients with COPD. Int J Chron Obstruct Pulmon Dis 2014;9:871-88.
- Ozyilmaz E, Kokturk N, Teksut G, Tatlicioglu T. Unsuspected risk factors of frequent exacerbations requiring hospital admission in chronic obstructive pulmonary disease. Int J Clin Pract 2013;67:691-7.
- Divo M, Cote C, de Torres JP, Casanova C, Marin JM, Pinto-Plata V. Comorbidities and risk of mortality in patients with COPD. Am J Respir Crit Care Med 2012;186:155-61.
- McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax 2007;62:411-5.
- McGarvey LP, Magder S, Burkhart D, Kesten S, Liu D, Manuel RC, et al. Cause-specific mortality adjudication in the UPLIFT? COPD trial: Findings and recommendations. Respir Med 2012;106:515-21.
- Gibson PG, McDonald WM. Asthma-COPD overlap 2015: now we are six. Thorax 2015;70:683-91.
- Mannino DM, Aguayo SM, Petty TL, Redd SC. Low Lung Function and Incident Lung Cancer in the United States Data From the First National Health and Nutrition Examination Survey Follow-up. Arch Intern Med 2003;163:1475-80.
- de Torres JP, Bastarrika G, Wisnivesky JP, Alcaide AB, Campo A, Seijo LM, et al. Assessing the relationship between lung cancer risk and emphysema detected on low-dose CT of the chest. CHEST 2007;132:1932-8.
- Wilson DO, Weissfeld JL, Balkan A, Schragin JG, Fuhrman CR, Fisher SN, et al. Association of radiographic emphysema and airflow obstruction with lung cancer. Am J Respir Crit Care Med 2008;178:738-44.
- Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J 2009; 34:380-6.
- Miller J, Edwards LD, Agusti A, Bakke P, Calverley PM, Celli B, et al. Comorbidity, systemic inflammation and outcomes in the ECLIPSE cohort. Respir Med 2013;107:1376-84.
- Gao YH, Guan WJ, Liu Q, Wang HQ, Zhu YN, Chen RC, et al. Impact of COPD and emphysema on survival of patients with lung cancer: A meta-analysis of observational studies. Respirology 2016;21:269-79.
- Sanchez-Salcedo P, Wilson DO, JP de-Torres JP, Weissfeld VL, Berto J, Campo A, Alcaide AB,? et al. Improving selection criteria for lung cancer screening. The potential role of emphysema. Am J Respir Crit Care Med 2015;191:924-31.
- Cottin V, Nunes H, Brillet PY, Delaval P, Devouassou G, Tillie-Leblond I, et al. Combined pulmonary fibrosis and emphysema: a distinct underrecognised entity. Eur Respir J 2005;26:586-93.
- Katzenstein AA, Mukhopadhyay S, Zanardi C, Dexter E. Clinically occult interstitial fibrosis in smokers: classification and significance of a surprisingly common finding in lobectomy specimens. Human Pathology 2010;41:316-25.
- Lin H, Jiang S. Combined pulmonary fibrosis and emphysema (CPFE): an entity different from emphysema or pulmonary fibrosis alone. J Thorac Dis 2015;7:767-9.
- Laghi F, Adiguzel N, Tobin MJ. Endocrinological derangements in COPD. Eur Respir J 2009;34:975-96.
- Corona G, Rastrelli G, Maggi M. Diagnosis and treatment of late-onset hypogonadism: Systematic review and meta-analysis of TRT outcomes. Best Practice & Research Clinical Endocrinology&Metabolism 2013;27:557-9.
- Huhtaniemi I. Late ‑onset hypogonadism: current concepts and controversies of pathogenesis, diagnosis and treatment. Asian J Androl 2014;16:192-202.
- Corona G, Vignozzi L, Sforza A, Maggi M. Risks and benefits of late onset hypogonadism treatment; an expert opinion. World J Mens Health 2013;31:103-25.
- Mekov E, Slavova Y, Tsakova A, Genova M, Kostadinov D, Minchev D, et al. Metabolic syndrome in hospitalized patients with chronic obstructive pulmonary disease. Peer J 2015;3:e1068.
- Doehnera W, Haeuslera KG, Endresa M, Ankerb SD, MacNeee W, Lainscak M. Neurological and endocrinological disorders: orphans in chronic obstructive pulmonary disease. Respir Med 2011;105:12-9.
- Laghi F, Adiguzel N, Tobin MJ. Endocrinological derangements in COPD. Eur Respir J 2009;34:975-96.
