LETTER TO THE EDITOR
Doi: 10.5578/tt.8062
Tuberk Toraks 2015;63(2):142-144

Uzam?? hava ka?a??n?n endobron?iyal valf ile tedavisi: Olgu sunumu
Erdo?an ?ET?NKAYA1, Zehra YA?AR2, Murat ACAT3
1 Yedikule G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, G???s Hastal?klar? Klini?i, ?stanbul, T?rkiye
1 Clinic of Chest Diseases, Yedikule Chest Diseases and Chest Surgery Training and Research Hospital, Istanbul, Turkey
2 Abant ?zzet Baysal ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Bolu, T?rkiye
2 Department of Chest Diseases, Faculty of Medicine, Abant Izzet Baysal University, Bolu, Turkey
3 Karab?k ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Karab?k, T?rkiye
3 Department of Chest Diseases, Faculty of Medicine, Karabuk University, Karabuk, Turkey
INTRODUCTION
Persistent air leaks are frequent after pulmonary resection, but can occur as a complication of lung diseases especially chronic obstructive lung disease (COPD) (1). It may affect up to 20% of COPD patients (2). Current treatment options of prolonged air leaks involve prolonged tube thoracostomy drainage, pleurodesis, surgical decortication or surgical repair. In patients who are not candidates for surgical treatment, alternative methods can be used such as endobronchial approaches and radiotherapy (3,4). In this case, an endobronchial valve was inserted by flexible bronchoscopy for persistent air leakage, resulting in a complete resolution and lung reexpansion in patient with COPD.
CASE REPORT
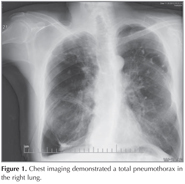
63-year-old male patient applied to emergency clinic with acute-onset dyspnea and substernal chest pain. He had a history of 60 pack-year smoking and ten years before that, he had been first told that he had emphysema and was treated with inhaled bronchodilators. Because of worsening dyspnea, he was treated with bullectomy five years ago. He had been admitted to the hospital for three times with a similar presentation; a spontaneous, right basal pneumothorax and was treated with tube thoracostomy. He was conscious, with vital signs of arterial blood pressure 135/80 mmHg, the heart rate 92 beats per minute, respiratory rate 28 per minute and an oxygen saturation of 89% at room air. There were decreased respiratory sounds in all zones on the right lung auscultation. Chest imaging demonstrated a total pneumothorax in the right lung (Figure 1). On thoracic-computed tomography (CT), bullous areas at the apexes of both lungs and a right pneumothorax were observed (Figure 2). Tube thoracostomy was performed. Although he had clinically improved, there was no improvement of the right pneumothorax, therefore surgery was considered. But this was contraindicated because of his healthy status. Because of prolonged chest drainage causes prolonged hospital stay and many complications; he discharged with drain tube connected to a Heimlich valve. Two weeks after hospital discharge until the patient could tolerate the drain being clamped, negative aspiration and talc pleurodesis were performed twice without satisfactory results. Based on a published report, endobronchial valve was attempted. Baloon catheter was inserted via the working channel of the flexible bronchoscope and balloon inflated on the right upper lobe. With occlusion of the right upper lobe bronchus, the air leak was ceased. 3 Zephyr valve were (4 mm diameter valve in apical and posterior segments, 5.5 mm diameter valve in anterior segment) placed to stop the air leak (Figure 2). After the procedure his health status was improved, he was decanulated and discharged within 1 week. On 7-month follow up, complete expansion of the lung was detected and no pneumothorax was observed.
