SHORT REPORT
Doi: 10.5578/tt.9700
Tuberk Toraks 2016;64(1):77-82

Trakea divertik?l?: Kronik ?ks?r?k ve tekrarlayan akciğer infeksiyonlarının nadir bir nedeni
Rajendra Prasad TAKHAR1, Motilal BUNKAR2, Shubhra JAIN3, Sanjay GHABALE3
1 Government Tıp Okulu, Solunum B?l?m?, Kota, Hindistan
1 Department of Respiratory Medicine, Government Medical College, Kota, India
2 Govt Tıp Okulu, Solunum B?l?m?, Kota, Hindistan
2 Department of Respiratory Medicine, Govt Medical College, Kota, India
3 S.M.S. Tıp Okulu Solunum Enstit?s?, Solunum B?l?m?, Jaipur, Hindistan
3 Department Of Respiratory Medicine, Institute of Respiratory Medicine, S.M.S. Medical College, Jaipur, India
?ZET
Trakea divertik?l?: Kronik ?ks?r?k ve tekrarlayan akciğer infeksiyonlarının nadir bir nedeni
Trakea divertik?l? (TD) trakea duvarının konjenital veya edinsel yapısal zayıflığı nedeniyle dışarı torbalaşması sonucu oluşan paratrakeal hava kistlerine yol a?an benign bir patolojidir. Klinik pratikte nadiren teşhis edilir ve literat?rde sınırlı sayıda olgu rapor edilmiştir. ?oğu olgu postmortem incelemelerde tesad?fen tanı alır ve ?oğunlukla sağ tarafta bulunur. Komplike olmayan TD asemptomatiktir ve semptom varsa, farinkste rahatsızlık, ?ks?r?k, dispne ve tekrarlayan solunum yolu infeksiyonu gibi komşu organa baskı veya ikincil bakteriyel infeksiyonlara bağlı ?zg?n olmayan semptomlardır. Torakoservikal ?ok kesitli spiral bilgisayarlı tomografi ve fiberoptik bronkoskopi ?nemli tanısal tetkiklerdir. Asemptomatik TD genellikle konservatif yaklaşımla tedavi gerektirmezken, komşu organa baskı ve tekrarlayan infeksiyon olan olgularda cerrahi gereklidir.
Bronkodilat?r tedaviye cevap vermeyen kronik ?ks?r?k ve tekrarlayan infeksiyonlar nedeniyle değerlendirilirken solda trakeal divertik?l saptanan 40 yaşında kadın olguyu sunuyoruz. Bilgisayarlı tomografide sol paratrakeal b?lgede dışarı k???k bir uzanım g?steren lezyon g?r?lerek TD tanısı konuldu ve fiberoptik bronkoskopi ile doğrulandı. Baryum kontrastlı grafi ile ?zefagus ve trakea arasında bağlantı g?sterilemedi. Olgu değerlendirilerek cerrahi i?in y?nlendirildi.
Anahtar kelimeler: Trakeal divertik?l?, kronik ?ks?r?k, fiber optik bronkoskopi
SUMMARY
Tracheal diverticulum: an unusual cause of chronic cough and recurrent? respiratory infections
Tracheal diverticulum (TD) defined as a typical benign out-pouching of the tracheal wall due to structural weakness, congenital or acquired in origin, resulting in paratracheal air cysts. It is rarely diagnosed in clinical practice with only limited reports in the literature. Most cases found incidentally in the postmortem examination and located on the right side. Uncomplicated TDs are usually asymptomatic and when symptoms have occurred, they usually present with non-specific symptoms like pharyngeal discomfort, cough, dyspnea, and recurrent respiratory infection due to either the compression of adjacent organs or secondary bacterial infection. Imaging techniques like thoraco-cervical multi-slice spiral computed tomography (CT) and fiber-optic bronchoscopy are important diagnostic tools for this entity. Asymptomatic TDs usually require no treatment and managed conservatively while surgical excision is indicated in cases of compression of adjacent organs and recurrent infections. Here we report a case of tracheal diverticulum on the left side, which was diagnosed as part of a work-up for chronic cough and recurrent chest infection in a 40 year old female who was already on bronchodilator without any relief. Diagnosis of TD was based on findings of computed tomography, revealing small bud like projection on left para tracheal region and further confirmed by fiber-optic bronchoscopy while the barium contrast study showed no esophageal communication. She was managed conservatively and referred for surgical excision.