- Mirrakhimov AE. Chronic obstructive pulmonary disease and glucose metabolism: a bitter sweet symphony. Cardiovasc Diabetol 2012;11:132.
- Guvener N, Tutuncu NB, Akcay S, Eyuboglu F, Gokcel A. Alveolar gas exchange in patients with type 2 diabetes mellitus. Endocr J 2003;50:663-7.
- Burt MG, Roberts GW, Aguilar-Loza NR, Quinn SJ, Frith PA, Stranks SN. Relationship between glycaemia and length of hospital stay during an acute exacerbation of chronic obstructive pulmonary disease. Intern Med J 2013;43:721-4.
- Pandya D, Puttanna A, Balagopal V. Systemic effects of inhaled corticosteroids: An overview. Open Respir Med J 2014;8:59-65.
- Henneicke H, Gasparini SJ, Brennan-Speranza TC, Zhou H, Seibel MJ. Glucocorticoids and bone: local effects and systemic implications. Trends Endocrinol Metab 2014;25: 197-211.
- Suissa S, Kezouh A, Ernst P. Inhaled corticosteroids and the risks of diabetes onset and progression. Am J Med 2010;123:1001-6.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrin Society clinical practice guideline. J Clin Endocrinol Metab 2011;96:1911-30.
- Janssens W, Lehouck A, Carremans C, Bouillon R, Mathieu C, Decramer M. Vitamin D beyond bones in chronic obstructive pulmonary disease: time to act. Am J Respir Crit Care Med 2009;179:630-6.
- Holick MF. Vitamin D deficiency. N Engl J Med 2007;357:266-81.
- Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An Official American Thoracic Society/European Respiratory Society Statement: Key Concepts and Advances in Pulmonary Rehabilitation. Am J Respir Crit Care Med 2013;188:13-64.
- Rabinovich RA, Vilaro J. Structural and functional changes of peripheral muscles in chronic obstructive pulmonary disease patients. Curr Opin Pulm Med 2010;16:123-33.
- Maltais F, Decramer M, Casaburi R, Barreiro E, Burelle Y, Debigare R, et al; ATS/ERS Ad Hoc Committee on Limb Muscle Dysfunction in COPD. An official American Thoracic Society/European Respiratory Society Statement: update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2014;189:15-62.
- Cielen N, Maes K, Gayan-Ramirez G. Musculoskeletal disorders in COPD. Bio Med Int 2014;2014:965764. Doi: 10.1155/2014/965764
- Man WD, Kemp P, Moxham J, Polkey MI. Skeletal muscle dysfunction in COPD: clinical and laboratory observations. Clin Sci 2009;117:251-64.
- Choudhury G, Rabinovich R, MacNee W. Comorbidities and systemic effects of COPD. Clin Chest Med 2014;35:101-30.
- Pryor JA, Prasad SA. Physiotherapy for respiratory and cardiac problems: adults and paediatrics. 4th ed. Churchill Livingstone: London; 2008.
- Cielen N, Maes K, Gayan-Ramirez G. Musculoskeletal disorders in COPD. Bio Med Int 2014;2014:965764.
- Seymour JM, Spruit MA, Hopkinson NS, et al. The prevalence of quadriceps weakness in COPD and the relationship with disease severity. Eur Respir J 2010;36:81-8.
- Donaldson AV, Maddocks M, Martollini D, Polkey MI, Man WD. Muscle function in COPD: a complex interplay. Int J Chron Obstruct Pulmon Dis 2012;7:523-35.
- WHO Scientific Group, "Prevention and management of osteoporosis: report of aWHO scientific group," internet communication, 2013.
- Bolton CE, Ionescu AA, Shiels KM, Pettit RJ, Edwards PH, Stone MD, et al. Associated loss of fat-free mass and bone mineral density in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004;170:1286-93.
- DeVries F, van Staa TP, Bracke SGM, Cooper C, Leufkens HGM, Lammers JWJ. Severity of obstructive airways disease and risk of osteoporotic fracture. Eur Respir J 2005;25:879-84.
- Kjensli A, Mowinckel P, Ryg MS, Falch JA. Low bone mineral density is related to severity of chronic obstructive pulmonary disease. Bone 2007;40:493-7.
- Graat-Verboom L, Wouters EF, Smeenk FW, van den Borne BE, Lunde R, Spruit MA. Current status of research on osteoporosis in COPD: a systematic review. Eur Respir J 2009;341:209-18.
- Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356:775-89.
- Langhammer A, Forsmo S, Syversen U. Long-term therapy in COPD: any evidence of adverse effect on bone? Int J Chron Obstruct Pulmon Dis 2009;4:365-80.
