RESEARCH ARTICLE
Doi: 10.5578/tt.9015
Tuberk Toraks 2015;63(1):71-77

Akci?er kanserli hastalarda serum VEGF ve Anjiopoietin-2 d?zeyinin prognostik ?nemi
P?nar AKIN KABALAK1, Ayd?n ??LEDA?1, Nalan DEM?R1, G?khan ?EL?K1, Cabir Y?KSEL2, G?zde K?YC?1,
Derya G?KMEN ?ZTUNA3, Abbas TANER4, Ak?n KAYA1, Hakan KUTLAY2, Numan NUMANO?LU5, ?smail SAVA?1
1 Ankara ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara, T?rkiye
1 Department of Chest Diseases, Faculty of Medicine, Ankara University, Ankara, Turkey
2 Ankara ?niversitesi T?p Fak?ltesi, G???s Cerrahisi Anabilim Dal?, Ankara, T?rkiye
2 Department of Chest Surgery, Faculty of Medicine, Ankara University, Ankara, Turkey
3 Ankara ?niversitesi T?p Fak?ltesi, Biyoistatistik Anabilim Dal?, Ankara, T?rkiye
3 Department of Biostatistics, Faculty of Medicine, Ankara University, Ankara, Turkey
4 TOBB ET? T?p Fak?ltesi, Mikrobiyoloji ve Klinik Mikrobiyoloji Anabilim Dal?, Ankara, T?rkiye
4 Department of Microbiology and Clinical Microbiology, TOBB ETU University, Ankara, Turkey
5 TOBB ET? T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara, T?rkiye
5 Department of Chest Diseases, Faculty of Medicine, TOBB ETU University, Ankara, Turkey
?ZET
Akci?er kanserli hastalarda serum VEGF ve Anjiopoietin-2 d?zeyinin prognostik ?nemi
Giri?: Anjiogenezis (neovask?lrizasyon) s?recinde vask?ler endotelyal b?y?me fakt?r? (VEGF) ve Anjiopoietin-2 (Ang-2) en ?nemli anjiogenik mediat?rleridir. ?u ana kadar bu belirte?ler akci?er kanserinde ayr? ayr? ve k???k h?cre d??? akci?er kanseri (KHDAK) i?in ele al?nm??t?r. Bu ?al??mada her iki belirte? KHDAK ve k???k h?creli akci?er kanseri (KHAK) i?in incelenecektir.
Hastalar ve Metod: Tek merkezli y?r?t?len bu ?al??mada 28 adenokanser ve 59 yass? h?creli olmak ?zere toplam 87 KHDAK ve 13 KHAK olmak ?zere toplam 100 hasta al?nm??t?r. Sonu?lar 30 sa?l?kl? g?n?ll?yle kar??la?t?r?lm??t?r. Tedavi ?ncesi al?nan serumlarda belirte? d?zeyleri "enzyme-linked immunosorbent assay (ELISA)" y?ntemiyle ?al???lm??t?r.
Bulgular: Hasta grubunda serum Ang-2 d?zeyi kontrol grubuna g?re anlaml? derecede y?ksek iken (23395 pg/mL - 4025 pg/mL, p< 0.001) serum VEGF d?zeyinde farkl?l?k izlenmedi (2308 pg/mL - 2433 pg/mL, p> 0.05). KHAK ve KHDAK tan?l? hastalarda serum Ang-2 d?zeyleri benzerdi. Ancak VEGF d?zeyi KHAK grupunda, hem KHDAK hem de kontrol grubuna g?re anlaml? derecede d???kt?. Her iki belirte? de h?cre tipi, t?mor boyutu, TNM evrelemesi, performans durumu ve operasyona uygunluk a??s?ndan korelasyon g?stermedi. Kronik obstr?ktif akci?er hastal??? (KOAH) olan olgularda VEGF d?zeyi, anlaml? olmamakla beraber KOAH tan?s? olmayanlara g?re daha y?ksekti. Youden index kullan?larak belirlenen sensitivite ve spesifiteye g?re ?? s?n?r de?er belirlendi. Bu de?erler? 8515.73 pg/mL (duyarl?l?k %78, ?zg?ll?k %76), 7097 pg/mL (duyarl?l?k %80, ?zg?ll?k %70) ve 11063.48 pg/mL (duyarl?l?k %76, ?zg?ll?k %70) olarak belirlendi. KHAK' l? hastalar t?m s?n?r de?erlerin ?zerinde daha k?t? prognoz g?sterdi (p> 0.05). VEGF ve Ang-2 zay?f ancak pozitif y?nde korelasyon g?sterdi (p= 0.1 ve r= 0.638).