Key words: Tracheal diverticulum, chronic cough, fiber-optic bronchoscopy
Geliş Tarihi/Received: 13.05.2015 • Kabul Ediliş Tarihi/Accepted: 19.05.2015
INTRODUCTION
Tracheal diverticulum is a rare entity characterized by solitary or multiple outpouchings of the tracheal wall, mostly on right side. Tracheal diverticulum can be either congenital or acquired, the difference residing mainly in the histological features of the wall. The majority of patients remain asymptomatic throughout the life and seldom diagnosed ante mortem, probably the reason for scant published literature for this entity. Tracheal diverticulum is often an incidental finding in the postmortem examination, reported in upto 1% of patients (1). Sometimes this may act as a reservoir for respiratory secretions that may spill-over into the tracheo-bronchial tree, causing repeated secondary infections and then presents with cough, dyspnea, stridor, throat irritation and chronic/ recurrent chest infections and may confuse with other etiologies like diseases of the digestive tract, vascular anomalies and pulmonary tuberculosis (2). Here we are discussing a case of tracheal diverticulum of left side presenting with chronic cough and frequent chest infection mimicking pulmonary tuberculosis along with review of literature.
CASE REPORT
A 40 years old female non-smoker housewife presented with complaints of chronic cough since five years, mucoid expectoration and episodes of low grade fever on and off since four years and dull aching diffuse chest pain on left side since two years. Since 3 weeks the frequency and severity of cough appeared to be increased without signs of dyspnoea, wheeze, haemoptysis, rhino-sinusitis or postnasal drip. She denied complaints of dysphagia, pyrosis or gastro-oesophageal reflux disease (GERD) and loss of appetite or weight. Her past medical records showed a diagnosis of recurrent respiratory tract infections and/or obstructive airway disease, for which she had multiple consultations and received inhaled bronchodilators with corticosteroid but to cause no relief. Her sputum was negative for acid fast bacilli but receiving anti-tubercular treatment without any relief. Occupational and family histories were not significant. No specific exposure to organic or inorganic materials could be identified. She did not take any medication associated with cough and no history of past surgery.
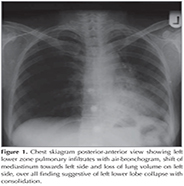
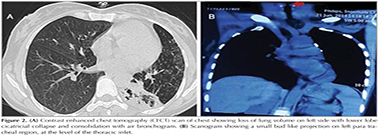
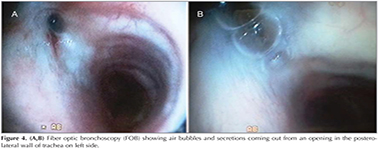
General physical and systemic examination revealed nothing abnormal except fine crepitations in left infra-scapular and infra-axillary region. Laboratory investigations were within normal limits. Pulmonary function test was normal without signs of bronchial obstruction and sputum was negative for acid fast bacilli. Her chest skiagram PA view showed left lower zone infiltrates with air-bronchogram, loss of lung volume on left side and same side shifting of mediastinum, over all finding suggestive of left lower lobe collapse with consolidation (Figure 1). Contrast enhanced chest tomography (CECT) scan of chest showed loss of lung volume on left side with lower lobe cicatricial collapse and consolidation with air-bronchogram while the scanogram revealed a small bud like projection on left para tracheal region, at the level of the thoracic inlet (arrow) (Figure 2A,B). The presence of a narrow stalk connecting the lesion with the posterior wall of the trachea was critical in establishing the diagnosis of a tracheal diverticulum. Furthermore, three-dimensional reconstruction CT ?virtual bronchoscopy confirmed our diagnosis as it showed an orifice of tracheal diverticulum in tracheal wall on left side just below the vocal cord (Figure 3). Fiber optic bronchoscopy (FOB) showed air bubbles and secretions coming out from an opening in the postero-lateral wall of trachea on left side approximate 1 cm below the vocal cords (Figure 4A, B). Further FOB revealed marked narrowing of the left lower lobe bronchus suggestive of cicatricial collapse. The diagnosis of tracheal diverticulum with left lower lobe collapse was made. The barium contrast study performed to look for any esophageal communication, but to fail (Figure 5). Bronchoalveolar lavage taken during FOB, sent for gram stain and pyogenic culture. Patient was referred for surgical management looking at the frequency of symptoms, but she denied for any operative intervention. She was then managed conservatively with antibiotics, mucolytics and vaccinations to reduce the frequency of chest infections and subsequent complication.
