RESEARCH ARTICLE
Doi: 10.5578/tt.9142
Tuberk Toraks 2016;64(2):105-111

?l??l? doz inhaler-spacer kullanımı eğitiminin ?ocuklarda astım kontrol? sağlanmasındaki etkileri
Ahmet T?RKELİ1, ?zge YILMAZ1, Hasan Y?KSEL1
1 Department of Pediatric Allergy and Pulmonology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
1 Celal Bayar ?niversitesi Tıp Fak?ltesi, ?ocuk Allerji ve Pulmonoloji Bilim Dalı, Manisa, T?rkiye
?ZET
?l??l? doz inhaler-spacer kullanımı eğitiminin ?ocuklarda astım kontrol? sağlanmasındaki etkileri
Giriş: Hatalı ?l??l? doz inhaler(?Dİ)-spacer kullanım tekniği ila?ların? akciğerlere optimalden daha az dağılmasına ve k?t? astım sonu?larına neden olabilir. Bu ?alışmanın amacı doğru ?Dİ-spacer kullanımı ve astım kontrol?nde standardize edilmiş eğitimin etkilerini değerlendirmek ve bu sonu?lar ile ilişkili fakt?rleri belirlemektir.
Materyal ve Metod: Bu ?alışma ?ocuklarda astım kontrol?nde ?Dİ-spacer cihazı kullanımına ilişkin standart eğitimin etkisini değerlendiren kohort bir ?alışmadır. Bu ?alışmaya ?Dİ-spacer kullanan astımlı ?ocuklar ve ebeveynleri alındı. ?ocuklar standart eğitimin ardından iki ay boyunca takip edildi ve astım kontrol?ndeki değişiklikler kaydedildi.
Bulgular: 2.5 ve 13 yaşları arasında otuz sekiz ?ocuk (14 kız ve 24 erkek) ?alışmaya alındı. ?ocukların yaş ortalaması 7.5 ? 2.8 yıl idi. İzlemde 6 hasta ?alışmadan ayrıldı ve otuz iki hasta ?alışmayı tamamladı. Ortalama inhalasyon tekniği puanı eğitim ?ncesinde 4.9 ? 1.3 idi ve eğitim sonrası 7.8 ? 0.4 olarak anlamlı şekilde arttı (p< 0.001). Ortalama astım kontrol ?l?eği (ACQ) puanı eğitim ile anlamlı derecede azaldı (Sırasıyla 0.77 ? 0.9 vs 0.1 ? 0.1, p< 0.001). Benzer şekilde astım semptom skoru (ASS) da eğitim ile anlamlı şekilde 4.3 ? 3.6'dan? 0.2 ? 0.7'ye d?şt? (p< 0.001). ?Dİ-spacer kullanımında en sık yapılan hata hastaların %78.9'unun eğitim ?ncesinde kullanım sonrası ağzın durulanmaması olarak tespit edilmiştir.
Sonu?: ?ocuklar ve ebeveynler i?in ?Dİ-spacer cihazı kullanımında standardize eğitimin verilmesi doğru ?Dİ-spacer kullanımına yol a?ar ve bu da astım semptom skoru ve astım kontrol?ndeki iyileşmeyle ilişkilidir.
Anahtar kelimeler: Astım kontrol?, ?ocuk, inhalasyon tekniği, ?l??l? doz inhaler, spacer, eğitim
SUMMARY
Metered dose inhaler-spacer use education effects on achieve asthma control in children
Introduction: Improper Metered Dose Inhaler (MDI)-spacer use technique? can result? in less than optimal delivery of medicine to the lungs and poor asthma? outcomes. The aim of this study was to evaluate the influence of standardized education on proper MDI- spacer use and asthma control in children with asthma and to identify the factors associated with these results.
Materials and Methods: This is a cohort study that evaluated the influence of standardized education about MDI-Spacer device use on asthma control in children. Asthmatic children using? MDI-Spacer device and their parents were enrolled in this study. Children were followed up for two months after standardized education and the change in asthma control was recorded.
