RESEARCH ARTICLE
Doi: 10.5578/tt.8799
Tuberk Toraks 2015;63(1):31-36

?st solunum yolu rezistans? sendromu (UARS) tan?s?nda yeni bir yakla??m: PAP y?ntemi
O?uz K?KT?RK1, Ay?e BAHA1, Asiye KANBAY2
1 Gazi ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara, T?rkiye
1 Department of Chest Diseases, Faculty of Medicine, Gazi University, Ankara, Turkey
2 ?stanbul Medeniyet ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?stanbul, T?rkiye
2 Department of Chest Diseases, Faculty of Medicine, Istanbul Medeniyet University, Istanbul, Turkey
?ZET
?st solunum yolu rezistans? sendromu (UARS) tan?s?nda yeni bir yakla??m: PAP y?ntemi
Giri?: ?st solunum yolu rezistans? sendromu (UARS); apne veya hipopneye yol a?madan, ?st solunum yolunda rezistans art??? sonucu, toraks i?i bas?n?ta belirgin art??a yol a?an ve sonunda s?k tekrarlayan arousallarla sonlanan, g?nd?z a??r? uyku hali ve kardiyovask?ler problemlerle karakterize bir sendromdur. Klasik polisomnografik incelemeyle tan?s? s?kl?kla g?zden ka?an bu sendrom, yanl??l?kla ?o?u kez basit horlama veya idiyopatik hipersomni tan?s? almakta ve ne yaz?k ki tedavi edilememektedir. Ger?ek tedavi se?ene?i olan pozitif hava yolu bas?nc?n?n (PAP), tedaviden-tan?ya y?ntemiyle hastal???n tan?s?nda da kullan?labilece?i, bu y?ntemle y?ksek titrasyon bas?nc? saptanan hastalar?n UARS tan?s? alabilece?i, ayn? zamanda tedavi bas?nc?n?n da belirlenmi? olaca?? sav?ndan hareketle bu ?al??ma planland?.
Materyal ve Metod: Apne hipopne indeksi (AH?) 5'in ve artm?? solunumsal ?aba ile ili?kili arousal (RERA) 20'nin ?st?nde, g?nd?z a??r? uyku hali (GAUH) olan, uyku s?resince oksijen desat?rasyonu saptanmayan 30 hastaya UARS ?n tan?s? ile PAP titrasyonu yap?ld?.
Bulgular: PAP titrasyonuyla y?ksek bas?nca ihtiya? duymad??? g?r?lerek UARS d???n?lmeyen 3 hasta ?al??ma d??? b?rak?ld?. ?al??maya dahil edilen 30 hastadan 16 (%53.3)'s? kad?n, 14 (%46.7)'? erkek ve ya? ortalamas? 46.4 ? 9.9 idi. Ortalama beden kitle indeksi (BK?) 26 ? 3.3 olan hastalar?n, Epworth uykululuk anketi puan ortalamas? 15 ? 3.9, ortalama AH?: 2.3 ? 1.4 ve ortalama RERA: 26.1 ? 4.9 bulundu. Ortalama PAP bas?nc? 7.1 ? 1.1 cmH2O olarak titre edildi. Mevcut bulgular ?????nda UARS d???n?len hastalarda PAP titrasyonu s?ras?nda y?ksek PAP de?erleri elde edilmesi, ?st solunum yolunda rezistans art???n?n delilidir.
Sonu?: PAP de?erleri normal bulunan hastalarda ise UARS tan?s? ekarte edilmi?tir. Bu y?ntemin UARS tan?s?n? kesinle?tirmede kan?ta dayal? t?p a??s?ndan anlaml? oldu?u d???n?lmektedir. Tedaviden-tan?ya protokol? ile uygulad???m?z PAP y?ntemi ile ayn? zamanda hastalar?n ihtiya? duyduklar? tedavi bas?nc? da belirlenmektedir. Bu hastalar?n PAP tedavisi alt?nda uzun s?reli takipleri sonucu klinik yan?tlar?n?n de?erlendirilmesi ve daha y?ksek say?da hasta i?eren serilerin sa?lanmas? ?y?llard?r ??z?lemeyen sorunlar? ?eklinde tan?mlanan bu sendromun tedavisine b?y?k katk? sa?layacakt?r.
