LETTER TO THE EDITOR
Doi: 10.5578/tt.8126
Tuberk Toraks 2015;63(1):62-64

Nadir g?r?len bir bron?ektazi nedeni
Fatma ??FTC?1, Ayd?n ??LEDA?1, Ak?n KAYA1
1 Ankara ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara, T?rkiye
1 Department of Chest Diseases, Faculty of Medicine, Ankara University, Ankara, Turkey
A 34-year-old woman presented to our clinic with a 5-year history of cough, sputum, dyspnea on exercise, and wheezing. She had no history of exposure to occupational pollutants but had a smoking history of 5 packs/year. She also complained of recurrent lower respiratory infections in winter.
Her vital signs included a blood pressure of 110/60 mm/Hg, pulse rate of 80 bpm, respiratory rate of 16/min, body temperature of 36.7?C, and oxygen saturation of 96% on room air. Her respiratory system examination revealed bilateral sonor rhonchi. Extremity examination revealed yellowish discoloration, thickening, onycholysis, and loss of lunula and cuticle of fingernails and toenails (Figure 1). There was also minimal non-pitting pretibial edema in both lower extremities. The patient told that her nails were yellowish in color since birth. Laboratory tests revealed the following: Hematocrit level %34.5, sedimentation rate 38 mm/hour, CRP 13.8 mg/L. White blood count, platelet count, coagulation profile, liver and renal function tests, blood glucose, and urinalysis were all normal. Respiratory function tests showed a FEV1 of 67% of expected, a FVC of 78% of expected, a FEV1/FVC ratio of 0.66, and a carbonmonoxide diffusion capacity of 78% of expected.
Chest X-ray was characterized by a linear reticular density increase and an ectatic pattern in lower zones.
Thorax high resolution computed tomography showed prominent mosaic perfusion pattern in lower zones of both lungs, bronchiectasis and centraciner micronodules causing tree-in-bud appearance in middle lobe, lingula, and both lower lobes, and subsegmental atelectases in middle lobe and lingula (Figure 2). Gram-positive diplococci proliferated in sputum culture. Tuberculin skin test was negative. Sputum acid-fast bacteria staining was also negative. No tuberculosis bacilli proliferation was detected in sputum culture.
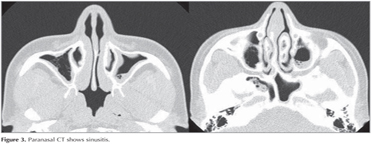
Paranasal CT revealed mucosal thickening as well as soft tissue densities consistent with sinusitis in the mucosa of maxillary, ethmoidal, sphenoidal, and frontal sinuses (Figure 3). Dermatological examination revealed no fungal infection of nails.
The patient was started on oral amoxicillin clavulonic acid, fluconazole, inhaler bronchodilators and oral Vitamin E. She also underwent postural drainage and chest phyisotherapy.
The yellow nail syndrome was first described by Samman and White in 1964 (1). In 1972 Hiller et al. described that the presence of two features of the classicial triad of yellowish nails, lymphedema, and respiratory system involvement would be sufficient to establish the diagnosis (2). In addition to yellowish discoloration of nails, there may also be lack of finger growth, finger cambering and thickening, onycholysis, and lunula and cuticle loss. It may be seen in all ages and affects both sexes equally. In the past it was thought that it had an autosomal dominant inheritance pattern; however, only a small minority of affected persons reveal a positive family history (3). Some autoimmune and malignant disorders may accompany the clinical picture.
As for its etiopathogenesis, lymphatic obstruction hypothesis was first proposed by Samman and White in 1964 and is thought to primarily underlie the disease (1). Other theories include microvascular leakage and hypoplasia of lymphatic channels (4,5).
Respiratory involvement may be characterized by pleural effusion as well as bronchiectasis and rhinosinusitis (6,7). Respiratory function tests may show a normal or combined restrictive and obstructive pattern. Lymphoedema is the initial symptom in one-third of cases. It usually affects the upper or lower limbs.
The treatment of yellow nail syndrome consists of symptomatic therapies. There are case reports in which local steroid injection, oral vitamin E (800 U bid for 18 months), topical vitamin E (5% solution bid), oral zinc supplementation, oral anti-fungals, and intra-lesional triamcinolone injections) were successfully used (8). The management of bronchiectasis include maintenance of pulmonary hygiene, postural drainage and chest physiotherapy. Lymphedema may benefittight bandage, diuretic, exercise, and external pneumatic compression. Pleural fluid may be treated with pleurodesis, pleurectomy, and pleuroperitoneal or pleurovenous shunt (9).
In conclusion, yellow nail syndrome should be remembered as a rare cause in the differential diagnosis of bronchiectasis. The affected cases should definitely be evaluated with a high resolution computed tomography. Any potential accompanying autoimmune or malignant disorders should be sought for and ruled out.
CONFLICT of INTEREST
None declared.
Geli? Tarihi/Received: 08.08.2014 • Kabul Edili? Tarihi/Accepted: 21.08.2014
REFERENCES
- Samman PD, White W. The ?yellow nail? syndrome. Br J Dermatol 1964;76:153-7.
- Hiller E, Rosenow EC 3rd, Olsen AM. Pulmonary manifestations of the yellow nail syndrome. Chest 1972;61:452-8.
- Hoque SR, Mansour S, Mortimer PS. Yellow nail syndrome: not a genetic disorder? Eleven new cases and a review of the literature. Br J Dermatol 2007;156:1230-4.
- D'Alessandro A, Muzi G, Monaco A, Filiberto S, Barboni A, Abbritti G. Yellow nail syndrome: does protein leakage play a role? Eur Respir J 2001;17:149-52.
- Bull RH, Fenton DA, Mortimer PS. Lymphatic function in the yellow nail syndrome. Br J Dermatol 1996;134:307-12.
- Vamey VA, Cumberworth V, Sudderic R, Durham SR, Mackay IS. Rhinitis, sinusitis and the yellow nail syndrome: a review of symptoms and response to treatment in 17 patients. Clin Otolaryngol 1994;19:237-40.
- Wiggins J, Strickland B, Chung KF. Detection of bronchiectasis by high-resolution computed tomography in the yellow nail syndrome. Clin Radiol 1991;43:377-9.
- Williams HC, Buffham R, du Vivier A. Successful use of topical vitamin E solution in the treatment of nail changes in yellow nail syndrome. Arch Dermatol 1991;127:1023-8.
- Glazer M, Berkman N, Lafair JS, Kramer MR. Successful talc slurry pleurodesis in patients with nonmalignant pleural effusion. Chest 2000;117:1404-9.
Yaz??ma Adresi (Address for Correspondence)
Dr. Fatma ??FTC?
Ankara ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
Ankara - TURKEY
e-mail: fatmarslann@yahoo.com