Discussion
Chronic and recurrent cough are common respiratory problem, most often caused by bronchial asthma and/or hyper-responsiveness, postnasal drip (PND), sinusitis and gastro-esophageal reflux (3). Tracheal diverticulum is a paratracheal air cyst which is barely a differential for such presentation.? TD is characterized by single or multiple outpouchings of the tracheal wall observed mostly during post-mortem examinations, sometimes discovered incidentally on routine chest radiography, CT or bronchoscopy (4). The reported incidence of this condition is 0.3% to 2%, varies from series to series and depends primarily on the diagnostic tool used (1). In an autopsy series, the incidence was reported to be 1% (1,5). In a recent study, thoracic Multi-Detector Computed Tomography (MDCT) scans in 700 patients revealed tracheal diverticula in 18 patients (2.57%), while another study reported its incidence of 2.38% with the same modality (6,7).
Tracheal diverticulum can be congenital and acquired types (8). Both varieties, most frequently located on the right posterolateral tracheal wall at the level of thoracic inlet or at the level of the T1-T2 vertebral body, but in the described case, had a unique presentation as tracheal diverticulum was present on left side.? The supportive presence of oesophagus and aortic arch on the left side of the tracheal wall makes it less susceptible to the development of diverticula explaining the preponderant right sided location of the diverticula (9). Congenital diverticulum are more common in males, usually single and located 4-5 cm from the vocal cords on the right lateral wall of the trachea. The exact mechanism of their origin is unclear, but thought to develop from evaginations of embryologic tracheal buds, where a supernumerary branch of the trachea develops and therefore it is composed of all the layers of the tracheal wall and the histological structure of this diverticulum resembles to that of trachea (2,8). As their communication with the trachea is often narrow leading to poor drainage of the secretions, which sometimes may become superinfected. Congenital tracheal diverticula are occasionally associated with other congenital abnormalities like Mounieir Kuhn syndrome (8).
Acquired tracheal diverticulum have an equal sex ratio and may be present anywhere in the trachea (10). Prolonged increase in intratracheal pressure from chronic violent coughing or from an occupation involving excessive vocal or pulmonary effort or obstructive lung disease with emphysema combined with the weakened musculature of the tracheal wall, causing herniation through a weak point in the trachea. Thus histologically, the wall is lined by respiratory epithelium; and devoid of mucous glands, smooth muscle or cartilage (11). Acquired form is described to be typically wide-mouthed and larger in size than congenital diverticula with adequate drainage of secretions and hence patients are often asymptomatic and infection free (10,12).
Clinically, the majority of patients with congenital or acquired diverticula are asymptomatic or present with non-specific symptoms (11,13,14). However, they might also act as a reservoir for secretions with secondary infections of the tracheobronchial tree, resulting in chronic cough, dyspnoea, stridor, throat irritation, haemoptysis, chest pain and repeated episodes of tracheobronchitis (1,2) Such events occur due to the dynamic interaction between cysts and the tracheal lumen (15).
