RESEARCH ARTICLE
Doi: 10.5578/tt.8516
Tuberk Toraks 2014;62(4):259-266

Koah'ta egzersiz kapasitesinin belirlenmesinde?
kardiyopulmoner egzersiz testiyle 6 dakika y?r?me? testinin kar??la?t?r?lmas?
Fatma ??FTC?1, Elif ?EN1, ?znur AKKOCA YILDIZ1, Sevgi SARYAL1
1 Ankara ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara, T?rkiye
1 Department of Chest Diseases, Faculty of Medicine, Ankara University, Ankara, Turkey
?ZET
Koah'ta egzersiz kapasitesinin belirlenmesinde? kardiyopulmoner egzersiz testiyle 6 dakika y?r?me? testinin kar??la?t?r?lmas?
Giri?: Bu ara?t?rmada kronik obstr?ktif akci?er hastal??? (KOAH)olan olgularda 6 dakika y?r?me testi (6DYT) ile kardiyopulmoner egzersiz testi (KPET) aras?ndaki ili?kiyi ve bu iki egzersiz testinin solunum fonksiyonlar? aras?ndaki ili?kiyi ara?t?rmak ama?lanm??t?r.
Materyal ve Metod: Orta ve a??r dereceli KOAH'? olan 36 (35 erkek, 1 kad?n) olguya ayr?nt?l? solunum fonksiyon testleri 6DYT ve KPET yap?lm??t?r.
Bulgular: Maksimal oksijen t?ketimi 6 dakika y?r?me mesafesi ile ili?kilidir. Her iki egzersiz testi de solunum fonksiyonlar? ile ili?ki g?stermektedir. Ancak, maksimum egzersiz kapasitesi solunum fonksiyonlar? ile istatistiksel olarak daha anlaml? ili?ki g?stermektedir. ?ki test de statik akci?er hacimleri ile ili?kilidir. ?nspiratuar kapasite 6DYT ve KPET parametreleriyle ili?kilidir. KPET dif?zyon kapasitesi ve maksimal inspiratuar bas?n? ile ili?kili saptan?rken, 6DYT ile ili?ki g?r?lmemi?tir. Hava yolu iletimi ve direnci testleri ile egzersiz testleri aras?nda ili?ki saptanmam??t?r.
Sonu?: Basit bir test olan 6DYT KOAH'da egzersiz kapasitesini belirlemede kullan?labilir. Her iki test de ventilatuar bozuklu?u g?steren ?zellikle FEV1, maksimum volenter ventilasyon (MVV) ve inspiratuar kapasite ile belirlenen solunum fonksiyon testleri ile ili?kilidir. Ancak, CPET hiperinflasyonu ve solunum kas g?c?n? daha iyi de?erlendiren ve 6DYT'den daha ayr?nt?l? sonu?lar veren bir egzersiz testidir.
Anahtar kelimeler: KOAH, kardiyopulmoner egzersiz testi, 6 dakika y?r?me testi, solunum fonksiyon testleri
SUMMARY
A comparison of cardiopulmonary exercise test and 6 minute walking test in determination of exercise capacity in chronic obstructive pulmonary disease
Introduction: This study aimed to determine the relationship of 6 minute walking test (6MWT) and cardiopulmonary exercise test (CPET) with each other and with the measures of lung functions in patients with chronic obstructive pulmonary disease (COPD).
Materials and Methods: Pulmonary function tests, 6MWT, and CPET were performed in 36 (35 males, 1 female) patients with moderate and severe COPD.
Results: Maximum oxygen uptake was significantly correlated with 6 minute walking distance. Both exercise tests were correlated with pulmonary function tests. However, maximum exercise capacity was more closely correlated with measures of lung function than 6MWT. Both tests were significantly correlated with static lung volumes. Inspiratory capacity (IC) was significantly correlated with 6MWT and CPET parameters. CPET was significantly correlated with diffusion capacity and maximal inspiratory pressure. Airway conductance and resistance tests showed no correlation with the exercise tests.
