RESEARCH ARTICLE
Doi: 10.5578/tt.8320
Tuberk Toraks 2014;62(3):177-182

Akut hiperkapnik solunum yetmezli?inde noninvaziv mekanik ventilasyonun ge? ba?ar?s?zl??? i?in risk fakt?rleri
Ayd?n ??LEDA?1, Ak?n KAYA1, ?zlem ER?EN D?KEN1, Zeynep P?nar ?NEN1, Elif ?EN1, Nalan DEM?R1
1 Ankara ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara, T?rkiye
1 Department of Chest Diseases, Faculty of Medicine, Ankara University, Ankara, Turkey
?ZET
Akut hiperkapnik solunum yetmezli?inde noninvaziv mekanik ventilasyonun ge? ba?ar?s?zl??? i?in risk fakt?rleri
Giri?: Noninvaziv mekanik ventilasyon akut hiperkapnik solunum yetmezlikli hastalar?n ?o?unda erken d?zelme sa?lar. Bu ?al??mada amac?m?z, akut hiperkapnik solunum yetmezlikli hastalarda noninvaziv mekanik ventilasyonun ge? ba?ar?s?zl??? i?in risk fakt?rlerini saptamakt?r.
Materyal ve Metod: Doksan ?? hasta prospektif olarak de?erlendirildi. Noninvaziv mekanik ventilasyon, hastan?n ent?basyon ihtiyac? geli?meden hastaneden taburcu olmas? halinde ba?ar?l? (grup 1), kan gazlar?nda ve genel durumunda ba?lang??ta d?zelme sonras? k?t?le?me g?r?lmesi halinde ise ge? ba?ar?s?z olarak kabul edildi (grup 2).
Bulgular: Noninvaziv mekanik ventilasyon 62 (%66.7) hastada ba?ar?l?yd?. 25 (%26.9) hastada ge? ba?ar?s?zl?k g?zlendi. Tedavi ?ncesi pH, PaCO2 ve PaO2/FiO2 a??s?ndan grup 1 ve grup 2 aras?nda farkl?l?k yoktu. Ancak, serum C-reaktif protein d?zeyi, Akut Fizyolojik ve Kronik Sa?l?k De?erlendirme II (APACHE II) skoru, bron?iektazi s?kl??? ve pn?moni anlaml? olarak daha y?ksekti ve serum albumin d?zeyi, Glasgow koma skalas?, ?ks?r?k g?c? ve noninvaziv mekanik ventilasyon kompliyans? grup 2'de anlaml? olarak daha d???kt?.
Sonu?: Tedavi ?ncesi y?ksek APACHE II skoru ve C-reaktif protein d?zeyi, d???k Glasgow Koma Skalas?, albumin d?zeyi, ?ks?r?k g?c?, noninvaziv mekanik ventilasyona k?t? kompliyans, bron?iektazi ve pn?moni varl???, tedavi sonras? PaO2/FiO2'de anlaml? d?zelme olmamas? noninvaziv mekanik ventilasyon ge? ba?ar?s?zl??? i?in risk fakt?r? olarak saptand?.
Anahtar kelimeler: Akut hiperkapnik solunum yetmezli?i, mekanik ventilasyon, noninvaziv mekanik ventilasyon, solunum yetmezli?i, solunum yo?un bak?m ?nitesi
SUMMARY
The risk factors for late failure of non-invasive mechanical ventilation in acute hypercapnic respiratory failure
Introduction: Non-invasive mechanical ventilation provides early improvement in most of the patients with acute hypercapnic respiratory failure. The aim of our study was to determine the risk factors for late failure of non-invasive mechanical ventilation in patients with acute hypercapnic respiratory failure.
Materials and Methods: Ninety three patients were prospectively evaluated. Non-invasive mechanical ventilation was accepted to be successful if the patient was discharged from the hospital without the need for intubation (group 1) and to be late failure if a deterioration occurred after an initial improvement of blood gases tension and general conditions (group 2).