Anahtar kelimeler: ?st solunum yolu rezistans? sendromu, PAP tedavisi, yeni tan?sal y?ntem
SUMMARY
A new approach in the diagnosis of upper airway resistance syndrome (uars): pap method
Introduction: Upper airway resistance syndrome (UARS) is characterized by repeated number of arousals at night, and excessive daytime sleepiness or somnolence (EDS). It is often missed in classical polysomnographic diagnostic approaches and misdiagnosed as simple snoring or idiopathic hypersomnia, thereby is often left untreated. We propose that positive airway pressure (PAP), which has shown to be effective against UARS, can be used as a diagnostic tool as well. The study designed to test whether patients with high titration pressures can be diagnosed for UARS, and whether this pressure can be used as the treatment pressure in UARS.
Materials and Methods: This study is a retrospective cohort study. The patients with the following selection criteria: apnea hypopnea index (AHI) < 5, respiratory effort related arousal (RERA) index > 20, excessive daytime sleepiness or somnolence (EDS) without nocturnal oxygen desaturation levels were included to the study. After diagnostic polysomnography (PSG), PAP titrarion was applied to diagnose and treatment.
Results: Fourteen (%46.7) of the patients were male, 16 (%53.3) were female, with a mean age of 46.4 ? 9.9 and mean body mass index (BMI) of 26 ? 3.3. The patiens had a mean Epworth sleepiness scale 15.3 ? 3.9, mean AHI: 2.3 ? 1.4 and average RERA: 26.1 ? 4.9. The mean CPAP titration pressure was 7.1 ? 1.1 cmH2O.
Conclusion: In the light of current findings, during PAP titration patients required high pressures is the evidence of increased upper airway resistance in UARS. Using the from therapy to diagnosis protocol, the PAP protocol determines the individual therapeutic pressures needed by patients. Following up the clinical outcomes of these patients under the PAP treatment, and including a larger cohort will contribute greatly to treating this syndrome, defined as one of the "unresolved problems in years".
Key words: Upper airway resistance syndrome, PAP treatment, new diagnostic procedure
Geli? Tarihi/Received: 18.09.2014 • Kabul Edili? Tarihi/Accepted: 04.01.2015
INTRODUCTION
The upper airway resistance syndrome (UARS) has been described based on the hypothesis that snoring and repetitive occurrence of RERAs without oxygen desaturation might cause a significant disease with symptoms, altered quality of life and cardiovascular morbidity. The syndrome was first defined in pediatric patients in 1982 and in adult patients in 1993 by Guilleminault (1). Although the description of RERA, American Academy of Sleep Medicine (AASM) has not accepted UARS as a distinct disease among sleep braething disorders. AASM has concluded that the current clinical and pathophysiological data are not sufficient to specifying UARS as a distinct conditon but instead defined it as borderline of Obstructive Sleep apnea (OSA). The International Classification of Sleep Disorders II's (ICSD II) 2005 version is consistent with the AASM in the matter. It is still controversial whether UARS, with its strong relationship with cardiovascular complications, needs to be regarded as a distinct disease (1,2). With UARS various neuropsychiatric symptoms such as Bruxism, irritable bowel syndrome, insomnia, and somatic problems as well as excessive daytime sleepiness, and major cardiovascular problems are known to occur (3,4,5).
We believe that UARS is a different disease from OSA, as it triggers sympathetic nervous system activation without causing apnea/hypopnea and desaturation. We also believe that UARS should be recognized as a disease that need to be treated, because its results in fatigue and excessive daytime sleepiness (EDS) and, has major cardiovascular consequences. Although there exists globally accepted criteria that can help us in UARS diagnosis, many patients remain undiagnosed and this group can not taken under the essential treatment (Table 1).
Based on these ideas, we set out to investigate a new method that will be cost and time-effective in patients where classical PSG points to a possibe UARS. Detection of increase in upper respiratory tract resistance will confirm of the diagnosis and the need for treatment.
This study was planned with the idea that, using treatment-diagnostic method, positive airway pressure (PAP) can be useful in diagnosing the disease and could also be used to determine the treatment pressure in the same session.