Conclusion: 6MWT is a simple and valuable test to determine the exercise capacity of COPD patients. Both 6MWT and CPET are correlated with ventilatory impairment determined by the lung function tests, particularly FEV1, maximum voluntary ventilation (MVV), and IC. However, CPET is an exercise test that more accurately evaluates and provides more detailed information about hyperinflation and respiratory musce strength than 6MWT does.
Key words: COPD, cardiopulmonary exercise test, 6 minute walking test, pulmonary function tests
INTRODUCTION
Several studies have shown that both certain objective and subjective measurements are related to exercise capacity in patients with chronic obstructive pulmonary disease (COPD). In general, measures of lung function have limited ability to predict exercise capacity in an individual. Exercise testing in individuals with COPD is a useful means for assessing the degree of disability, prognosis, presence of exercise-induced hypoxemia, and response to treatment (1). FEV1 is the most widely used index of lung function used to assess COPD severity. However, a limitation of FEV1 is that it does not directly reflect the degree of static and dynamic hyperinflation or the exercise capacity in COPD. Because of its relationship with dynamic hyperinflation, inspiratory capacity (IC) might be a better predictor of exercise performance in COPD than FEV1 (2).?
Because of its ability to provide measures of physiologic data in addition to diagnostic information, cardiopulmonary exercise test (CPET) using cycle ergometer with measurement of indexes of cardiac and pulmonary performance such as maximum oxygen consumption has long been the standart method for assessment of exercise capacity in COPD. However, cycle ergometry has some limitations hindering its use in routine clinical practice. First, CPET employs an activity that is less familiar than walking; and second, measurement of gas exchange requires an expensive and complex technology (3). Finally, exercise capacity, expressed in units of oxygen consumption or power output, can be difficult to interpret by cycle ergometry, particularly with regard to an individual's ability to perform daily activities.
In recent years, simple walking tests have been increasingly used for the assessment of COPD patients in clinical and research settings. The 6 minute walking test (6MWT) has a good reliability and validity as a measure of functional capacity (4). The advantages of the 6MWT include the use of minimal technical resources and employment of a familiar form of exercise.
In conclusion, we aimed to determine whether lung function measurements, arterial blood gases, complete blood count, and inflammatory markers, were correlated with both forms of exercise tests to a similar degree.
MATERIALS and METHODS
This study prospectively enrolled 36 (1 female, 35 males) clinically stable COPD patients with a mean age of 60 ? 9 years between December 2007 and June 2008. All patients were categorized based on the GOLD criteria (5).
Ankara University Medical Ethical Committee approved the study. A written informed consent was obtained from each subject. All subjects underwent detailed clinical evaluation. Duration of clinical symptoms and signs, current treatment regimen, concomitant diseases, and smoking history were questioned. Pulmonary function tests (expiratory air flow rates, static lung volumes, diffusion testing, maximum inspiratory and expiratory pressure, airways resistance, and conductance) were performed in our clinic's laboratory. Expiratory flow rates were measured by Vmax 229 Pulmonary Function/Cardiopulmonary Exercise Testing Device (Sensormedics, Bilthoven, Netherland). Body plethysmography device (Body box SensorMedics 6200 Autobox, Bilthoven, Netherland) was used for lung volume measurements.?
6MWT was measured at a 20-meter-long corridor. None of the patients needed portable oxygen supplementation, as assessed by the ATS criteria, during the 6-minute walk test (6).
A symptom-limited or maximal incremental exercise test with Bruce protocol was performed on a cycle ergometer (Ergometrics 900, SensorMedics?, Bilthoven, Netherlands) with workload increases of 15 Watts at 1-minute intervals. Electrocardiography, blood pressure and oxygen saturation (Palce pulse oximeter? 53400, California, USA) were closely monitored during the test.