Sonu?: ?al??mam?zda VEGF d?zeyi akci?er kanseri erken tan?s?, prognoz veya h?cre tipi a??s?ndan yol g?sterici izlenmezken Ang-2 ay?r?c? tan?da anlaml? bulunmu?tur. Serum d?zeyindeki ?al??ma sonu?lar?ndaki heterojenite nedeniyle t?m?r dokusunda yap?lacak ?l??mler daha yol g?sterici olabilir.
Anahtar kelimeler: Akci?er kanseri, anjiogenezis, serum belirte?leri, ya?am beklentisi
SUMMARY
Prognostic significance of serum vascular endothelial growth factor and angiopoietin-2 in patients with lung cancer
Introduction: Vascular endothelial growth factor (VEGF) and Angiopoietin-2 (Ang-2) are major angiogenic mediators in neovascularization process. In current literature both biomarkers are discussed separately and only for non-small cell lung cancer (NSCLC). So in this study we aimed to examine them together for both cell types NSCLC and small cell lung cancer (SCLC).
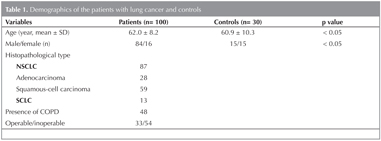
Patients and Methods: 100 patients with lung cancer were enrolled to this single center study. 87 of patients were diagnosed with NSCLC including 28 adenocarcinomas and 59 squamous cell cancers and 13 were SCLC. Results were compared with 30 healthy volunteers. Pre-treatment serum VEGF and Ang-2 levels were measured by using ELISA method.
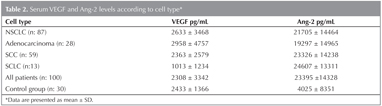
Results: While serum Ang-2 levels were higher in patients than healthy controls (23395 pg/mL vs. 4025 pg/mL, p< 0.001), VEGF levels didn't differ (2308 pg/mL vs. 2433 pg/mL, p> 0.05). There was no difference between cases with SCLC and NSCLC in terms of Ang-2. But serum VEGF values were significantly lower in SCLC than NSCLC and control groups. None of these mediators were correlated with cell type, tumor size, TNM staging, performance status and operability. VEGF levels were higher in patients with chronic obstructive pulmonary disease (COPD), but it was not significant. Three cut of values were determined according to sensitivity and specificity by using youden index. They were 8515.73 pg/mL (sensitivity 78%, specificity 76%), 7097 pg/mL (sensitivity 80%, specificity 70%) and 11063.48 pg/mL (sensitivity 76%, specificity 70%). Patients with SCLC had shorter survival time above cut-off values (p> 0.05). VEGF and Ang-2 showed a weak positive correlation (p= 0.1 and r= 0.638).
Conclusion: In conclusion, serum VEGF wasn't useful to predict lung cancer, prognosis or cell type. Albeit Ang-2 was higher in patients with lung cancer without any effect on survival. Due to the heterogeneity of the studies done with serum measurement Ang-2 on tumor tissue should be more meaningful.
Key words: Angiogenesis, lung cancer, serum biomarkers, survival
INTRODUCTION
Angiogenesis is an essential process for human physiological circumstances that goes on in balance of angiogenic and anti-angiogenic factors. Angiogenesis also promotes tumor progression and metastasis, because a tumor cell needs new vascular supply to growth and persist (1). Tumor associated angiogenesis proceed in two phases included angiogenic switch (prevascular phase) and vascular phase (2).