MATERIALS and METHODS
Patient Selection
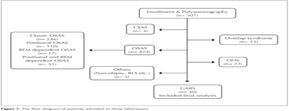
The study was approved by the Ethics Committee of Gazi University. The study population consisted of participants recruited in the Sleep Disorders Centre of Gazi University School of Medicine between January 2008 and December 2012, who were referred for a clinically indicated sleep study 507 patients were examined with PSG (Figure 1). The patients were classified as UARS according to criterias in Table 1.
Polysomnographic Studies
PSG was performed to patients admitted with complaints of snoring and excessive daytime sleepiness. The data from all patients were collected at our AASM-accredited sleep laboratory, all night, using a 16-channel polysomnography (Sensormedics Alpha is Somnost system, Sensormedics, CA, USA). During recording, central and occipital electroencephalogram, bilateral electrooculogram, submental and tibial electromyogram, and electrocardiogram were used. Nasal air flow was measured by pressure transducer. Tracheal sounds were monitored with a microphone. Thoracoabdominal belts were used in the measurement of thorax and abdomen movements. Monitoring of oxygen saturation was performed with noninvasive methods using pulse oximetry. The test was terminated after 6-8 hours of recording. Rechtschaffen and Kales sleep staging and scoring criteria were used from the beginning of sleep was out of the 30-second epochs (6).
All patient scoring were carried out by a nurse working in the center with Sleep Technician Certification and 12 years of experience. In accordance with AASM 2007 criteria, increases in respiratory effort that last for at least ten seconds or airflow limitations that lead to arousal but not met apnea or hypopnea criteria, were defined as RERA. PAP titration was performed on patients with verified EDA and with AHI < 5', RERA> 20' at PSG, with no desaturation, and with a score over 10 in the Epworth Sleepiness Questionnaire (Johns, 1991). PAP titration was performed on patients who showed no impediment for a PAP titration upon an upper respiratory tract examination.
PAP Titration
Auto-PAP titration was performed along with PSG to patients who met the aforementioned criteria by Res Med AutoSet T 1999 model.
Patients with average pressure over 4 cmH2O during titration were considered to have increased resistance of the upper respiratory tract.
Endpoint
In healthy individuals the upper respiratory tract pressure does not exceed 4 cmH2O. PAP titration values over this pressure is the best proof that there is an increase in resistance on the patient's upper respiratory tract.
Primary endpoint: On a patient that we demonstrate an upper airway resistance increase, if the OSA criteria are not met (AHI < 5 and no desaturation) and the patient experiences excessive daytime sleepiness, this patient can be diagnosed to have UARS (Table 1).
Secondary endpoint: It is widely accepted all over the world that diseases with major cardiovascular complications should be treated. UARS also causes this complication and we believe that this is the absolute indication for treatment. We know that nowadays the most effective treatment of upper airway pressure increase is PAP. The prerequisite for PAP therapy to patients is to determine the pressure they need and the methods we use for this purpose is the PAP titration.
After demonstrating increased resistance in the upper airway for the diagnosis of UARS by PAP titration we also learn positive pressure that the patient needs for therapy at the same time. So this means we can offer the patient the diagnosis and treatment options in the same session.
This method eliminated the need for invasive and untolerated methods like esophageal pressure measurement, which is used to make a definitive diagnosis of UARS. PAP method is more effective in terms of cost, more comfortable for the patient and less time-consuming for both the patient and the physician.
Statistical Analysis
The data obtained in the study were evaluated using the SPSS 16.0 package program. Statistical analysis of the cases demographics, polysomnographic recording results and descriptive statistics were used in the evaluation of PAP titration results. Results were given as mean values accompanied by standard deviation.
RESULTS
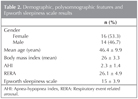
Thirty patients included to the study according to the PSG results and history consideration who were diagnosed as UARS. Fourteen (46.7%) of the patients were male, and 16 (53.3%) were female. The mean age was 46.4 ? 9.9. While determining EDS by the Epworth Sleepiness Questionnaire all patients were over 10 points and mean score was 15 ? 3.9. The mean AHI was 2.3 ? 1.4, and mean RERA was 26.1 ? 4.9 (Table 2).
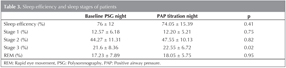
During PAP titration, the results were pathological and the mean pressure was 7.1 ? 1.1 in our study group. These patients that had over 4 cmH2O PAP pressure were diagnosed with UARS, and during diagnosis the PAP pressure that they needed during treatment was also determined. When we compared the sleep efficiency and all sleep stages in the diagnostic polysomnography and titration night; only Stage 3 increased statically significant (21.6 ? 8.36 vs. 22.55 ? 6.72, p= 0.02) (Table 3).