O2 consumption (VO2), CO2 production (VCO2), respiratory exchange coefficient (R), heart rate reserve (HRR), O2 pulse (VO2/HR), breath reserve (BR), minute ventilation (VE), ventilation equivalents (VE/VO2, VE/VCO2) were determined by CPET.? Oxygen saturation, heart rate, and blood pressure were monitored while the dyspnea level was assessed by the Borg dyspnea scale before and after both exercise tests.
Statistical analysis was performed using Statistical Package for Social Sciences, version 11.5 for Windows (SPSS INC., Chicago, IL, USA). Shapiro-Wilk test was used to test the normality of distribution of the variables. Descriptive data were presented as means and standard deviation for continuous variables and number and percentages for categorical variables. Pearson and Spearman correlation tests were used to determine the linear correlation between two variables. A p value less than 0.05 was considered statistically significant.
RESULTS????????
The general characteristics of the study population were listed on Table 1. A total of 36 patients were enrolled. According to the GOLD criteria, 14 (38%) subjects had severe and 22 (62%) had moderately severe disease. Six (4 with severe and 2 with moderately severe COPD), patients completed 6MWT but failed to finish the CPET as a result of being unaccustomed to cycling and were thus excluded from the study. Because of ease of adaptation to 6MWT, compliance to it was higher than that of CPET.
The mean CPET exercise time was 9.48 ? 2.06 minutes while the mean 6 minute walking distance was 513.70 ? 68.68 meters. Data related to the exercise capacity of COPD patients were given on Table 2.? Thirty patients could complete the CPET while 6 patients could not. Among those who could not complete CPET, 4 had severe and 2 had moderately severe COPD. CPET was terminated because of dyspnea in 13 (43.3%) patients, leg fatigue in 15 (50%) patients, and a high blood pressure response during the test in 2 (6.7%) patients.
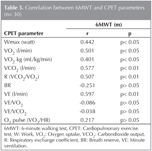
6MWT was significantly correlated with maximal exercise test parameters, maximum work (Wmax), maximum heart rate (HRmax), oxygen uptake (VO2), corbondioxide output (VCO2) respiratory exchange ratio (R), and minute ventilation (VE) (Table 3).
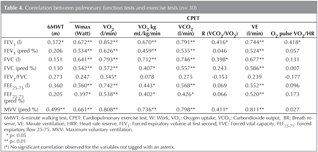
Comparison of the six minute walking distance and the pulmonary function test parameters showed that FEV1 and MVV were significantly correlated with 6MWT. VO2 (L/dk) and VO2 (pred %)? were significantly correlated with all pulmonary function test parameters. Wmax, VE, VCO2 and VO2 kg were significantly correlated with FEV1 (L), FEV1 (%), FVC (L), FVC (%), FEF 25-75 (L), FEF 25-75 (%), and MVV. VE/VO2, VE/VCO2, and BR were not correlated with any pulmonary function test parameter. As a result, both exercise tests were correlated with FEV1 and MVV. However, maximum exercise capacity was more closely correlated with lung function measures than six-minute walking distance (Table 4).
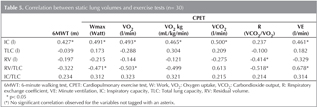
The relationship between both exercise tests and static lung volumes was also assessed. 6MWT was correlated with IC. There were significant correlations between VE (l/min) and IC, RV/TLC; Wmax, VO2 kg (mL/kg/min) and VCO2, IC, RV/TLC. R value was negatively correlated with RV and RV/TLC (Table 5). The analysis of the correlation between exercise tests and lung volumes revealed significant correlation between IC and both tests. CPET parameters were correlated with RV/TLC, an indicator of air trapping.
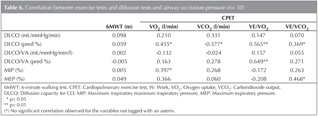
No significant correlation was observed between 6MWT and the diffusion test. DLCO (ml/mmHg/min) was positively correlated with HRR. VO2, VCO2, VE/VO2, VE/VCO2 were significantly correlated with DLCO (pred %) and MIP (%). There was a significant correlation between DLCO/VA and VE/VO2 (Table 6).