DISCUSSION
COPD is the common cause of spontaneous seconder pneumothorax and the most consistently identified risk factor for persistent air leak that is detected in 20% of COPD patients (1). Also it is reported in up to 45% of cases who have undergone lung volume reduction surgery due to pulmonary emphysema (5). Persistent air leak may cause a high level of mortality, infectious, cardiopulmonary complications and prolonged hospital stays (3,6). The treatment options are thoracostomy drainage, pleurodesis, surgical decortication, surgical repair, endobronchial valves. Patients with underlying lung disease especially COPD tend to have longer duration of air leaks. If it is lasting longer than seven days surgery procedures should be the first option. In COPD patients, surgical risk is generally much increased like our case. These patients present therapeutic adversities of carrying prolonged chest drainage as increased risk of infections, subcutaneous emphysema, misplacement of the tube and prolonged hospital stays. One of the alternative approach is medical pleurodesis but the study in the literature showed that it has not yet been very effective (7). Local radiotherapy was used in patients with persistent pneumothorax controversial results are reported in previous studies (4,8).
The other encouraging approach is endobronchial treatment such as endobronchial valves (EBV) that can be performed with flexible bronchoscope. EBV prevents air from entering distal airways and allows time for to heal. Traveline and colleagues reported that the EBV was effective for a large number of patients with persistent air leak (3). The previous study showed the use of EBV in two complex medical condition as lymphangiomyomatosis and severe pneumonia with ARDS (9). Detection of air leaking source is important for successful procedure. The most commonly used method is balloon catheter occlusion that inserted through the working channel of bronchoscopy. Balloon inflated and assessed the degree of air leak. The EBV is then deployed to the leaking airways by use of delivering catheter.
The adverse affects may occur in the treatment of pulmonary emphysema with EBV. These complications include pneumothorax, pneumonia of non-involved lobes, COPD exacerbation and pleural effusion. In our case we have not seen any of these complications on 7 month follow-up.
We describe the case of a 63-year-old man who presented with secondary spontaneous pneumothorax and persistent air leak. Implantation of EBV decreased the air leak enough for the chest tube to be removed. These nonsurgical and minimally invasive approaches that may promising for patients with persistent air leak. However, prospective studies are needed to observe the treatment results to validate this approach.
CONFLICT of INTEREST
None declared.
REFERENCES
- Stolz AJ, Schutzner J, Lischke R, Simonek J, Pafko P. Predictors of prolonged air leak following pulmonary lobectomy. Eur J Cardiothorac Surg 2005;27:334-6.
- Videm V, Pillgram-Larsen J, Ellingsen O, Andersen G, Ovrum E. Spontaneous pneumothorax in chronic obstructive pulmonary disease: complications, treatment and recurrences. Eur J Respir Dis 1987;71:365-71.
- Travaline JM, McKenna RJ Jr, De Giacomo T, Venuta F, Hazelrigg SR, Boomer M, et al. Treatment of persistent pulmonary air leaks using endobronchial valves. Chest 2009;136:355-60. doi: 10.1378/chest.08-2389.
- Cetinkaya E, Ozg?l MA, G?l S, Cam E, B?y?kpolat Y. Treatment of a prolonged air leak with radiotherapy: a case report. Case Rep Pulmonol 2012;2012:158371. doi: 10.1155/2012/158371.
- Ciccone AM, Meyers BF, Guthrie TJ, Davis GE, Yusen RD, Lefrak SS, et al. Long-term outcome of bilateral lung volume reduction in 250 consecutive patients with emphysema. J Thorac Cardiovasc Surg 2003;125:513-25.
- Cerfolio RJ, Tummala RP, Holman WL, Zorn GL, Kirklin JK, McGiffin DC, et al. A prospective algorithm for the management of air leaks after pulmonary resection. Ann Thorac Surg 1998;66:1726-31.
- Kilic D, Findikcioglu A, Hatipoglu A. A different application method of talc pleurodesis for the treatment of persistent air leak. ANZ J Surg 2006;76:754-6.
- Kanagasabay RR, Lamb PM, Tait DM, Madden BP. Local radiotherapy for alveolar air leak. J R Soc Med 1999;92:190-2.
- Toma TP, Kon OM, Oldfield W, Sanefuji R, Griffiths M, Wells F, et al. Reduction of persistent air leak with endoscopic valve implants. Thorax 2007;62:830-33.
Yaz??ma Adresi (Address for Correspondence)
Dr. Zehra YA?AR
Abant ?zzet Baysal ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
G?lk?y, BOLU - TURKEY
e-mail: zehraasuk@hotmail.com