Angiopoietins have been defined in the mid-1990s as a potent angiogenic factors including 4 isoforms called Ang-1, 2, 3 and 4. Ang-1 and Ang-2 are the best identified of them. They act as ligands for Tie-2 that a tyrosine kinase receptor and expressed on endothelial cells plays a major role in this process together with VEGF (3). While Ang-1 stabilizes vessel structure, Ang-2 antagonizes Ang-1's effect by binding Tie-2 receptor competitively. Existence of VEGF is essential for tumoral angiogenesis regulating by Ang-2. Vessels destabilized by Ang-2 may be regress in the absence of VEGF and others angiogenic factors. Thus neovascularization is a dynamic process controlling with many factors (4).
Vascular endothelial growth factor is major, potent and well-defined angiogenic molecule. It has affinity to tyrosine kinases receptor on endothelial cell same as Ang-2 (3). As other malignancies, VEGF levels get higher both serum and tumor tissue in lung cancer cases. According to a study with forty patients with lung cancer serum VEGF levels were significantly higher than twenty-five healthy volunteers (5). In another analyses with seventy-five NSCLC patients, above cut-off value of 119 pg/mL prognosis significantly decreased compared to values under 119 pg/mL (6).
Angiopoietin-2 is detected high in various malignancies such as prostate, thyroid, acute myeloid leukemia. Lung cancer is one of these malignancies studied in concert with Ang-2. Its' significance regarding with VEGF in lung cancer has not been investigated enough (7). Knowledges are focusing on especially NSCLC.
We aimed to determinate the levels of VEGF and Ang-2 in patients with lung cancer, and to evaluate an association between these angiogenic factors and clinical, pathologic characteristics and survey of these patients.
PATIENTS and Method
This study was designed with a hundred patients diagnosed lung cancer between 2009 and 2011. 30 healthy adults (15 male, 15 female, median age 60 years) were accepted as control group. None of healthy volunteers had a chronic disease that requires regular drug use and/or symptom of malignancies.
Serum samples were collected from patients before any treatment, venous blood samples were spun at 3000 revolutions per minute for 10 minutes. Supernatant was placed into 2 cc eppendorf tubes after centrifugation and stored at -80?C deep freeze until the measurement. Enzyme-linked immunosorbent assays (ELISA) were used for measurements of VEGF and Ang-2 (RayBio? Human VEGF ELISA Kit and E90009Hu 96 Tests Enzyme-linked Immunosorbent Assay Kit for Angiopoietin 2).
Various methods were used for diagnosis of lung cancer. Bronchoscopy and fine needle aspiration methods were performed in most of the cases. Thoracentesis, sputum cytology, surgery were used less frequently for the diagnosis. TNM staging was done according to International Association for the Study of Lung Cancer (IASLC) - 7th editions (3,8). Eastern Cooperative Oncology Group (ECOG) performance status, age, sex, smoking status (pack-year), hemogram, biochemical parameters (lactate dehydrogenase and calcium) and coexistence of chronic obstructive pulmonary disease (COPD) are recorded for each patient (9). Chemotherapy had been administered inoperable patients according to treatment protocols.
Survival analyses of the patients were investigated by following up to fifteen months.
Study protocol was approved by ethical committee and all participants were informed about study design (Ethics committee decision number 16-350 and date 4.10.2010).
Statistical Analysis
Statistical software (SPSS for Windows version 11.5 SPSS) was used for the analyses. Variables that obtain by measurement are given as mean ? SD, for counting parameters frequency distribution was used as descriptive statistics. The Mann Whitney U test was used to compare patients and control group. For analyses of variance Kruskal-Wallis test was used. Spearman correlation of rank coefficient was used to analyze correlations between parameters. To assess whether mediators are useful to make discrimination between control and healthy group the area under curve of operating characteristic was used. The most appropriate cut-off values were taken by using Youden index. Survival analyses were performed by Kaplan-Meier method and p< 0.05 was considered statistically significant.