Neither of the two tests was significantly correlated with airway conductance and resistance tests.
DISCUSSION
This study aimed to assess the relationship of two exercise tests with each other and with lung functions in patients with COPD. It revealed that in clinical practice both exercise tests may be used in patients with COPD, although CPET was more effective in the assessment of exercise capacity and more significantly correlated with lung functions.
COPD patients have limited exercise capacity and quality of life. Evaluation of functional capacity in COPD has recently gained importance with respect to understanding and controlling the actual or estimated effects of the disease. Six minute walking test is preferred because of its ease of adaptation and reproducibility. Some authors have suggested that 6MWT is the most effective exercise test for evaluation of functional capacity during daily activities (7-9).
In this study, the majority of the subjects had moderately severe or severe COPD. 6MWT is more effective in moderately severe or severe COPD because in mild disease walking effort does not cause stress and reaches a plato level at 600 meters. There is a significant correlation between walking distance and functional parameters in patients with a FEV1 level less than one liter. Dyspnea scales, hyperinflation, and patient motivation are the primary determinants in these patients (10).
The data of six subjects were excluded from the statistical analysis due to failure to complete cycle ergospirometry because of unfamiliarity with cycling. CPET requires a more advanced technology, high patient compliance, and continuous monitorization during the test. However, Turkish population is more familiar to walking as a daily activity than cycling, and it is also easy to adopt for them. This may explain the high patient compliance with corridor walking test. Some previous studies have also reported a higher patient compliance to 6MWT.
Besides the impaired lung mechanics, arterial desaturation due to ventilation response increases the dyspnea sensation. Increased respiratory demand in exercise results in air trapping and dynamic hyperinflation in patients with flow limitation. Dyspnea sensation varies among patients despite similar workloads. It has been showed that leg fatigue limits peak exercise performance as much as dyspnea (11,12).
The average muscle loss is about 30% in moderate to severe COPD patients. COPD? patients highly perceive leg fatigue and terminate exercise prematurely due to reduction of muscle power by 40-45%? (13,14). In our study, exercise was terminated due to dyspnea in 43% of the subjects and due to leg fatigue in another 50%. Leg fatigue appaears to cause termination of exercise in mild to moderate COPD while dyspnea is the cause for termination of exercise in severe COPD. Although literature data suggest that dyspnea is the most common symptom causing termination of CPET, it was leg fatigue that most commonly led to termination of CPET in our study, possibly due to certain characteristics of our population including lack of conditioning, sedentary life style, and COPD-induced muscle weakness (13).? Similarly, Killian et al. showed that leg fatigue is the primary reason for termination of the exercise (11).
In this study patients walked 513.70 ? 68.68 meters in 6 minutes. It is well known that disease severity is related to walking distance. Our study population was composed of moderately severe (62%) and severe (38%) COPD subjects. Completing a shorter walking distance may be explained by the severity of the disease. At present, there are no widely accepted normal reference values for the 6MWT. However, two former studies provided reference formulae for men and women (14-16).
Normal or mildly impaired subjects may exhibit a ceiling effect because jogging is not permitted in the testing procedure. Walking rate cannot exceed a certain level and walking distance tends to accumulate around a certain value (17). Mildly impaired individuals with COPD, therefore, may retain normal or near normal 6MWT distance. As the disease progresses, the maximum exercise capacity attained in CPET declines to a greater degree than that in 6MWT. This is believed to be due to the fact that, in most individuals, the 6MWT reflects the maximum sustainable exercise (18). Some patients, however, may adopt a strategy whereby they transiently reach maximum oxygen capacity during 6MWT (19).
