CASE REPORT
Doi: 10.5578/tt.10005
Tuberk Toraks 2016;64(2):175-178

Germ h?creli t?m?r?n endobronşiyal metastazı: İki olgu sunumu
Ayperi ?ZT?RK1, Zafer AKTAŞ1, Aydın YILMAZ1
1 Ankara Atat?rk G?ğ?s Hastalıkları ve G?ğ?s Cerrahisi Eğitim ve Araştırma Hastanesi, Girişimsel Pulmonoloji,
Ankara, T?rkiye
1 Clinic of Interventional Pulmonology, Ankara Ataturk Chest Diseases and Chest Surgery Training and Research Hospital,
Ankara, Turkey
?ZET
Germ h?creli t?m?r?n endobronşiyal metastazı: İki olgu sunumu
Ekstratorasik malignitelerin akciğer metastazları sık g?r?lmekle birlikte endobronşiyal metastazları (EBM) nadirdir. ?zellikle meme, kolon ve renal karsinomların EBM'leri bilinmektedir. Ancak germ h?creli t?m?rlerin EBM'leri ?ok nadirdir. Otuz dokuz yaşında ve 27 yaşında iki erkek hasta hemoptizi ve dispne şikayetleri ile farklı zamanlarda hastanemize başvurdu. Her ikisinin de ?zge?mişlerinde mikst germ h?creli t?m?r nedeniyle sol orşiektomi ?yk?leri (sırayla iki yıl ve bir yıl ?nce) mevcuttu. Akciğer grafilerinde ve toraks bilgisayarlı tomografilerinde ilk hastada sağ ?st lob atelektazisi, ikinci hastada ise sağ total atelektaziyle uyumlu g?r?n?m izlendi. Yapılan fiberoptik bronkoskopilerinde ilk olguda sağ ?st lob girişini obstr?kte eden, ikinci olguda ise sağ ana bronşu tama yakın tıkayan kanamalı EBL izlendi. Her iki olguya genel anestezi altında tanı ve tedavi ama?lı rijid bronkoskopi ile argon plazma koag?lasyon ve mekanik rezeksiyon (debulking) uygulandı. İlk hastada parsiyel a?ıklık sağlanırken, ikinci hastada total atelektazi tamamen a?ıldı. Her iki olgunun biyopsileri imm?nhistokimyasal inceleme sonucu mikst germ h?creli t?m?r?n EBM'si şeklinde rapor edildi. Germ h?creli t?m?rlerin EBM'si az g?r?lmekte olup ?zellikle lobar ya da total atelektaziye neden olacak şekilde ortaya ?ıkması ?ok nadirdir. Bu olgular eşliğinde EBM'lerin primer akciğer malignitelerinden ayırt edilmesinin hem tedavi hem de prognoz a?ısından ?nemli olduğunu vurgulamak istedik.
Anahtar kelimeler: Girişimsel pulmonoloji, endobronşiyal metastaz, mix germ h?creli testis t?m?r?
SUMMARY
Endobronchial metastasis of mixed germ cell tumors: two cases
Lung metastases from extrapulmonary malignancies are common however endobronchial metastases (EBM) from nonpulmonary neoplasms are rare. A variety of extrathoracic tumors have a tendency to EBM especially breast, colon, and renal carcinomas are most frequent reported tumors however EBM of germ cell tumors are extremely rare. A 39-year-old and a 27-year-old male patient were admitted to our hospital with hemoptysis and dyspnea at different times. Both of them had a history of left orchiectomy due to mixed germ cell tumor two years and one year ago, respectively. On chest X-Ray and thorax computed tomography, first had a right upper lobe atelectasis and second had right total atelectasis. Fiberoptic bronchoscopy (FOB) performed and a vascularized endobronchial lesion (EBL) which tended to bleed was seen in the orifis of right upper lobe in the first case and right main bronchus was totally obstructed by EBL also in the second. Interventional bronchoscopy was performed via rigid bronchoscopy for biopsy and palliative treatment (argon plasma coagulation and debulking) in both two patients because of tendency to bleeding. A partial aperture was achieved at right upper lobe bronchus in the first case and total atelectasis resolved in the second case. Immunohistochemically, histopathological examinations of both patients biopsies confirmed EBM of mixed germ cell tumors. In conclusion, EBM of the germ cell tumors especially with total or partial atelectasis are extremely rare. We want to present? these cases to emphasize the importance of distinguishing EBM from primary lung carcinoma which treatment and survival could be different.