Results: Thirty eight children (14 females and 24 males) aged between 2.5 and 13 years were enrolled in the study. Mean age of the children was 7.5 ? 2.8 years. Six patients were lost to follow up and thirty two patients completed the study. Mean inhalation technique score was 4.9 ? 1.3 before education and increased significantly to 7.8 ? 0.4 after education (p< 0.001). Mean Asthma Control Questionnaire (ACQ) score decreased significantly with education (0.77 ? 0.9 vs 0.1 ? 0.1 respectively, p< 0.001).? Similarly, mean asthma symptom score (ASS) decreased significantly from 4.3 ? 3.6 to 0.2 ? 0.7 with education (p< 0.001). Most common mistake in use of MDI-Spacer device use was detected to be lack of mouth rinsing after use before education in 78.9% of the patients.
Conclusion: Providing standardized education about MDI-Spacer device use to children and parents leads to correct MDI-Spacer device use and is associated with improvement in asthma symptom score and asthma control.
Key words: Asthma control, children, inhalation technique, metered dose inhaler, spacer, education
INTRODUCTION
Inhalation therapy is a necessary part of treatment for many of the chronic lung diseases of childhood such as asthma (1). Global initiative for asthma (GINA) indicates that inhaled steroids are the mainstay of asthma treatment in children (2). However effective asthma management can only be done with good self management and optimal use of asthma medications via inhaler device (3,4). In 2011, GINA is focused on patient education about asthma (2). Inhaled treatment has many advantages such as direct fast onset of action due to local delivery high concentration of the drug to the airways with minimal systematic side effects however, use of these medications with improper technique leads to the inefficacy of treatment (5,6,7,8). Inefficient inhaler treatment results in poor asthma outcomes, frequent exacerbations, increased hospitalization rates and medication cost (3,5,8,9,10,11).
A large number of inhalation devices are used for delivery of asthma medication in children (12). Proper prescription of inhaler devices especially in young children are important to the success of drug treatment (10). MDI are the therapy of choice for inhaled treatment in young children, but this often requires the use of spacers (7,9,10,13). Spacers that require breathing at tidal volume, have high clinical efficacy with low oropharyngeal deposition. These devices eradicate the problem of cooperation that exists with MDIs due to the one way valve system that open with inspiration and close with expiration (6,9). Younger children may need the use of a mask tightly sealing to the face (6,9). Although, use of spacers increases the clinical MDI therapy in young children, improper technique may eliminate this advantage. Therefore, the most important step for the effective asthma management is achieved by demonstration of the correct inhaler device technique by healthcare professionals (HCP) to patients and/or caregivers.
Influence of standardized education of patients on improvement of inhalation technique has been demonstrated (3,4,7,9,10). However influence of this modality on asthma control on long term has only achieved in a few number of previous studies in children (3,14,15). Therefore, the aim of this study was to evaluate the change in asthma control and after standardized education on proper MDI-Spacer use.
MATERIALS and METHODS?
Study Population
Children with uncontrolled asthma despite treatment with MDI-Spacer and their parents were enrolled in this study. They were recruited consecutively from the Pediatric Allergy and Pulmonology outpatient department. Diagnosis of asthma was based on GINA criteria. All children had recurrent exacerbations detected by a physician before and reversibility of bronchoconstriction was demonstrated either by clinical findings or by spirometry (2). Inclusion criteria;
1. Being diagnosed as having uncontrolled asthma despite treatment.
2. Using inhaled treatment MDI-Spacer.
Exclusion criteria;
1. Having a chronic lung disease other than asthma that may influence Asthma control questionnaire (ACQ) results.
2. Having received a standardized education MDI-Spacer use from a physician previously.
Study Design
This is a cohort study that evaluated the influence of standardized education about MDI-Spacer use on asthma control in children. Children were followed up for two months after standardized education and the change in asthma control was recorded.
Measurements
Age, gender, duration of asthma diagnosis, duration of aerosol treatment use were recorded as well as the age, gender, education and occupation of the parents. Asthma symptom score was evaluated for all children and ACQ was filled in by all parents at the beginning and end of the study period.