CPET reflects the cardiopulmonary oxygen transport system. It is believed that CPET parameters such as maximum oxygen uptake (VO2max) reflect COPD severity. However, pulmonary function tests at rest do not reflect exercise performance and exercise-induced hypoxemia (3). In our study, not surprisingly, VO2max levels pointed to a low exercise performance in moderate to severe COPD patients. COPD severity appeared to affect 6MWT less than it affected exercise capacity in CPET. In this study the association between the two exercise test parameters was also assessed. The two forms of exercise testing were correlated with each other. 6MWT was particularly correlated with VO2 max and Wmax. These results reflect the parallel nature of the two exercise tests. While CPET provides specific and detailed measurements of maximum exercise performance, 6MWT provides information about functional ability in the simplest way (20,21). Previous studies comparing the exercise tests head-to-head have reported varying results. We found that, similar to most of the previous studies, metabolic parameters (VO2, VCO2, R), respiratory parameters (BR, VE), and maximum work parameters of CPET were significantly correlated with 6MWT (22).
Disease progression results in death space ventilation by causing parenchymal destruction and loss of elastic components. FEV1 is the most susceptible parameter to airflow limitation. It is used for staging purposes and determination of the prognosis. Both tests used in the present study were correlated with FEV1. These result shows that the severity of obstruction was related to exercise capacity. Although 6MWT and CPET were significantly correlated with each other, they measure somewhat different domains of exercise performance in individuals with COPD. Performance in both exercise tests is correlated with ventilatory impairment indicated by standard lung function tests, particularly FEV1 and IC. On the other hand, maximum exercise capacity testing provides a more accurate assessment of physiologic as well as maximal functional impairment. The correlation of 6MWT with FEV1 was weaker than its correlations with FEV1 and VO2 (r= 0.372 vs. r= 0.672).
We found that inspiratory capacity (IC) was correlated significantly with 6MWT (r= 0.427) and CPET parameters.? IC is an important sign of hyperinflation and is inversely proportional to end expiratory lung volume (EELV). Decreased IC and IC/TLC are related to COPD survival and poor exercise tolerance (21,23). Because of its close correlation with dynamic hyperinflation, IC is a better indicator of the maximal exercise performance. Unlike FEV1, IC shows significant correlation with the clinical parameters (24).? Marin et al. studied 72 COPD patients and concluded that end expiratory lung volume (EELV) is a sensitive marker for dyspnea, indicating the correlation between maximum exercise capacity and maximum ventilation (24-27).
MVV is defined as the volume wasted in one minute by high amplitude and frequency respiration. MVV reflects the muscle performance in COPD. Due to increased airway resistance and hyperinflation, patients with moderate to severe airflow obstruction have decreased respiratory muscle power. This study demonstrated a significant correlation between MVV and the two exercise tests.
In patients with pulmonary diseases DLCO is a surrogate marker of abnormal gas transfer in lungs. In COPD, death space ventilation ensues secondary to destruction of parenchyma and loss of elastic tissue. Furthermore, as in the case of our subjects, lung volumes continually increase, subsequently leading to hyperinflation. Alveolar destruction and loss of the vascular bed causes an increase in pulmonary vascular resistance. Gas diffusion becomes impaired and perfusion becomes nonhomogenous. Eventually, diffusion capacity decreases, as in our subjects. In our study DLCO was related to CPET parameters but not to 6MWT. These results suggest that CPET more accurately assess alveolar destruction, capillary destruction, air trapping, and hyperinflation. It has also been suggested that CPET is able to provide more detailed information about the exercise capacity in COPD with a predominantly emphysematous component. Marthan et al. studied 51 severe COPD patients by inert gas method in resting state and concluded that the ventilation-perfusion mismatch is the most important reason of the gas exchange defect (28).
Wasserman et al. studied 276 subjects and measured resting and exercise-related DLCO values. Resting DLCO values were correlated with exercise measures. They concluded that resting DLCO was a specific but insensitive test for exercise (29).
