LETTER TO THE EDITOR
Doi: 10.5578/tt.6814
Tuberk Toraks 2014;62(3):253-254

?ocukluk ?a??nda spontan pn?momediastinum: ast?m tan?s? alan ad?lesan olgu
Fatih FIRINCI1, Funda ?ZG?RLER1, Mustafa DO?AN1, Ali KO?Y???T2, Emin METE1
1 Pamukkale ?niversitesi T?p Fak?ltesi, Pediatri Anabilim Dal?, Denizli, T?rkiye
1 Department of Pediatrics, Faculty of Medicine, Pamukkale University, Denizli, Turkey
2 Pamukkale ?niversitesi T?p Fak?ltesi, Radyoloji, Denizli, T?rkiye
2 Department of Radiology, Faculty of Medicine, Pamukkale University, Denizli Turkey
Spontaneous pneumomediastinum (SPM) is a term used to define presence of gas in the mediastinum without any associated condition like mechanical ventilation, cardiac catheterization or thoracic surgery, which is first reported by Hamman (1). This condition usually affects tall young males (2). Here we report an adolescent case diagnosed with SPM with their radiological and clinical findings.
CASE REPORT
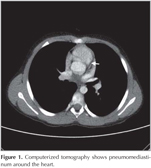
A 12 year old an adolescent boy was administered to our clinic with persisting cough for one month. His pulmonary function test was normal and atypical pneumonia treatment was given. After one month it was learned that his cough resolved after treatment but increased in a few days. Although his physical examination was normal, his chest radiogram showed that there was linear opacity along cardiac border. There was not any history of trauma, invasive procedure or smoking. Computerized tomography also confirmed pneumomediastinum (Figure 1). Inhaled steroid and analgesic was given. Since his acute phase reactants were negative and there was not any sign of infection, antibiotherapy did not given. In a few days his control chest radiogram showed resolution of gas in mediastinum without any complication. In control, his pulmonary function test was consistent with asthma. He is in follow with asthma in our clinic.
DISCUSSION
Pneumomediastinum is defined as gas into the mediastinum, however SPM is a term, which means pneumomediastinum without trauma, mechanical ventilation or surgical procedures (2). While Yellin et al. reported the incidence of SPM in adults as 1/14.000, Lee et al. reported as 1/8302 in children (3,4). Age distrubiton shows bimodal peak of children age less than 4 years and adolescents (4). Although SPM may appear spontaneously in some children like our case, in 70-90% of patients, there were triggers like asthma, vomiting, Valsava maneuver or an infection (2). In our case asthma triggered pneumomediastinum. Chiu et al. reported that asthma is the most common cause of SPM in children. Also it is recommended that, when a child is treated with SPM, after treatment child should perform diagnostic pulmonary function test (5). Our patients also got diagnosis of asthma after SPM.
The most common presenting symptom is dyspnea and secondly chest pain, followed with neck pain (5). Chest pain is characteristically sudden and pleuritic. Also may radiate to the back and shoulders. Yellin et al. recommends routine chest X-ray for all young patients that present to emergency departments with chest pain and dyspnea (3).
Anteroposterior chest X-ray is usually enough for diagnosis. If chest X-ray is not diagnostic or to rule our perforation computerized tomography may be considered.
SPM is usually benign condition that resolves in few days spontaneously. Mostly analgesic and bed rest is enough for recover (6). Our patient general condition and physical examination was normal. Also there were no signs of infection, so we did not hospitalize him but called for control in a few days. In our case SPM resolved spontaneously without complication.
As a conclusion, although it is a rare condition, SPM should be considered when especially an adolescent male admitted with acute chest pain. Also in patients followed with asthma, SPM should be kept in mind.
CONFLICT of INTEREST
None declared.
REFERENCES
- Hamman L. Spontaneous mediastinal emphysema. Bull John Hopkins Hosp 1939;64:1-21.
- Chalumeau M, Clainche L, Sayeg N, Sannier N, Michel JL, Marianowski R, et al. Spontaneous pneumomediastinum in children. Pediatric Pulmonology 2001;31:67-75.
- Yellin A, Gapanavicius GM, Lieberman Y. Spontaneous pneumomediastinum: Is it a rare cause of chest pain? Thorax 1983;38:383-5.
- Lee CY, Wu CC, Lin CC. Etiologies of spontaneous pneumomediastinum in children of different ages. Pediatrics & Neonatology 2009;50(5):190-5.
- Chiu CY, Wong KS, Yao TC, Huang JL. Asthmatic versus non-asthmatic spontaneous pneumomediastinum in children. Asian Pacific Journal of Allergy and Immunology 2005;23:19-22.
- Tezel ?, Varer P, Baysungur V, Okur E, Halezero?lu. Spontaneous pneumomediastinum: report of two cases. Ulusal Travma Acil Cerrahi Derg 2011:13(4):368-70.
Yaz??ma Adresi (Address for Correspondence)
Dr. Fatih FIRINCI
Pamukkale ?niversitesi T?p Fak?ltesi,
Pediatri Anabilim Dal?,
20500, DEN?ZL? - TURKEY
e-mail: fatihfirinci@yahoo.com