Results: Non-invasive mechanical ventilation was successful in 62 (66.7%) patients. In 25 (26.9%) patients a late failure was observed. There was no difference between groups 1 and 2 in terms of pretreatment pH, PaCO2 and PaO2/FiO2. However, serum C-reactive protein level, Acute Physiology and Chronic Health Evaluation II (APACHE II) score and frequency of bronchiectasis and pneumonia were significantly higher and serum albumin level, Glasgow Coma Score, cough strength and compliance to non-invasive mechanical ventilation were significantly lower in group 2.
Conclusion: The pretreatment high APACHE II Score and C-reactive protein level, low Glasgow Coma Score, albumin level, cough strength, bad compliance to non-invasive mechanical ventilation, the presence of bronchiectasis and pneumonia and absence of significance improvement in PaO2/FiO2 after treatment were determined as risk factors for non-invasive mechanical ventilation late failure.
Key words: Acute hypercapnic respiratory failure, mechanical ventilation, non-invasive mechanical ventilation, respiratory failure, respiratory intensive care unit
INTRODUCTION
In recent years non-invasive mechanical ventilation (NIMV) has been successfully used in selected populations as an effective treatment for acute hypercapnic respiratory failure (AHRF). Non-invasive mechanical ventilation improves alveolar ventilation, gas exchange abnormalities and respiratory rate in most patients with AHRF. With its low complication rate, it also shortens mechanical ventilation time and intensive care unit (ICU) stays (1,2). Despite recent encouraging results, NIMV is not always successful in the management of AHRF. The NIMV failure eventually requires intubation. The most significant success indicators of NIMV are decrease in the respiratory rate and PaCO2, improvement in pH and oxygenation in the first two hours of NIMV (3). The NIMV failure rate is in the range of 5-40% in the literature (4-11).
In a subgroup of patients, despite an initial improvement in arterial blood gases and clinical condition, a late failure (> 48 hours) characterized with deterioration after an initial success may occur. The recognition of this subset of patients is critical because prolonged treatment of NIMV may result in a delay in the time of intubation and increased mortality. Although, the factors associated with NIMV failure have been well established, the risk factors for late failure of NIMV and the clinical and physiological characteristics of these patients has been evaluated in only a few studies (12,13).
In this study, we aimed to establish the effectiveness of NIMV and risk factors related with late failure of NIMV in patients with AHRF.
MATERIALS and METHODS
The study was performed in a respiratory ICU of tertiary-care university teaching hospital. The study protocol was approved by the local ethics committee. Informed consent was obtained from the patients or the first-degree relative. Patients who were admitted with AHRF were enrolled to study and evaluated prospectively. Acute hypercapnic respiratory failure was defined as; as severe dyspnea, hypercapnia (PaC02> 45 mmHg) and acute respiratory acidosis (pH< 7.35). Patients who had contraindications for NIMV [respiratory or cardiac arrest, medical instability (hypotensive shock, myocardial infarction, uncontrolled ischemia or arrhythmia), inability to protect airways, untreated pneumothorax, mask unsuitability, (facial surgery, trauma, deformity or burn), recent upper airway or oesophageal surgery] were excluded from the study.
The demographical data and diagnoses of the patients were recorded. Also, strength of cough (0: too weak, 10: strongest), secretion quantities (0: none, 10: plenty) and patient's compliance score to NIMV (1= poor, 2= quite bad, 3= sufficient, 4= good, 5= excellent) were evaluated by the Likert scale. Respiratory rate, heart rates, blood pressure values, complete blood count, blood biochemistry, C-reactive protein (CRP), Glasgow Coma Score (GCS) and Acute Physiology and Chronic Health Evaluation II (APACHE II) score were recorded. The presence of bronchiectasis and pneumonia were investigated by radiologic evaluation.
All patients received standard medical treatment with oxygen by nasal cannula to maintain arterial saturation at approximately 90%, mucolytics and antibiotics if needed. Chronic obstructive pulmonary diseases (COPD) patients also received inhaled steroids, bronchodilators and oral steroids (for one week) and teophylline. Patients were ventilated with NIMV using a full face mask. The inspiratory positive airway pressure (IPAP) was adjusted according to patient's tolerance to obtain a tidal volume of 7-10 mL/kg with an expiratory positive airway pressure (EPAP) lower than 7 cmH2O. The EPAP was set initially at 5 cmH2O and increased in increments of 1 cmH2O until fractional inspired oxygen (FiO2) requirement was less than 0.5. The respiratory count, heart rate, systolic and diastolic blood pressures, arterial blood gasses were evaluated in the 1st and 3rd hours of the treatment.