Mak et al. and Jones et al. studied 42 COPD and 28 severe asthma patients, respectively. They concluded that DLCO was positively correlated with walking distance (30,31). Wijkstra et al. studied 40 severe (FEV1< 50%) COPD patients and found a significant relationship between pulmonary function tests (FEV1, RV, DLCO) and exercise tests (21).
In COPD patients, the decrease in flow rates, increase in airway resistance, high-volume respiration, and hyperinflation cause respiratory muscle weakness. Afferent nerves from the thoracic wall muscles, tendon muscles and joints are responsible from the dyspnea sensation. COPD patients, as our study subjects, show a decreased MIP, a parameter that reflects the functions of diaphragm, intercostals, and accessory respiratory muscles. Hyperinflation also causes the MIP level to decrease (32).? In our study VO2max was positively correlated with MIP. VO2max, a marker of exercise capacity, decreased proportional to the decreasing MIP values.
In COPD, narrowing of the airway lumen and decline in elastic recoil capacity results in an increase in resistance and a decrease in conductance. In our study exercise tests were not correlated with Raw and Gaw values. Eight subjects were not cooperated with the test procedures used in this study and were thus excluded. A decreased number of subjects may have reduced the power of this study. Further studies are needed to evaluate the effects of respiratory conduction and resistance on exercise capacity.
As a conclusion; 6MWT is a simple and valuable test for determination of exercise capacity of COPD patients. Patient compliance to 6MWT is higher than CPET. Both tests are correlated with ventilatory impairment. However, CPET is more effective for evaluating hyperinflation, air trapping, muscle strength, and exercise capacity.
CONFLICT of INTEREST
None declared.
REFERENCES
- Brown CD, Wise RA. Field tests of exercise in COPD: The six-minute walk test and shuttle walk test. COPD 2007;4:217-23.
- Diaz O, Villafranca C, Ghezzo H, Borzone G, Leiva A, Milic-Emil, J, et al. Role of inspiratory capacity on exercise tolerance in COPD patients with and without tidal expiratory flow limitation at rest. Eur Respir J 2000;16:269-75.
- Ortega F, Montemayor T, Sanchez A. Role of cardiopulmonary exercise testing and criteria used to determine disability in patients with severe COPD. Am J Respir Crit Care Med 1994;150:747-51.
- Butland RJA, Pang J, Gross ER, Woodcock AA, Geddes DM. Two, six and, twelve minute walk tests in respiratory disease. BMJ 1982;84:1607-8.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of Chronic Obstructive Lung Disease (revised? 2011), www.goldcopd.com
- American Thoracic Society. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002;166:111-7.
- Sciurba F, Criner GJ, Lee SM, Mohsenifar Z, Shade D, Slivka W et al. Six minute walk distance in chronic obstructive pulmonary disease. Am J respir Crit Care Med 2003;167:1522-7.
- Guyatt GH, Thompson PJ, Berman LB, Sullivan MJ, Townsend M, Jones NL, et al. How should we measure function in patients with chronic heart and lung disease? J Chronic Dis 1985;38:517-24.
- Solway S, Brooks D, Lacasse Y, Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest 2001;119:256-70.
- Calverley PMA, Pearson MG. Clinical and laboratory assessment in chronic obstructive pulmonary disease. In: Calverley PMA, Mac Nee W, Pride NB, Rennard SI (eds). London: Arnold, 2003:282-309.
- Killian KJ, Summers E, Jones NL. Dyspnea and leg effort during incremental cycle ergometry. American Rev Respir Dis 1992;145:1339-45.
- Hamilton AL, Killian KJ, Summers E, Jones NL. Symptom intensity and subjective limitation to exercise in patients with cardiorespiratory disorders. Chest 1996;110:1255-63.
- Ambrosino N, Scano G. Measurement and treatment of dyspnoea. Respir Med 2001;95:539-47.