Asthma Symptom Score
Asthma symptom score (ASS) consisted of four items scored 0 to three. Total score was expresed as the sum of all scores. The items were "how commonly did you feel wheezing or tightness in the chest?", "how often did you wake up due to cough or tightness in the chest?", "how often did you have asthma symptom upon waking up in the morning?" and "how often did cough, wheezing or tightness in the chest bother you during your physical activities?". The responses ranged between never, less often than once a week, 1-3 days a week and 4-7 days a week. The score increased as the symptoms increased (16).
Asthma Control Questionnaire
ACQ was developed by Juniper et al and validity and reliability has been demonstrated (17). It is composed of 5 questions about symptoms, 1 question about bronchodilator use during the previous week and one question about FEV1% change. The last item about spirometry may be omitted when children don't coorperate with respiratory function test. All questions are scored 0 to 6 and total score is expressed as the mean of these scores. Asthma control deteriorates as the score increases (18). Clinically important change in ACQ score is reported to be 0.5 (17).
Standardized Education on Metered Dose Inhaler-Spacer Use
All children and/or parents were instructed to demonstrate how they use their MDI-Spacer at the beginning of the study. Then, the pediatric allergy and pulmonology nurse told and demonstrated MDI-Spacer use to the child and parent. Finally, the child and/or parent was asked to MDI-Spacer use again. Inhalation technique evaluation form that consisted of eight steps of MDI-Spacer use was filled in for both demonstrations by the study participants and one point was given for each step that was completed successfully (Table 1) (13). Total spacer use score was expressed as the sum of points received for each step. Study participants were called in two months later and were asked to demonstrate MDI-Spacer use again and inhalation technique evaluation form was filled in again.
Statistical Analysis
Sociodemographic and clinical findings were presented as number or mean ? SD as appropriate. Statistical analysis of data was performed by SPSS 15.0 (Chicago IL) computer software. Mean MDI-Spacer use scores, ASS and ACQ scores at the beginning and end of the study period were compared by paired samples t test. Correct MDI-Spacer use step before and after education in each step were compared with Pearson's Chi-square test. Statistical significance was defined as p< 0.05.
The study was approved by the ethical committee of the University and informed consent was taken from the parents of children.
RESULTS
Sociodemographic and Asthma Characteristics
Thirty eight children (14 females and 24 males) aged between 2.5 and 13 years were enrolled in the study. Mean age of the children was 7.5 ? 2.8 years. Six patients were lost to follow up and thirty two patients completed the study.
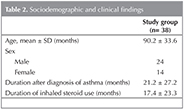
Mean duration of asthma was 21.2 ? 27.2 months and mean duration of Spacer with MDI-Spacer use was 17.4 ? 23.3 months (Table 2).
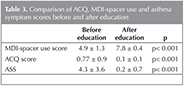
Asthma Symptom, Asthma Control Questionnaire and Inhalation Technique Scores
Mean inhalation technique score was 4.9 ? 1.3 before education and increased significantly to 7.8 ? 0.4 after education (p< 0.001). Mean ACQ score decreased significantly with education (0.77 ? 0.9 vs 0.1 ? 0.1 respectively, p< 0.001). Similarly, mean asthma symptom score decreased significantly from 4.3 ? 3.6 to 0.2 ? 0.7 with education (p< 0.001) (Table 3).
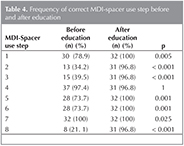
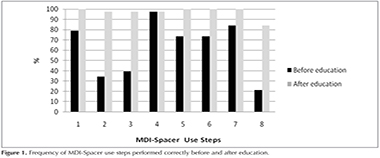
Frequency of correct MDI-Spacer use step before and after education in each step is shown in Table 4 and Figure 1. Most common mistake in use of MDI-Spacer device use was detected to be lack of mouth rinsing after use before education in 78.9% of the patients. This was followed by lack of exhalation before inhaling the drug (65.8%) and not shaking the inhaler before use (60.5%). Most common mistakes that were detected after education were not shaking the inhaler before use, not exhaling before inhalation of the drug and lack of mouth rinse and face cleaning after use (2.6% each) (Table 4 and Figure 1).
CONCLUSION
We found that MDI-Spacer use by children was frequently incorrect. The results of our study indicated a significant improvement of asthma control and symptom score with improved inhalation technique after a standardized education on MDI-Spacer use. This is in concordance with the international guidelines that state the importance of patient and family education on long term asthma treatment (2,3).