In the current case, the patient presented with recurrent episodes of cough and authors believe that this was likely related to recurrent tracheobronchitis. Indeed, the cough may play two roles in diverticulum, either an aetiological factor in their development like in acquired variety or a symptom secondary to the lesion. Also progressive cough might also be a result of mechanical stimuli due to growing of the diverticulum, which in turn further aggravates cough, as a result of direct stimulation of the vagal nerve and also aggravates its expansion (16).
Although paratracheal air collections can seldom be seen on chest radiography, further investigations are required to assess the size and origin of the lesion. The diagnosis is relatively straightforward on computed tomography (CT), showing the presence of mediastinal cysts or paratracheal air collections (13). CT provides information regarding the location, origin, size of the lesion, size of the neck of diverticulum, presence or absence of cartilaginous rings in the wall thus helping to distinguish between congenital and acquired variety of the diverticulum along with wall thickness to assess repeated inflammation and sometimes, communication between tracheal lumen and diverticulum. CT may also show the damage to lung parenchyma as the result of chronic illness (1,11,16). Barium swallow contrast study can be done to rule out any gastrointestinal origin of the paratracheal air cyst. Bronchoscopy is definitely useful in confirming the diagnosis, which may provide a vision of the tracheal communication of the diverticula, although bronchoscopy may fail to diagnose the entity, e.g., diverticula with a very narrow opening, such as in congenital cases or those joined to the trachea by just a fibrous tract (5,11,17). On respiratory dynamic CT, the cysts expanded during forced expiration and shrank during inspiration. Change in the size of the paratracheal cyst during respiration suggests communication between the cyst and the airway. Three-dimensional reconstruction CT to create a virtual bronchoscopy may be helpful in the morphologic diagnosis of this entity, if the diagnosis remains elusive or to define the extent of the diverticulum (14).
The differential diagnosis of a paratracheal air collection includes a laryngocele, pharyngocele, Zenker's diverticulum, tracheal diverticula, an apical hernia of the lungs, Mounier-Kuhn syndrome and apical paraseptal bullae. Techniques found useful to distinguish between these disorders are a barium study and CT. Laryngocele can be seen on CT as an abnormal diverticula of the saccule of the laryngeal ventricle. Phayngeoceles and Zenker's diverticula can usually be identified by barium examination. An apical hernia has continuity with the remainder of the lung and presence of lung markings on CT scans. Apical paraseptal blebs or bullae, which are air cysts within the lung, can easily be recognized on CT scans (1,11)
Various treatment options for TD with no general consensus have been described in the literature including surgical resection, fulguration and endoscopic cauterization with a laser or electro-coagulation, and conservative measures depending on the overall health status of the patient. As the majority of patients are asymptomatic, they require no specific intervention (14). Surgical resection should be considered in young patients in whom the diverticulum is causing repeated respiratory problems, while conservative medical management with antibiotics, mucolytics and physiotherapy may be appropriate for elderly and debilitated patients. Surgical approaches will vary according to the location of the diverticulum (13).
In this case report, we describe a patient with a symptomatic tracheal diverticulum. The present case probably had congenital variety of TD as there were no other apparent causes of chronic cough (e.g. asthma, gastroesophageal reflux, sinusitis or PND or history of ACE inhibitors) leading to development of TD in this patient. Also there was no history of prolonged coughing or any neck surgery in the past. We assume the tracheal diverticulum as a reason for the recurrent cough and infections in our patient. Pooling of secretions in the pouch and secondary infection followed by spillage in tracheobronchial tree leading to tracheobronchitis would explain the recurrent cough.
Conclusion
Tracheal diverticulum is rarely reported in clinical practice or the literature, found as an incidental finding without any symptom and frequently go undiagnosed, but occasionally may act as a reservoir for secretions causing repeated episodes of tracheobronchitis, so the diagnosis should be considered in patients with persistent/recurrent coughing, particularly if the plain film radiography and spirometry are normal. The present case demonstrates the importance of keeping a tracheal diverticula in mind while dealing a patient with recurrent and chronic cough apart from well known causes of such presentation. Diagnosis can be made by Fibre-optic bronchoscopy and CT scan with 3-dimensional reconstructions. Treatment options include surgical resection and conservative management depending on the presentation.