Results
Age distribution of patients was similar between study and control group. Squamous cell was the most frequent cell type with 59 patients. Nearly half of patients had COPD (n: 48) (Table 1).
Comparison of Serum Ang-2 and VEGF Levels Between Patient and Control Groups
While the serum Ang-2 levels were higher in patients with lung cancer (23395 pg/mL) than control group (4025 pg/mL) (p< 0.001), there was no difference between subjects and controls for VEGF (2308 pg/mL vs. 2433 pg/mL, p> 0.05) (Table 2).
Both of serum biomarkers had no relation with LDH, serum calcium and performance status.
Comparison of Serum VEGF on Cell Type
and Correlation with Ang-2
There was no notable difference between SCLC and NSCLC groups with respect of serum Ang-2 levels (p= 0.4). When considering only NSCLC patients Ang-2 level was minimal higher in SCC than adenocarcinoma. As mentioned above, VEGF was not appropriate to distinguish patients and controls. Nonetheless, mean VEGF levels were significantly lower in SCLC than NSCLC and control patients (p= 0.005 and p= 0.003). Serum Ang-2 and VEGF levels according to histopathological type of lung cancer were shown in Table 2.
Smoking Status, Existence of COPD in Subjects
and VEGF and Ang-2 Levels
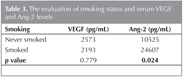
Ang-2 was related with smoking. It was higher in smokers (p= 0.024) but amount of pack-year wasn't associated with Ang-2 (Table 3).
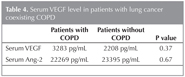
Because of CODP is a risk factor for lung cancer, we evaluated Ang-2 and VEGF levels according to the existence of COPD in patients with lung cancer. At the end of this analysis, we observed that serum VEGF levels were higher in patients with COPD than patients without COPD, but it was statistically insignificant (Table 4). Ang-2 levels were similar between patients with and without COPD.
Evaluation of Serum Ang-2 and VEGF Levels in
Terms of TNM Staging and Operability
When Ang-2 and VEGF levels were analyzed according to staging of lung cancer in all patients, the tumor size (T) or lymph node involvement (N) were not correlated with serum biomarker levels. In cases with M1b had more elevated serum VEGF and Ang-2 levels. However, it was no significant, statistically (p= 0.1 and p= 0.5, respectively). Except of SCLC - extensive disease, in all patients with lung cancer serum Ang-2 and VEGF levels showed a poor, positive correlation without significance. Especially stage IIA showed highest correlation (p= 0.1, r= 0.638).
The number of metastatic regions did not affect serum levels of these mediators. In patients with NSCLC, operability showed no effect on serum VEGF and Ang-2 levels.
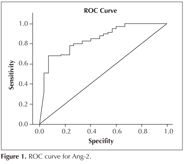
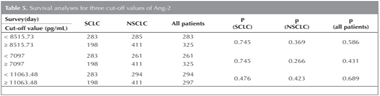
Association of Serum Ang-2 with Survival
Ang-2 levels were evaluated for survival time due to its' significance compared with control group (Figure 1). Three cut of values were determined according to sensitivity and specificity. They were 8515.73 pg/mL (sensitivity 78%, specificity 76%), 7097 pg/mL (sensitivity 80%, specificity 70%) and 11063.48 pg/mL (sensitivity 76%, specificity 70%) (Table 5).
In group of patients with NSCLC, there was no relation between survival days and Ang-2 levels; however, the patients with SCLC got lower above all cut-off values (p> 0.05). When the type of lung cancer was analyzed; the cases with adenocarcinoma had lower survival days under all cut-off values especially according to value off 11063.48 pg/mL (p= 0.967). While above value of 11063.48 pg/mL mean survival was 164 days, below this value mean survival was 385 days.
There was no statistically significant difference between operable and inoperable groups with respect to Ang-2 levels; however, survival time of inoperable group was low above all cut-off values without significance. Similarly coexistence of COPD (n= 42) was related to poor prognosis without any significance (p> 0.05).