Currently, inhaled corticosteroids are very effective in reducing asthma associated morbidity and mortality (2,19). In children with asthma, technical education at the time of prescription of inhaled medication is essential for correct inhalation technique (7,20). Responsibility HCP's in inhaler use are crucial for both in achieving initial correct inhaler technique and also in maintaining this correct inhaler application over time. Most patients are trained on proper inhaler technique by physicians or nurses and, to a lesser extent, pharmacists (5,21). But only 15 to 69% of HCP can demonstrate correct inhaler device use, minority of patients receive inhaler use education (1,7,21,22). Consequently, approximately half of patients who initially learn how to use their inhalers properly, do not maintain this correct technique over time (21).
Using inhaler device is a problem for all ages of patients. In a review of 21 studies looking at misuse of metered dose inhalers, poor technique was estimated to be prevalent in 14 e 90% (with an average of 50%) of cases (20). Many research have shown that a high proportion of children do mistakes while using inhaled treatments (10,13,23). Lack of cooperation in young children especially hand mouth coordination may interfere with effective inhalation therapy with MDI (13,24,25). It has been demonstrated that the most common mistakes include not exhaling before starting, not shaking the MDI and inhaling for a very short time (10,13,21,23,24,25,26,27). Similar with other studies, common mistakes detected in our study were lack of mouth rinsing after use followed by lack of exhalation before inhaling the drug and not shaking the inhaler before use.
Also repeated education is required for correct inhaler technique., due to inhaler technique may worsen after initial tutorial (9,25,28). HCP should repeat this instructions at subsequent visits to confirm correct usage of inhaler device (29,30). Another critical step is the way of the education. Verbal instruction in addition to physical demonstration is the most effective patient training technique in correct inhaler use like the method, we used in our study (28). It has been reported that most children and adults reduce their mistakes in inhalation device use after getting education about it (31,32). Repeated educations result in better inhalation technique and play a key role in successful inhalation therapy (8,9,22,23,25,30,31). It is reported that repeated education about MDI inhalation technique resulted in a statistically significant improvement in MDI technique scores when compared to single education (33,34). Getting a second education besides the one at the time of first prescription increased the rate of correct technique to 91% (33). These results are similar to our results in which we have shown that children completed only 4.9 ? 1.3 of steps required for correct use of MDI-Spacer before receiving standard education despite the fact that they had been suing it before being enrolled in the study. This number increased to 7.8 ? 0.4 after education session.
The main aim of asthma therapy in current international guidelines is to control astma by inhibiting undesirable consequences (2). Efficacy of the inhaled treatments in astma patients, depends on the quantity of delivered medication into the lungs which is mostly influenced by the inhalation techniques. Improvement in MDI technique provides better delivery of medication into the lungs thus clinically significant improvement (11). Inappropriate inhalation technique decreases drug delivery in the lungs and decreases the efficacy of medical treatment and hinder better asthma control (7,8,10,11). People with asthma and improper inhaler technique were shown to have poorer symptom control compared to those with good inhaler technique, with a subsequent increase in medical or emergency visits (8,11,20,25). Furthermore, as improved inhalation technique has been shown to improve adherence to asthma therapy (possibly due to the positive reinforcing effects of improved symptom relief concurrent with improved medication administration (29).
ACQ is an indicator developed by Juniper et al. to assess control of asthma. Correlation of ACQ with functional parameters related to asthma in children has also been demonstrated in six minute walking test in a previous study (35). Some authors reported that patients who use their inhalation device correctly have better asthma control (3,5,8,11,36). McWhirter et al, Horner and Brown showed that children with asthma have lower requirement for medication, reduction in symptoms of wheeze and improvement in children's quality of life as their inhaler skill improved (14,15). It has been shown that improvement in inhalation technique is associated with an improvement in disease specific quality of life indicated by pediatric asthma quality of life questionnaire (PAQLQ) scores and a decrease in the inhaled steroid dose required (3,31). Likewise, we have demonstrated that asthma symptom score and ACQ score improved during the two months after the children received standardized education with MDI-Spacer use. On the other hand, some authors did not detect a correlation between PAQLQ scores and correct MDI-Spacer use technique score and some others showed that asthma symptom score did not worsen despite wrong use of MDI-Spacer (32,33). These differences in different research might be attributed to many factors such as differences in study populations in terms of asthma severity and differences in standardized education protocols.