- Smith MC, Wrobel JP. Epidemiology and clinical impact of major comorbidities in patients with COPD. Int J Chron Obstruct Pulmon Dis 2014:9;871-88.
- Patel AR, Hurst JR. Extrapulmonary comorbidities in chronic obstructive pulmonary disease: state of the art. Expert Rev Respir Med 2011:5;647-62.
- Schols AM, Ferreira IM, Franssen FM, Gosker HR, Janssens W, Muscaritoli M, et al. Nutritional assessment and therapy in COPD: a European Respiratory Society statement. Eur Respir J 2014;44:1504-20.
- Annemie MWJ. Schols. Nutrition as a metabolic modulator in COPD. Chest 2013;144:1340-5.
- Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J 2009;33:1165-85.
- de Miguel D?ez J, Chancafe Morgan J, Jim?nez Garc?a R. The association between COPD and heartfailure risk: a review. Int J Chron Obstruct Pulmon Dis 2013;8:305-12.
- Ni H, Nauman D, Hershberger RE. Managed care and outcomes of hospitalization among elderly patients with congestive heart failure. Arch Intern Med 1998;158:1231-6.
- Flu WJ, van Gestel YR, van Kuijk JP, Hoeks SE, Kuiper R, Verhagen HJ, et al. Co-existence of COPD and left ventricular dysfunction in vascular surgery patients. Respir Med 2010;104:690-6.
- Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis 2015:10;95-109.
- Brekke PH, Omland T, Smith P, S?yseth V. Underdiagnosis of myocardial infarction in COPD-Cardiac Infarction Injury Score (CIIS) in patients hospitalised for COPD exacerbation. Respir Med 2008;102:1243-7.
- Buch P, Friberg J, Scharling H, Lange P, Prescott E. Reduced lung function and the risk of atrial fibrillation in the Copenhagen City Heart Study. Eur Respir J 2003;21:1012-6.
- Roversi S, Roversi P, Spadafora G, Rossi R, Fabbri LM. Coronary artery disease concomitant with chronic obstructive pulmonary disease. Eur J Clin Invest 2014;44:93-102.
- Etminan M, Jafari S, Carleton B, FitzGerald JM. Beta-blocker use and COPD mortality: a systematic review and meta-analysis. BMC Pulm Med 2012;12:48.
- Mortensen EM, Copeland LA, Pugh MJV, Restrepo MI, de? Molina RM, Nakasihima B, et al. Impact of statins and ACE inhibitors on mortality after COPD exacerbations. Respiratory Research 2009:10;45.
- Collop N. Sleep? and sleep disorders in chronic obstructive pulmonary disease. Respiration 2010;80:78-86.
- Budhiraja R, Siddiqi TA, Quan SF. Sleep disorders in chronic obstructive pulmonary disease: etiology, impact, and management. J Clin Sleep Med 2015;11:259-70.
- Sidney S, Sorel M, Quesenberry CP Jr, DeLuise C, Lanes S, Eisner MD. COPD and incident cardiovascular disease hospitalizations and mortality: Kaiser Permanente Medical Care Program. Chest 2005;128:2068-75.
- McNicholas WT, Verbraecken J, Marin JM. Sleep disorders in COPD: the forgotten dimension. Eur Respir Rev 2013;22:365-75.
- Meecham Jones DJ, Paul EA, Jones PW, Wedzicha JA. Nasal pressure support ventilation plus oxygen compared with oxygen therapy alone in hypercapnic COPD. Am J Respir Crit Care Med 1995;152:538-44.
- Atlantis E, Fahey P, Cochrane B, Smith S. Bidirectional associations between clinically relevant depression or anxiety and COPD: a systematic review and meta-analysis. Chest 2013;144:766-77.
- Stage KB, Middelboe T, Stage TB. Depression in COPD-management and quality of life considerations. Int J Chron Obstruct Pulmon Dis 2006;1:315-20.
- Paz-Diaz H, Montes de Oca M, Lopez JM, Celli BR. Pulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPD. Am J Phys Med Rehabil 2007;86:30-6.
- Ferrari M, Manea L, Anton K, Bruzzone P, Meneghello M, Zamboni F. Anemia and hemoglobin serum levels are associated with exercise capacity and quality of life in chronic obstructive pulmonary disease. BMC Pulm Med 2015;15:58.
Yazışma Adresi (Address for Correspondence)
Dr. Nurdan K?KT?RK
Gazi ?niversitesi Tıp Fak?ltesi,
G?ğ?s Hastalıkları Anabilim Dalı,
ANKARA - TURKEY
e-mail: kokturk.nurdan@gmail.com