DISCUSSION
This study demonstrates that UARS diagnosis can be confirmed and PAP pressure needed for treatment can be determined in the same session. The gold standard method for the diagnosis of UARS is Esophageal Pressure Measurement. Decreased esophageal pressure (PES) is the earliest indication of respiratory arousals caused by increased upper airway resistance. However, this method is not being used by many labs because of the disruption of sleep quality, not being well tolerated by patients , and because it is an invasive procedure (4,5,7). Therefore, a more practical method for diagnosis is resorted to. Today, PSG is imperative to ensure the diagnosis of UARS. It is required to have AHI< 5, and RERA significantly high with no desaturation. In addition to these criteria, the presence of EDS leads to the diagnosis of UARS in the patients (1,4,8). All of the patients included in our study had AHI below 5 and RERA over 20. In all patients, EDS was confirmed by the Epworth Sleepiness Questionnaire.
UARS diagnosis is not easy due to the following reasons: Esophageal Pressure Measurement is an invasive method and is difficult to tolerate for the patients. There is no limit to RERA number to clarify the UARS diagnosis in PSG. Moreover, there are no objective methods available in practice in EDS. However, we know that increased upper airway resistance is a pathological event.
PSG results with no apnea/hypopnea or desaturation, but an increase in resistance in the upper respiratory tract directly lead us to the diagnosis of UARS. As we know, the pressure in the upper respiratory tract of a healthy person does not exceed 4 cm H2O. The most objective way to prove the upper airway resistance with non-invasive method is to perform a PAP titration.
In our country, like many parts of the world, the opinion to consider UARS as a separate disease is dominant (9). But the AASM and the ICSD-2, considers UARS as a preliminary step of OSA. In a study conducted by Guilleminault and colleagues, long-term follow-up results with a diagnosis of UARS patients who did not receive PAP therapy were published. According to this study, only 5 of 94 patients (5.3%) developed OSA. Rather than OSA, daytime sleepiness, fatigue, insomnia, difficulty concentrating, and depression has been found to be significantly increased in frequency among these patients. In addition, the same patients showed significantly increased use of hypnotic, antidepressant and stimulant drugs (10).
The complications of OSA can be explained by apnea/hypopnea and desaturation. However, UARS shows none of these symptoms, and develops similar complications with OSA just by arousals. This suggests that treatment of UARS should be taken more seriously.
In cases with sleep disorders breathing, remarkable hypertension is observed due to increased upper airway resistance. In hypertensive patients the incidence of OSAS is 30-40%, and the incidence of non-apneic snoring is 30-70% (4,5).
In one of their studies Guilleminault and colleagues showed that the borderline hypertension has been shown by to be controlled with CPAP therapy in patients with UARS. In pediatric patients, UARS have been reported to cause complications like behavioral disorders, and school failure (4,7,10,11).
In our opinion, due to the excessive daytime sleepiness, major cardiovascular problems, and the adverse effects during childhood, patients with UARS should be treated. The goal of treatment is to improve symptoms and quality of life, to reduce the morbidity and mortality of the disease by overcoming the increased upper airway resistance. Generally applicable methods for the treatment of OSAS are used for UARS (4,5,13).
Nowadays PAP therapy is the most effective treatment to overcome the resistance of the upper airway. With the use of PAP therapy, neuropsychiatric symptoms significantly improved and EDS has been shown to decrease. Even the demostration of an improvement in EDS is with PAP therapy is among the minor diagnostic criteria (1,4,13).
In one study, Guilleminault and colleagues observed that CPAP treatment or turbinectomy showed much better results than behavioral therapy alone in postmenopausal women with UARS who suffered from daytime fatigue and chronic insomnia (14).
For the patients to be treated with PAP, PAP titration is the first examination to be done. Pressure determined after PAP titration, is the threshold pressure necessary to keep the patient's upper respiratory tract open. We determined the accurate pressures necessary for our patients by PAP titration.
As already mentioned, we kept two things in mind when we performed PAP titration to our patients suspected to have UARS. First, if we observe pressure over 4 cmH2O during PAP titration, this proves the presence of patient's upper airway resistance. Second, this observation not only proves but also determines the necessary pressure for the treatment of UARS.