The major limitation of this study was the small sample of size of the study population. However, even with this sample size, change in the outcome variables was statistically significant.
In conclusion, incorrect use of inhaled treatment in children may be a major cause of uncontrolled asthma and improvement of MDI-Spacer use technique may lead to better asthma control and a decrease in asthma symptoms. Therefore, incorrect inhalation technique should be sought in children with uncontrolled asthma before increasing the treatment step or further diagnostic work up. Moreover, standardized and interactive education about MDI-Spacer use may be recommended as an integral component of asthma treatment in children.
ACKNOWLEDGMENTS
Hasan Yuksel and Ozge Yilmaz involvement in the conception, hypotheses delineation, and design of the study.
Ahmet Turkeli wrote and Ozge Yilmaz, Hasan Yuksel revised the manuscript.
Ahmet Turkeli took part in acquisition of the data.
Ozge Yilmaz participated in analysis and interpretation of data.
REFERENCES
- Goralski JL, Davis SD. Breathing easier: Addressing? the challenges of aerosolizing medications to infants and? preschoolers. Respir Med 2014;108:1069-74.
- 2014 GINA Report, Global? strategy for asthma management? and prevention. Updated December 2011. Available? from: http://www.ginasthma.org/GINA-Report,-Global-Strategy-for-Asthma-Management-and-Prevention.
- Vasbinder EC, Janssens HM, Rutten-van M?lken MP, van Dijk L, de Winter BC, de Groot RC, et al. e-Monitoring of Asthma therapy to improve compliance in children using a real-time medication monitoring system (RTMM): the? e-MATIC study protocol. BMC Med Inform Decis Mak 2013;13:38.
- Bosnic-Anticevich SZ, Stuart M, Mackson J, Cvetkovski B, Sainsbury E, Armour C, et al. Development and evaluation of an innovative model of inter-professional education focused on asthma medication use. BMC Med Educ 2014; 14:72.
- Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011;105:930-8.
- Pedersen S, Dubus JC, Crompton GK; ADMIT Working Group. The ADMIT series--issues in inhalation therapy. Inhaler selection in children with asthma. Prim Care Respir J? 2010;19:209-26.
- Price D, Bosnic-Anticevich S, Briggs A, Chrystyn H, Rand C, Scheuch G, et al. Inhaler competence in asthma: common errors, barriers to use and recommended solutions.Respir Med 2013;107:37-46.
- Al-Jahdali H, Ahmed A, Al-Harbi A, Khan M, Baharoon S, Bin Salih S, et al. Improper inhaler technique is associated with poor asthma control and frequent emergency department visits. Allergy Asthma Clin Immunol 2013;9:8.
- Crompton GK, Barnes PJ, Broeders M, Corrigan C, Corbetta L, Dekhuijzen R, et al.? Aerosol Drug Management Improvement Team. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respir Med? 2006;100:1479-94.
- Uijen JH, van Uijthoven YJ, van der Wouden JC, Bindels PJ. Adequate use of asthma inhalation medication in children: more involvement of the parents seems useful. BMC Res Notes? 2009;2:129.
- Baddar S, Jayakrishnan B, Al-Rawas OA. J Asthma. Asthma control: importance of compliance and? inhaler technique assessments. J Asthma 2014;51:429-34.
- Nilsson E, Chawes BL, B?nnelykke K, Vindfeld S, Moore AC, Bisgaard H. Effect of delivery device on systemic exposure to inhaled Fluticasone Propionate in children with asthma. Br J Clin Pharmacol 2014;78:435-7.
- Deerojanawong J, Promsaka na SV, Prapphal N, Hanrutakorn C, Sritippayawan S. Evaluation of metered-dose inhaler administration technique among asthmatic children and their caregivers in Thailand. Asian Pac J Allergy Immunol 2009;27:87-93.