For associated complications, factors reported by Jimenez et al. were used (14). The complications of NIMV were also recorded.
While the success of NIMV was defined as absence of death or need of intubation with the patient's discharge from hospital (group 1), late failure (after > 48 hours of NIMV) was defined as deterioration occurred after an initial improvement of blood gas tension and general condition (group 2). At the time of late failure, patients in group 2 were still receiving NIMV. Early failure of NIMV was defined as death or need of intubation after a few hours of NIMV and this group was not included in the comparison. The need of intubation was defined as presence of one of following criteria: (1) pH below 7.20, (2) pH: 7.20-7.25 on two occasions 1 h apart, (3) hypercapnic coma (GCS< 8 and PaCO2> 8kPa) (4), PaO2 below 6 kPa despite maximum tolerated FiO2 and (5) cardiorespiratory arrest.
Statistical Analysis
The SPSS 11.5 package program was used in the analysis of the data. As a defining measure, the average standard deviation [median (min-max)] was used in the variables acquired using measures, and the frequency (%) was used in the variables acquired using a count. For comparisons between the groups, the Kruskal-Walls variance analysis was used, while within the groups, the Friedman test was used. A p value of less than 0.05 was considered as statistically significant.
RESULTS
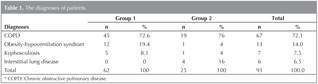
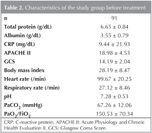
Ninety three patients with AHRF, with a mean age of 67.70 (median 69 ? 11.97 years), admitted to ICU were enrolled to study. The diagnoses in both groups were showed in Table 1. 73 (78.5%) of 93 patients had comorbid diseases. There were no significant differences in term of comorbid diseases between two groups. The baseline characteristics of study group were shown in Table 2.
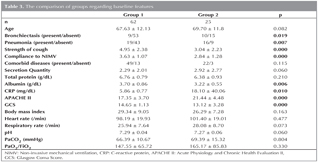
While NIMV was successful in 62 (66.7%) patients, in 6 patients early failure and in 25 (26.9%) patients late failure was observed. The mean time of late failure was 6.3 days (median 4.50 ? 4.66). The comparison of groups regarding baseline features were showed in Table 3. There was no difference between groups 1 and 2 in terms of pretreatment pH, PaCO2, PaO2/FiO2, respiratory rate, heart rate, and systolic and diastolic blood pressures. However, serum CRP level, APACHE II score were significantly higher and serum albumin level and GCS were significantly lower in group 2. The presence of bronchiectasis and pneumonia was significantly higher in group 2. The cough strength and compliance to NIMV score were significantly higher in group 1. The amount of secretion was higher in group 2, but the difference was not significant. The compliance score and cough strength which were evaluated by Likert scale were significantly lower in group 2.
There was no significant difference for baseline pH and PaCO2 between two groups. Also, after 1 h and 3 h of NIMV a significant improvement was observed in both groups. Similarly, the respiratory rate was significantly decreased in both groups after 1 h and 3 h of NIMV. While a significant decrease in heart rate after 1 h and 3 h of NIMV was observed in group 1, there was no significant change in group 2 (p: 0.003 and 0.881, respectively). Also, after 1 h and 3 h of NIMV, a significant increase in the PaO2/FiO2 value was observed in group 1 (p: 0.01), however there was no significant change in group 2 (p: 0.79).
For associated complication, before treatment, there was no significant difference between group 1 and group 2 (19.4% vs. 32%, respectively; p: 0.11). However, after NIMV there was significantly higher associated complications in group 2 (13.3% vs. 44%, respectively; p: 0.004).
