LETTER TO THE EDITOR
Doi: 10.5578/tt.7278
Tuberk Toraks 2014;62(2):174-176

Tracheoesophageal fistula in a treatment naive patient with lung cancer
?zge ?ZT?RK1, Deniz K?KSAL1, Salih EMR?1
1 Department of Chest Diseases, Faculty of Medicine, Hacettepe University, Ankara, Turkey
1 Hacettepe ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara, T?rkiye
Malignant tracheoesophageal fistula (TEF) is a serious complication of thoracic malignant diseases and is more common in esophageal cancer than in lung cancer (1,2). The largest study evaluating patients with malignant TEF and bronchoesophageal fistula reported an incidence of 0.16% in 5714 patients with lung cancer (3). Patients with TEF typically presents with coughing and shortness of breath due to aspiration of food and saliva. Recurrent respiratory infections and malnutrition leads to rapid deterioration. Life expectancy is estimated at about six weeks without proper and prompt treatment (4). In lung cancer patients, new interventions such as combination chemoradiotherapy and anti-angiogenesis agents lead to an increased risk for the development of TEF (5). Herein we would like to present a treatment naive patient with advanced stage pulmonary adenocarcinoma and TEF.
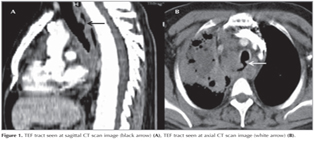
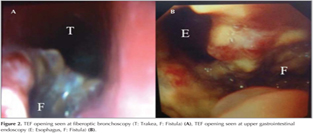
A 44-year-old male patient was admitted to our clinic with chest pain, cough, dyspnea, and difficulty in swallowing. He was diagnosed as pulmonary adenocarcinoma by percutaneous needle biopsy from the mass lesion in the right upper lobe, and was consulted to our clinic for fiberoptic bronchoscopy (FOB). He was receiving palliative cranial radiotherapy for cranial metastasis. Computed tomography (CT) of the thorax demonstrated a mass lesion in right upper lobe with a largest diameter of 7 cm and enlarged conglomerated mediastinal lymph nodes. A TEF tract was seen both on axial and sagittal CT images (Figure 1). FOB and upper gastrointestinal endoscopy revealed a large TEF (Figure 2). Since TEF was located in the proximal part of the esophagus, the patient was not found suitable for esophageal stenting. A percutaneous endoscopic gastrostomy (PEG) was performed and he was referred to an interventional pulmonology clinic for the insertion of a tracheal stent after the first cycle of chemotherapy that was applied without any serious complication.
The management of malignant TEF is primarily palliative in terms of quality of life. The therapeutic aim should be restoring the patency of the trachea and enabling the patient to be nourished. Surgery is usually considered inappropriate in malignant TEF, as the patients tend to be in poor performance status and near the end of their lives (6). Airway and esophageal stenting are safe procedures and beneficial for symptomatic relief. Some papers report high success rates in double stenting (7). When it is difficult to place double stent at the same time, a tracheal stent has priority, because an esophageal stent alone may compress the trachea and elicit respiratory distress. Plastic and silicone-cuffed stents were initially used in the management of TEF (8,9). With the use of self-expandable metallic stents (SEMS), there is an increase in quality of life of the patients. A recent study reported improvement of symptoms in 90% of patients with airway-esophageal fistula treated by insertion of esophageal SEMS (10). Herth et al, performed a prospective evaluation of airway stenting versus esophageal stenting versus double stenting of the airway and esophagus in 112 patients (83 with lung cancer, 29 esophageal cancer). Sixty five patients had airway stents, 37 had esophageal stents and 10 had double stenting as their primary intervention. The quality of life scores were significantly improved after stenting in all three groups. However the survival was significantly lower in patients who received only airway stents (11).
The American College of Chest Physicians guidelines recommended double stenting of the esophagus and airway or esophageal stenting with SEMS. They make a remark at the sequence of stenting. They suggested that the airway stent should be placed prior to the esophageal stent to minimize the risk of airway compromise if the esophageal stent is placed first (6). PEG is an alternative procedure that can be considered in palliative treatment of TEF (12). Our patient was not suitable for esophageal stenting. Since he was young and was in good performance status, we prefer to perform PEG for effective nutrition and tracheal stenting for prevention of aspirations of saliva.
CONFLICT of INTEREST
None declared.
REFERENCES
- Fitzgerald RH, Bartles DM, Parker EF. Tracheoesophageal fistulas secondary to carcinoma of esophagus. J Thorac Cardiovasc Surg 1981;82:194-7.
- Rodrigez AN, Diaz-Jimenez JP. Malignant respiratory-digestive fistulas. Curr Opin Pulm Med 2010;16:329-33.
- Martini N, Goodner JT, D'Angio GJ, Beattie EJ Jr. Tracheaoesophageal fistula due to cancer. J Thorac Cardiovas Surg 1970;59:319-24.
- Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am 2003;13:271-89.
- Spigel DR, Hainsworth JD, Yardley DA, Raefsky E, Patton J, Peacock N, et al. Tracheo-esophageal fistula formation in patients with lung cancer treated with chemoradiation and bevacizumab. J Clin Oncol 2010;28:43-8.
- Simoff MJ, Lally B, Slade MG, Goldberg WG, Lee P, Michaud GC, et al. Symptom management in patients with lung cancer. Diagnosis and management of lung cancer, 3rd ed: ACCP Guidelines. Chest 2013;143(Suppl):e455s-97s.
- Lutz F, Edith T, Heinz S, Terrence JD, Georgios S. Management of malignant esophagotracheal fistulas with airway stenting and double stenting. Chest 1996;110:1155-60.
- Hegarty MM, Angorn IB, Bryer JV, Henderson BJ, le Roux BT, Logan A. Palliation of malignant esophago-respiratory fistulae by permanent indwelling prosthetic tube. Ann Surg 1977;185:88-91.
- Hordijk ML, Dees J, van Blankenstein M. The management of malignant esophago-respiratory fistulas with a cuffed prosthesis. Endoscopy 1990;22:241-4.
- Ross WA, Alkassab F, Lynch PM, Ayers GD, Ajani J, Lee JH, et al. Evolving role of self expanding metal stents in the treatment of malignant dyshagia and fistulas. Gastrointestinal Endosc 2007;65:70-6.
- Herth FJF, Peter S, Baty F, Eberhardt R, Leuppi JD, Chhajed PN. Combined airway and esophageal stenting in malignant airway-esophageal fistulas: a prospective study. Eur Respir J 2010;36:1370-4.
- Vanis N, Saray A, Gornjakovic S, Mesihovic R. Percutaneous endoscopic gastrostomy (PEG): Retrospective analysis of a 7-year clinical experience. Acta Inform Med 2012;20:235-7.
Yaz??ma Adresi (Address for Correspondence)
Dr. Deniz K?KSAL
Hacettepe ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
ANKARA - TURKEY
e-mail: deniz_koksal@yahoo.com