- McWhirter J, McCann D, Coleman H, Calvert M, Warner J. Can schools promote the health of children with asthma? Health Education Research 2008;23:917-30.
- Horner SD, Brown A. Evaluating the effect of an asthma self-management intervention for rural families. J Asthma 2014;51:168-77.
- St?rdal K, Johannesdottir GB, Bentsen BS, Knudsen PK, Carlsen KC, Closs O, et al. Acid suppression does not change respiratory symptoms in children with asthma and gastro-oesophageal reflux disease. Arch Dis Child 2005;90:956-60.
- Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J 1999;14:902-7.
- Juniper EF, Svensson K, M?rk AC, St?hl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med 2005;99:553-8.
- Salvi S, Gogtay J, Aggarwal B. Use of breath-actuated inhalers in patients with asthma and COPD - an advance in inhalational therapy: a systematic review. Expert Rev Respir Med 2014;8:89-99.
- Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J 2002;19:246-51.
- Bryant L, Bang C, Chew C, Baik SH, Wiseman D. Adequacy of inhaler technique used by people with asthma or chronic obstructive pulmonary disease. J Prim Health Care 2013;5:191-8.
- Gemicioglu B, Borekci S, Can G. Investigation of knowledge of asthma and inhaler devices in pharmacy workers. J Asthma 2014;10:1-7.
- Brand PL. Key issues in inhalation therapy in children.? Curr Med Res Opin 2005;21(Suppl 4):S27-32.
- Rubin BK, Fink JB. Optimizing aerosol delivery by pressurized metered-dose inhalers. Respir Care 2005;50:1191-200.
- Marguet C, Couderc L, Le Roux P, Jeannot E, Lefay V, Mallet E. Inhalation treatment: errors in application and difficulties in acceptance of the devices are frequent in wheezy infants and young children. Pediatr Allergy Immunol 2001;12:224-30.
- Sanchis J, Corrigan C, Levy ML, Viejo JL; ADMIT Group.Inhaler devices-from theory to practice. Respir Med 2013;107:495-502.
- Sleath B, Ayala GX, Gillette C, Williams D, Davis S, Tudor G, et al. Provider demonstration and assessment of child device technique during pediatric asthma visits. Pediatrics 2011;127:642-8.
- Bosnic-Anticevich SZ, Sinha H, So S, Reddel HK.? Metered-dose inhaler technique: the effect of two educational interventions delivered in community pharmacy over time. J Asthma 2010;47:251:e6.
- M?kel? MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med 2013;107:1481-90.
- Sleath B, Carpenter DM, Ayala GX, Williams D, Davis S, Tudor G, et al. Communication during pediatric asthma visits and child asthma. J Asthma 2012;49:918-25.
- Kamps AW, Brand PL, Kimpen JL, Maill? AR, Overgoor-van de Groes AW, van Helsdingen-Peek LC, et al. Outpatient management of childhood asthma by paediatrician or asthma nurse: randomised controlled study with one year follow up. Thorax 2003;58:968-73.
- Horner SD, Fouladi RT. Improvement of rural children's asthma self-management by lay health educators. J Sch Health 2008;78:506-13.
- Kamps AW, van Ewijk B, Roorda RJ, Brand PL. Poor inhalation technique, even after inhalation instructions, in children with asthma. Pediatr Pulmonol 2000;29:39-42.
- Takemura M, Kobayashi M, Kimura K, Mitsui K, Masui H, Koyama M, et al. Repeated instruction on inhalation technique improves adherence to the therapeutic regimen in asthma. J Asthma 2010;47:202-8.
- Yuksel H, Yilmaz O, Goksen B, Ustun S, Sogut A. Is the six-minute walk test correlated with disease control and quality of life in children with asthma? Turk J Med Sci 2012;42:839-44.
- Giraud V, Allaert FA, Roche N. Inhaler technique and asthma: feasability and acceptability of training by pharmacists. Respir Med 2011;105:1815-22.
Yazışma Adresi (Address for Correspondence)
Dr. Hasan Y?KSEL
Celal Bayar ?niversitesi Tıp Fak?ltesi,
?ocuk Allerji ve Pulmonoloji Bilim Dalı,
MANİSA - TURKEY
e-mail: hyukselefe@hotmail.com