DISCUSSION
In recent years, NIMV has been shown to be effective in certain types of acute respiratory failure, based on the results of clinical trials showing improved outcomes. However, NIMV is not always successful and selection of appropriate patients is crucial for the optimization of NIMV success rates. Predictors of NIMV success or failure may be helpful in selecting patients and the reported best predictors of success of NIMV are reduction in respiratory rate, improvement in pH, oxygenation and PaCO2 within one to two hours. The pretreatment high APACHE II score, CRP level and low GCS were also reported as predictive factors for NIMV failure (15). In some patients, despite an initial improvement, after > 48 hours of NIMV a deterioration which is defined as late failure may be developed. There is little data in the literature about the clinical and physiological characteristics of these patients and the risk factors for late failure of NIMV.
In a multicentre randomised study comparing NIMV with standart treatment protocols in patients with COPD, it was shown that the use of NIMV significantly reduced the need for endotracheal intubation; however, 15% of patients who were successfully treated with NIMV initially, needed endotracheal intubation after at least 48 hours (16). In another study performed by Meduri et al, NIMV was applied in 158 patients with ARF (1). NIMV was effective in improving or correcting gas exchange abnormalities in 80% of patients and avoiding endotracheal intubation in 65%. However, 28% of the initial responders needed endotracheal intubation and the mortality rate in this subgroup was 22%. The characteristics of this subset of patients were not determined in both of these two studies. There are only a few studies evaluating factors related with late failure of NIMV. Moretti et al, studied 186 patients with COPD treated with NIMV because of AHRF (12). In their study, 74% of patients were successfully ventilated non-invasively at first and were therefore enrolled for data analysis. The authors found that, after 8.4 days (range 3-13) days of NIMV 23% of patients experienced a new episode of acute respiratory failure. The occurrence of late NIMV failure was significantly associated with functional limitations before admission to the respiratory ICU, the presence of medical complications and a lower pH on admission. They also reported that, these patients have a very poor in hospital prognosis, especially if NIMV is continued rather than prompt initiation of invasive ventilation. In another study, performed by Carratu et al, in which 122 patients with COPD complicated by ARF and treated with NIMV were enrolled, 10 (8%) patients? had a late failure (13). This subgroup of patients had poor prognosis with a 80% mortality. The authors reported that the characteristics of the late failure patients group were very similar to the success group without any statistically significant difference and the only predictor of late failure was the presence of metabolic disorders. They also reported that, the early failure group had different characteristics owing to more severe conditions with higher values of APACHE II score and lower values of pH and GCS.
In our study, the rate of late failure was 26.9%, quite similar with Meduri's and Moretti's study and higher than Brochard's and Carratu's study (1,12,13,16). Although majority of patients had a diagnosis of COPD, our study consisted of a heterogenous population with different etiology of AHRF different from previous studies. However, we couldn't compare NIMV success and factors related with failure between each disease due to small number of patients with non-COPD diseases. As mentioned previously, little is known about characteristics of late failure patients. In our study, pretreatment high serum CRP level, APACHE II score, presence of bronchiectasis and pneumonia, low GCS, cough strength and compliance to NIMV and no improvement in PaO2/FiO2 after NIMV, were found as risk factors for late failure of NIMV. Also, before treatment, although there was no significant difference between group 1 and group 2 for associated complication, after NIMV there was significantly higher associated complications in group 2. In contrast, in Meduri's study, functional limitations before admission to the respiratory ICU, the presence of medical complications and a lower pH on admission and in Carratu's study, only the presence of metabolic disorders were reported as risk factors for late failure. Different from Meduri's report, in our study, there was no difference between success and late failure groups in terms of pretreatment pH and PaCO2 similar with Carratu's study.
Although little is known about the clinical and physiological characteristics of patients with late failure, it has been reported that these patients have a very poor prognosis with high mortality and this high mortality may be due to prolonged application of NIMV and a delay in intubation. Moretti et al, reported that, late failure of NIMV has a high mortality rate (67.7%) which was significantly higher if the NIMV is maintained (91.6%) than if the patient was given invasive ventilation (52.6% mortality) (12). In our study the mortality rate in late failure group was found as 73.3% consistent with previously reported poor prognosis.