Key words: Interventional pulmonology, endobronchial metastasis, mixed germ cell tumors
INTRODUCTION
Pulmonary metastasis of extrapulmonary malignancies are frequent however pure endobronchial metastasis (EBM) were rarely reported. The prevalence of EBM originating from extrathoracic neoplasms is variable, ranging from 2 to 28% of all pulmonary metastasis (1,2). A variety of extrathoracic tumors has a tendency to EBM; especially breast, colon, and renal carcinomas are most frequent reported tumors (1,3,4). EBM of germ cell tumors are extremely rare but mediastinal nodal enlargements due to testicular seminomas are frequent (5).
Case 1
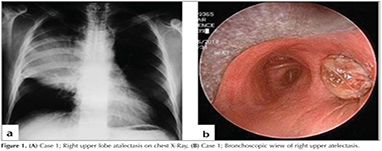
A 39-year-old male patient referred to our clinic with a history of hemoptysis and dyspnea? which persisted for two weeks. The only remarkable finding in his medical records was left orchiectomy which performed two years ago and pathologic examination revealed a mixed germ cell tumor. He was a smoker with a history of 30 pack-years. His physical examination was normal. Routine laboratory tests erythrocyte sedimentation rate was 120 mm/h. Chest X-Ray was consistent with right upper lobe atelectasis (Figure 1a). Thorax computerized tomography (CT) showed a mass lesion localized in right hilum (10 x 8 x 7 cm). Positron emission tomography (PET-CT) revealed multiple mediastinal lymph nodes uptakes. Fiberoptic bronchoscopy (FOB) performed and a vascularized endobronchial lesion which tended to bleed was seen in the? orifis of right upper lobe (Figure 1b).
Case 2
A 27-year-old male patient admitted to our emergency clinic with hemoptysis and dyspnea. He had a history of left orchiectomy due to mixed germ cell tumor one year ago. Chest X-Ray was consistent with right total atelectasis. Thorax CT revealed a large mass lesion involved to right main bronchus and lesion had indistinguishable boundaries to a consolidation area. In addition to mass lesion and consolidation, there was a volume loss in right lung (Figure 2a). FOB performed and revealed that right main bronchus was totally obstructed by endobronchial lesion (EBL). The distal end of trachea, main carina was infiltrated and the entry of left main bronchus was narrowed about 50% (Figure 2b). There was a major risk of bleeding and asphyxia so biopsy did not performed by FOB.
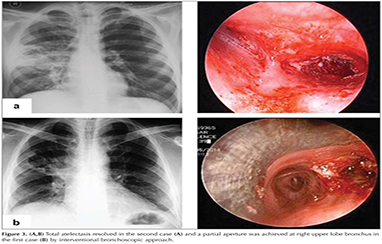
Interventional bronchoscopy was performed via rigid bronchoscopy for biopsy and palliative treatment in both two patients. A partial aperture was achieved at right upper lobe bronchus in the first case and total atelectasis resolved in the the second case by interventional bronchoscopic approach. (Figure 3a and b). Histopathological examinations of both patients bronchus biopsies confirmed EBM of mixed germ cell tumors and immunohistochemical staining was strongly positive for PLAP and focal positive for PAS. Patients were referred to medical oncology department for further treatments.
Discussion
Lung metastases from extrapulmonary primary malignancies are common however endobronchial metastases from nonpulmonary neoplasms are rare. A variety of primary tumors have been associated with EBM, predominantly breast, colon, and renal carcinomas (1,3). EBM from testicular seminomas is extremely rare. The majority of testicular tumors originate from the main cell type of testicular germ cells. Germ cell tumors are frequently composed by multiple cell types, therefore they are called mixed type tumors and most commonly embryonic carcinoma (50%) and seminoma (30-40%) were reported. Only a few reports of primary testicular seminoma causing EBM have been published (5,6,7).?