DISCUSSION
Due to the lack of screening method for early diagnosis, lung cancer is still mortal at the present time (1). Although smoking cessation treatments and awareness of people are increased, new angiogenic mediators are needed to be investigated. Because of angiogenesis is main pathway for tumor development and distant metastasis, the determination of thoroughly validated predictive biomarkers for lung cancer may help to stratify cancer patients and to monitor tumor progression and response to the therapy.
In the view of the previous studies emphasizing the importance of angiogenic mediators, Ang-2 that functioning by tyrosine kinase and activated by existence of VEGF in patients with lung cancer was investigated were evaluated in this study. Literature is overviewed to date; it's known that serum Ang-2 and VEGF levels have been found higher in patients with lung cancer than healthy controls. In contrast to this, there have also been few studies that elevated VEGF and Ang-2 levels could not determine in such patients. Our measurements showed significant differences from control group for Ang-2 levels of patients with lung cancer, but VEGF didn't show any difference as similar to a study (4). This result may explain with some possible mechanisms: All angiogenic factors and their receptors are produced in tumor cell. In tumor tissue vascular density and angiogenic mediators show heterogeneity. Furthermore VEGF has six isoforms and VEGF189, VEGF206 aren't detectable in serum although they are secreted by tumor tissue. So a tumor tissue couldn't be supposed to release mediators as high as expected. This diversity may affect to the studies done with sera (8,10).
In this study, VEGF levels could not be used as a determinant factor for differentiation of cell type of the patients with lung cancer. When Ang-2 levels were evaluated according to the cell type of subjects, there was no difference between SCLC and NSCLC patients. Adenocarcinoma and squamous cell carcinoma were included to present study within the NSCLC group. In a study designed with 136 patients with NSCLC, VEGF and Ang-2 levels were not found differ between the patients with squamous cell carcinoma and adenocarcinoma (4). Consequently angiogenesis process in NSCLC doesn't seem to show any differences according to the cell type. So it seems to be hard to determine any cut-off values for mediators suitable to predict cell type. But in our study it was noticeable that serum Ang-2 and VEGF levels were lower in SCLC group than NSCLC, significantly. We had limited number of SCLC patients (n= 13) where as there were 87 of NSCLC. When we consider only patients with NSCLC, the results of the study didn't change.?
According to available data, existence of COPD and smoking are affecting to the serum VEGF and Ang-2 levels due to inflammatory process (9,11,12,13). In present study, approximately a half of patients and controls were active smoker, but none of healthy volunteers had COPD. Smoking was found to be related with elevated Ang-2 levels regardless of pack-year. However, VEGF levels were not correlated with smoking status of patients with lung cancer, when it was compared to the controls. Why there was no statistically a difference compared to controls for VEGF might be associated with bronchial wall damage due to smoking. But this reason could not help to us to explain the elevated Ang-2 levels in smoker patients with lung cancer. In COPD group, both of mediators were higher than patients without COPD and this elevation was more remarkable for VEGF without significance. Earlier studies have shown that patients with COPD had high VEGF level on bronchial epithelial and it causes pulmonary hypertension in time. Using inhaled corticosteroid and beta-2 agonist treatments were shown to be responsible decreasement of VEGF by in vitro studies (12). In our study it is a limitation that we couldn't consider if a patient is in exacerbation period or using inhaled drug. These limitations could be another reason why VEGF didn't differ between study and control group. Smoking and existence of COPD have an important role in carcinogenesis, so the relationship of these conditions and serum Ang-2 and VEGF levels should be investigated carefully in patients with lung cancer.?
Previous studies showed that serum levels of Ang-2 and VEGF levels were increased significantly according to stage progression. However, another studies showed that Ang-2 levels were associated with stage progression without VEGF relation (4,6,10). Additionally, some studies that serum VEGF level was not an independent factor for survival have been published in the literature (14). Nonetheless, a study shown that Ang-2 was a useful clinical marker for detecting NSCLC with distant metastasis and it was of potential prognostic value in contrast to VEGF (4). In another study including 236 patients with NSCLC, positive Ang-2 expression had been found related to poor prognosis (10). In contrast to these previous studies showing Ang-2 and VEGF can be correlated with staging and prognosis, we determine three cut of values according to sensitivity and specificity for Ang-2. Patients with SCLC survival decreased above all cut-off values without significance but it would be more accurate to connect this result to aggressive nature of this cell type. In NSCLC group survival weren't related to mediator's level.