CONCLUSION
In conclusion, the principal finding of our study was pretreatment high APACHE II score and CRP level, low GCS, albumin level, cough strength, bad compliance to NIMV, the presence of bronchiectasis and pneumonia and absence of improvement in PaO2/FiO2 after treatment are predictors of NIMV late failure.
AUTHORS' CONTRIBUTION
A?, AK, ?ED designed and performed study, collected data and wrote the paper. ZP?, E?, NDF collected and analyzed data and helped to write the paper.
CONFLICT of INTEREST
None declared.
REFERENCES
- Meduri GU, Turner RE, Abou-Shala N, Wunderink R, Tolley E. Non-invasive positive pressure ventilation via face mask. First-line intervention in patients with acute hypercapnic and hypoxemic respiratory failure. Chest 1996;109:179-93.
- Confalonieri M, Aiolfi S, Gandola L, Scartabellati A, Della Porta R, Parigi P. Severe exacerbation of chronic obstructive lung disease treated with BiPAP by nasal mask. Respiration 1994;61:310-6.
- Garpestead E, Brennan J, Hill NS. Non-invasive ventilation for critical care. Chest 2007;132:711-20.
- Celikel T, Sungur M, Ceyhan B, Karakurt S. Comparison of non-invasive positive ventilation with standard medical therapy in hypercapnic acute respiratory failure. Chest 1998;114:1636-42.
- Meduri GU, Abou-Shala N, Fox RC, Jones CB, Leeper KV, Wunderink RG. Non-invasive face mask ventilation in patients with acute hypercapnic respiratory failure. Chest 1991;100:445-54.
- Wood KA, Lewis L, Von Harz B, Kollef MH. The use of non-invasive positive pressure ventilation in the emergency department. Results of a randomized clinical trial. Chest 1998;113:1339-46.
- Brochard L, Isabey D, Piquet J, Amaro P, Mancebo J, Messadi AA, et al. Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. N Engl J Med 1990;323:1523-9.
- Wysocki M, Tric L, Wolff MA, Gertner J, Millet H, Herman B. Non-invasive pressure support ventilation in patients with acute respiratory failure. Chest 1993;103:907-13.
- Vitacca M, Rubini F, Foglio K, Scalvini S, Nava S, Ambrosino N. Non-invasive modalities of positive pressure ventilation improve the outcome of acute exacerbations in COPD patients. Intensive Care Med 1993;19:450-5.
- Fernandez R, Blanch L, Valles J, Baigorri F, Artigas A. Pressure support ventilation via facial mask in the hypercapnic failure in COPD patients. Intensive Care Med 1993;19:456-61.
- Kramer N, Meyer TJ, Meharg J, Cece RD, Hill NS. Randomized, prospective trial of non-invasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med 1995;151:1799-806.
- Moretti M, Cilione C, Tampieri A, Fracchia C, Marchioni A, Nava S. Incidence and causes of non-invasive mechanical ventilation failure after initial success. Thorax 2000;55:819-25.
- Carrat? P, Bonfitto P, Dragonieri S, Schettini F, Clemente R, Di Gioia G, et al. Early and late failure of non-invasive ventilation in chronic obstructive pulmonary disease with acute exacerbation. Eur J Clin Invest 2005;35:404-9.
- Jimenez P, Torres A, Roca J, Cobos A, Rodriguez-Roisin R. Arterial oxygenation does not predict the outcome of patients with acute respiratory failure needing mechanical ventilation. Eur Respir J 1994;7:730-5.
- Kaya A, Cileda? A, Cayl? I, Onen ZP, Sen E, G?lbay B. Associated factors with non-invasive mechanical ventilation failure in acute hypercapnic respiratory failure. Tuberk Toraks 2010;58:128-34.
- Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A. Non-invasive ventilation for acut exacerbations of chronic obstructive pulmonary disease. N Engl J Med 1995;333:817-22.
Yaz??ma Adresi (Address for Correspondence)
Dr. ?zlem ER?EN D?KEN
Ankara ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
06100, Cebeci, ANKARA - TURKEY
e-mail: oercen@hotmail.com