REFERENCES
- Goo JM, Im J, Ahn KM, Moan WK, Chung JW, Park JH, et al. Right paratracheal air cysts in the thoracic inlet: clinical and radiologic significance. AJR Am J Roentgenol 1999;173:65-70.
- Early EK, Bothwell MR. Congenital tracheal diverticulum. Otolaryngol Head Neck Surg 2002;127:119-21.
- Ptok M. Chronic cough-diagnostic aspects. Laryngorhinootologie 2008;87:468-75.
- Grassi R, Rea G, Scaglione M, Brunese L, Scialpi M. Imaging of tracheocoele: report of three cases and review of the literature. Radiol Med 2000;100:285-7.
- Caversaccio MD, Becker M, Zbaren P. Tracheal diverticulum presenting with recurrent laryngeal nerve paralysis. Ann Otol Rhinol Laryngol 1998;107:362-4.
- Sharma R, Arora M, Mahajan M, Gupta P, Sharma P. A study to evaluate relationship of tracheal diverticulum with emphysematous changes in lung using multi-detector computed tomography-a report from North-West India. Clinical Medicine and Diagnostics 2014;4:79-82 DOI: 10.5923/j.cmd.20140405.01.
- Kurt A, Sayit AT, Ipek A, Tatar IG. A multi detector computed tomography survey of tracheal diverticulum. Eurasian J Med 2013;45:145-8.
- Restrepo S, Villamil MA, Rojas IC, Lemos DF, Echeverri S, Triana G, et al. Association of two respiratory congenital anomalies: tracheal diverticulum and cystic adenomatoid malformation of the lung. Pediatr Radiol 2004;34:263-6.
- Gaissert HA, Grillo HC. Complications of tracheal diverticulum after division of congenital tracheoesophageal fistula. J Pediatr Surg 2006;41:842-4.
- Sen G, Mathur S, Gupta S, Acharya S. Non-communicating fluid filled tracheal cyst. Indian J Thoracic Cardiovascular Surg 2005;21:224-5.
- Tanaka H, Mori Y, Kurokawa K, Abe S. Paratracheal air cysts communicating with the trachea: CT findings. J Thorac Imaging 1997;12:38-40.
- Webb EM, Elicker BM, Webb WR. Using CT to diagnose non-neoplastic tracheal abnormalities: appearance of the tracheal wall. AJR Am J Roentgenol 2000;174:1315-21.
- Agust? EB, Vecina VM, Figuerola CR, Monz?n Gasp? M. Tracheal diverticulum: a case report. Acta Otorrinolaringol Esp 2007;58:278-9.
- Polverosi R, Carloni A, Poletti V. Tracheal and main bronchial diverticula: the role of CT. Radiol Med 2008;113:181-9.
- Reitsma W, Visser MJ , Vries FD, Hengel PV. A 64-year-old man with chronic cough and recurrent respiratory? infections. Respiratory Medicine CME. 2010;3:103-5. doi:10.1016/j.rmedc.2009.03.005
- Infante M, Mattavelli F, Valente M, Alloisio M, Preda F, Ravasi G. Tracheal diverticulum: a rare cause and consequence of chronic cough. Eur J Surg 1994;160:315-6.
- Pinot D, Breen D, Peloni JM, Gaubert JY, Dutau H, Vervloet D. An incidental finding in a 34-year-old male under investigation for haemoptysis. Diagnosis: the radiological and endoscopic images demonstrate a complex defect along the posterior tracheal wall consistent with acquire tracheal diverticulum. Eur Respir J 2009;33:1227-9.
Yazışma Adresi (Address for Correspondence)
Dr. Rajendra Prasad Takhar
Government Medical College,
Department of Respiratory Medicine,
KOTA - INDIA
e-mail: drrajtakhar@gmail.com