VEGF and Ang-2 levels were not affected to the tumor size, lymph node involvement, staging, the number of distant metastasis and operability in present study as previous studies (4,5).
CONCLUSION
In conclusion, we observed that VEGF wasn't useful to predict lung cancer, prognosis or cell type when measured in serum. Although Ang-2 was useful for differential diagnosis it had no effect on survival. Tumor angiogenesis is a complicated process because of heterogeneity of tumor tissue. Because of variability in mediator release it should be more significant to study mediators on tumor tissue.
Acknowledgment
This study was supported by Ankara University Scientific Research Project Unit (Project number: 10A3330009).
CONFLICT of INTEREST
None declared.
REFERENCES
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011;61:134.
- Mc Mahon G. VEGF Receptor Signaling in Tumor Angiogenesis. The Oncologist 2000;(Suppl 1):S3-S10.
- Thomas M, Augustin HG. The role of the angiopoietins in vascular morphogenesis. Angiogenesis 2009;12:125-37.
- Park JH, Park KJ, Kim YS, Sheen SS, Lee KS, Lee HN, et al. Serum angiopoietin-2 as a clinical marker for lung cancer. Chest 2007;132:200-6.
- Sa?lam DA, Ursava? A, Karada? M, Yilmaztepe Oral A, Co?kun F, G?z? RO. The evaluation to relationship between serum vascular endothelial growth factor (VEGF) level, metastases and other tumor markers in patients with lung cancer. Tuberk Toraks 2008;56:50-5.
- Kaya A, Ciledag A, Gulbay BE, Poyraz BM, Celik G, Sen E, et al. The prognostic significance of vascular endothelial growth factor levels in sera of non-small cell lung cancer patients. Respir Med 2004;98:632-6.
- Tabernero J. The role of VEGF and EGFR inhibition: implications for combining anti?VEGF and anti?EGFR Agents. Mol Cancer Res 2007;5:203-20.
- Tanaka F, Ishikawa S, Yanagihara K, Miyahara R, Kawano Y, Li M, et al. Expression of angiopoietins and its clinical significance in non-small cell lung cancer. Cancer Res 2002;62:7124-9.
- Park JE, Keller GA, Ferrara N. The vascular endothelial growth factor (VEGF) isoforms: differential deposition into the subepithelial extracellular matrix and bioactivity of extracellular matrix-bound VEGF. Mol Biol Cell 1993;4: 1317-26.
- Pavlisa G, Pavlisa G, Kusec V, Kolonic SO, Markovic AS, Jaksic B. Serum levels of VEGF and bFGF in hypoxic patients with exacerbated COPD. Eur Cytokine Netw 2010;21:92-8.
- Cho YJ, Ma JE, Yun EY, Kim YE, Kim HC, Lee JD, et al. Serum angiopoietin-2 levels are elevated during acute exacerbations of COPD. Respirology 2011;16:284-90.
- Feltis BN, Wignarajah D, Reid DW, Ward C, Harding R, Walters EH. Effects of inhaled fluticasone on angiogenesis and vascular endothelial growth factor in asthma. Thorax 2007;62:314-9.
- Kanazawa H, Asai K, Tochino Y, Kyoh S, Kodama T, Hirata K. Increased levels of angiopoietin-2 in induced sputum from smoking asthmatic patients. Clin Exp Allergy 2009;39:1330-7.
- Chakra M, Pujol JL, Lamy PJ, Bozonnat MC, Quantin X, Jacot W, et al. Circulating serum vascular endothelial growth factor is not a prognostic factor of non-small cell lung cancer. J Thorac Oncol 2008;3:1119-26.
Yaz??ma Adresi (Address for Correspondence)
Dr. P?nar AKIN KABALAK
Ankara ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
Cebeci, ANKARA - TURKEY
e-mail: pinarakinn@yahoo.com