Extrapulmonary malignancies involve lungs by different routes (7,8). Direct lymphatic spread, secondary invasion from a parenchymal or mediastinal lesion, transbronchial aspiration or direct invasion are possible routes (8). The most common metastatic spread of testicular tumors occurs via lymphatic system to the retroperitoneal lymph nodes and also spread via blood usually to the lung, liver, brain and bone. Pulmonary metastases are observed in approximately 15% of patients with testicular seminoma (7).
The most common symptoms are cough and hemoptysis with dyspnea and wheezing which presents less often in EBM, similar to primary bronchogenic carcinoma. However, some patients are asymptomatic (3,4). In our cases the only symptoms on admission were hemoptysis and dyspnea.
Radiologic findings? in patients with EBMs are quite variable. Evidence of atelectasis and multiple pulmonary nodules, hilar masses, mediastinal lymphadenopathy, or normal chest radiographic findings may present. Mediastinal nodal enlargement is the most common intrathoracic manifestation of metastatic testicular seminoma. As a conclusion, it is difficult to differentiate between diagnoses of primary lung carcinoma and EBM on the basis of the symptoms and radiographic findings alone. As in our patients, histopathological examination and immunohistochemical staining should be performed for definitive diagnosis of metastatic testicular tumors. The most reliable methods should be used for the diagnosis of EBM considering possible complications such as bleeding so interventional bronchoscopic techniques can be preferred like we did in our patients.
Interval between diagnosis of the primary tumor and the EBM is generally long, ranges from 0 to 65 months (9). Survival is variable according to the primary tumor, but prognosis is generally poor. However, 5-year survival in metastatic testicular carcinoma is approximately 82% in patients with only lung or lymph node involvement (10).
In conclusion, EBM of the germ cell tumors especially with total or partial atelectasis? are extremely rare. We want to present these cases to emphasize the importance of distinguishing EBM from primary lung carcinoma which treatment and survival could be different.
REFERENCES
- Braman SS, Whitcomb ME. Endobronchial metastasis. Arch Intern Med 1975;135:543-7.
- Shepherd MP. Endobronchial metastatic disease. Thorax 1982;37:362-5.
- Marchioni A, Lasagni A, Busca A, Cavazza A, Agostini L, Migaldi M, et al. Endobronchial metastasis: an epidemiologic and clinicopathologic study of 174 consecutive cases. Lung Cancer 2014;84:222-8.
- Akoglu S, U?an ES, Celik G, Sener G, Sevin? C, Kilin? O, et al. Endobronchial metastases from extrathoracic malignancies. Clin Exp Metastasis 2005;22:587-91.
- ?zsu S, Erol M, ?ztuna F, Ers?z S, Kavgaci H, Aksoy HZ, et al. Endobronchial metastasis from testicular seminoma. Med Princ Pract 2008;17:493-5.
- Varma VA, Lipper S, Kahn SB. Endobronchial metastasis from testicular seminoma. Arch Pathol Lab Med 1981;105:680.
- Williams MP, Husband JE, Heron CW. Intrathoracic manifestations of metastatic testicular seminoma: a comparison of chest radiographic and CT findings. Am J Roentgenol 1987;149:473-5.
- Fitzgerald RH. Endobronchial metastasis. South Med J 1977;70:440-1.
- Kiryu T, Hoshi H, Matsui E, Iwata H, Kokuba M, Shimokawa K, et al. Endotracheal/endobronchial metastases. Chest 2001;119:768-75.
- International Germ Cell Cancer Collaborative Group. International Germ Cell Consensus Classification: a prognostic factor-based staging system for metastatic germ cell cancers. J Clin Oncol 1997;15:594-603.
Yazışma Adresi (Address for Correspondence)
Dr. Ayperi ?ZT?RK
Ankara Atat?rk G?ğ?s Hastalıkları ve
G?ğ?s Cerrahisi Eğitim ve Araştırma Hastanesi,
Girişimsel Pulmonoloji Kliniği,
ANKARA -? TURKEY
e-mail: drayperi@yahoo.com