There are a number of limitations of our study. First, the number of patients is limited. Second, patients suspected of UARS according to PSG were included in the study. Among these patients, because of the decrasing sleep quality, UARS have not been shown with Esophageal Pressure Measurement method. For the reasons stated above, however, Esophageal Pressure Measurement, as in many places around the world, is not performed at our clinic. Third, in the evaluation of patients' EDS, the Epworth Sleepiness Questionnaire was used but has not been confirmed by MSLT. However, we set our RERA limits high for preliminary diagnostic criteria for UARS. Sleep fragmentations that occur as a result of RERA is expected to cause EDS in the patient. Fourth, the long term follow-up results were not included in the study.
As a result, among UARS suspected patients, achieving high PAP values from PAP titration is an evidence of increased upper airway resistance. In patients with normal PAP values UARS diagnosis were excluded. Use of this method defines UARS diagnosis and thought to be significant for evidence-based medicine. With The PAP method, from therapy to diagnosis protocol, the treatment pressure is also determined at the same time. Long-term follow-up of these patients under PAP treatment and the evaluation of clinical outcomes and also including higher number of patients in series will contribute to the treatment of this syndrome defined "unsolved problems in years". Larger scale studies on the subject are needed.
CONFLICT of INTEREST
None declared.
REFERENCES
- Wheatley JR. Definition and diagnosis of upper airway resistance syndrome. Sleep 2000;23(Suppl 4):193-6.
- Guilleminault C, L?ger D. Le syndrome des voies a?riennes sup?rieures: pertinence clinique et physiopathologique. Rev Mal Respir 2005;22:27-30.
- Gold AR, Dipalo F, Gold MS, O'Hearn D. The symptoms and signs of upper airway resistance syndrome. A link to the functional somatic syndromes. Chest 2003;123:87-95.
- Exar EN, Collop NA. The upper airway resistance syndrome. Chest 1999;115:1127-39.
- R?hle KH, Sclenker E, Randerath W. Upper airway resistance syndrome. Respiration 1997;64(Suppl 1):29-34.
- Rechtschaffen A KA, ed. A Manual of Standardized Terminology, Techniques, and Scoring System for Sleep Stages in Human Subjects. Los Angeles, CA: VCLA, 1968.
- Kryger MH. Monitorig respiratory and cardiac function. In: Kryger MH, Roth T, Dement WC (eds). Principles and Practice of Sleep Medicine. 3rd ed. Philadelphia: WB Saunders Company 2000:1217-30.
- Christian Guilleminault and Virginia De Los Reyes. Upper airway resistance syndrome. Handbook of Clinical Neurology. Vol. 98 (3rd series) Sleep Disorders, Part 1. 2011;401-9.
- Kristo DA, Shah AA, Lettieri CJ, MacDermott SM, Andrada T, Taylor Y, et al. Utility of split-night polisomnography in the diagnosis of upper airway resistance syndrome. Sleep Breath 2009;13:271-5.
- Guilleminault C, Kirisoglu C, Poyares D, Palombini L, Leger D, Farid-Moayer M, et al. Upper airway resistance syndrome: a long-term outcome study. Journal of Psychiatric Research 2006;40:273-9.
- Guilleminault C, Stoohs R, Shiomi T, Kushida C, Schnittger I. Upper airway resistance syndrome, noccturnal blood pressure monitoring and borderline hypertension. Chest 1996;109:901-8.
- Guilleminault C, Winkle R, Korobkin R, Simmons B. Children and nocturnal snoring: Evaluation of the effects of sleep related respiratory resistive load and daytime functioning. Eur J Pediatr 1982;139:165-71.
- Montserrat JM, Badia JR. Upper airway resistance sydrome: Sleep Medicine Reviews 1999;3:5-21.
- Guilleminault C, Palombini L, Poyares D, Chowdhuri S. Chronic insomnia, postmenaposal women, end SDB. Part 2. Comparison of non-drug treatment trials in normal breathing and UARS post-menopasual women complaining of insomnia. J Psychosomat Res 2002;53:617-23.
Yaz??ma Adresi (Address for Correspondence)
Dr. O?uz K?KT?RK
Gazi ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
ANKARA - TURKEY
e-mail: kanbaydr@yahoo.com