- Enright PL, Sherill DL. Referans equations fort he six minute walk in healty adults. Am J Respir Crit Care Med 1998;158:1384-7.
- Troosters T, Gosselink R, Decramer M. Six minute walking distance in healty elderly subjects. Eur Respir J 1999;14:270.
- Gibbons WJ, Fruchter N, Sloan S, levy RD. Reference values for a multiple repetition 6-minute walk test in healty adults older than 20 years. J cardiopulm Rehabil 2001;21:87-93.
- Fletcher GF. Exercise Standards for Testing and Training. A Statement for Healthcare Professionals From the American Heart Association. Circulation 2001;104:1694-740.
- Casa A, Vilaro J, Robinovich R. Encouraged 6-min walking test indicates maximum sustainable exercise in COPD patients. Chest 2005;128:55-61.
- Turner SE, Eastwood PR, Cecins NM, Hillman DR, Jenkins SC. Pysiologic responses to incremental and self paced exercise in COPD: a comparison of tree tests. Chest 2004;126:766-73.
- Ong KC, Earnest A, Lu SJ. A multidimensional grading system (BODE index) as predictor of hospitalization for COPD. Chest 2005;128:3810-16.
- TenVergert EM, Wijkstra PJ,? van der Mark TW, Postma DS, Van Altena R, Kraan J, et al. Relation of lung function, maximal inspiratory pressure, dyspnoea, and quality of life with exercise capacity in patients with chronic obstructive pulmonary disease. Thorax 1994;49:468-72.
- Berry MJ, Adair NE, Rejeski WJ. Use of peak oxygen consumption in predicting physical function and quality of life in COPD patients. Chest 2006;129:1516-22.
- Ulubay G, Gorek A, Savas S, Oner Eyuboglu F. Evaluation of dynamic hyperinflation?? parameters and exercise capacity at maximal exercise in patients with COPD. Tuberk toraks 2005;53:340-6.
- Carter R, Peavler M, Zinkgraf S, Williams J, Fields S. Predicting maximal exercise ventilation in patients with chronic obstructive pulmonary disease. Chest 1987;92:253-9.
- Marin JM, Carrizo SJ, Gascon M. Inspiratory capacity, dynamic hyperinflation, breathlessness and exercise performance during the six minute walking test in COPD. Am J Respir Crit Care Med 2001;163:1395-9.
- Fink G, Lebzelter J, Turner D, Klainman E, Shlomo M, Katz I, et al. Pulmonary function threshold for distinguishing ventilatory- and nonventilatory-limited patients with airflow obstruction. Respir Med 1998;92:1245-50.
- LoRusso TJ, Belman MJ, Elashoff JD, Koerner SK. Prediction of maximal exercise capacity in obstructive and restrictive pulmonary disease. Chest 1993;104:1748-54.
- Marthan R, Castaing Y, Manier G, Guenard H. Gas Exchange alterations in patients with chronic obstructive lung disease. Chest 1985;87:470-5.
- Wasserman K, Sue DY, Oren A, Hansen JE. Diffusing capacity for carbon monoxide as a predictor of gas exchange during exercise. N Engl J Med 1987;316:1301-6.
- Mak VHF, Bugler JR, Roberts CM, Spiro SG. Effect of arterial oxygen desaturation on six minute walk distance, perceived effort, and perceived breathlessness in patients with airflow limitation. Thorax 1993;48:33-8.
- Jones NL, Jones G, Edwards RHT. Exercise tolerance in chronic airway obstruction. Ani Rev Respir Dis 1971;103:447-91.
- Akkoca O, Demir G, Saryal S, Karab?y?koglu G. The effect of hyperinflation on respiratory muscles and breathing pattern in COPD. Tuberk Toraks 2003;51:244-52.
Yaz??ma Adresi (Address for Correspondence)
Dr. Fatma ??FTC?
Ankara ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
ANKARA - TURKEY
e-mail: fatmarslann@yahoo.com