LETTER TO THE EDITOR
Doi: 10.5578/tt.6512
Tuberk Toraks 2014;62(1):91-94

Dev ?ntrapulmoner Malign Lokalize Fibroz T?m?r: Olgu Sunumu
B?lent Mustafa YEN?G?N1, ?i?dem GONCA1, Murat ?ZKAN1, Cabir Y?KSEL1, Serkan EN?N1, Hakan KUTLAY2
1 Ankara ?niversitesi T?p Fak?ltesi, ?bn-i Sina Hastanesi, G???s Cerrahisi Anabilim Dal?, Ankara, T?rkiye
1 Department of Chest Surgery, Faculty of Medicine, Ankara University, Ibn-i Sina Hospital, Ankara, Turkey
2 Ankara ?niversitesi T?p Fak?ltesi, G???s Cerrahisi Anabilim Dal?, Ankara, T?rkiye
2 Department of Chest Surgery, Faculty of Medicine, Ankara University, Ankara, Turkey
INTRODUCTION
The primary tumors of the pleura are usually examined under two headings: diffuse and localized tumors. In the localized form, there is no relationship with asbestosis (1). Localized fibrous tumors were previously known by names such as benign mesothelioma, submesothelial fibroma and localized fibrous mesothelioma. Today, they are usually referred as localized fibrous tumors (2). These tumors comprise 10% of all pleural tumors. Even though they generally display benign histological behavior, there is a 12% prevalence of malignancy (3). Our case was believed to be worthy of presenting as it was intrapulmonary, giant, and displayed malignant behavior, which is rare.
CASE REPORT
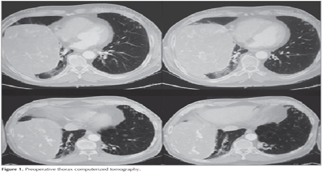
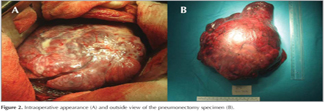
A 64-year-old male patient presented to our clinic with complaints of increasing dyspnea and coughing in the last two years. On physical examination, clubbing that had become more distinct in the last two years was found. No significant trait existed in the patient's history. Sedimentation rate was 55 mm/hour and pH: 7.43, pO2: 49.9 mmHg, pCO2: 30.6 mmHg, O2 saturation 91% in arterial blood gas. Other examinations including complete blood count and serum chemistry showed no abnormality. Chest X-ray showed homogeneous opacity with smooth margins in the right hemithorax. Thorax computerized tomography showed a solid mass lesion which almost completely covered the right hemithorax, extended to the diaphragmatic surface, was pleural based and approximately 19 x 17 x 14 cm in size, included multiple calcified regions, displayed heterogenity following IV contrast injection, with cystic and necrotic components and smooth lobular contours (Figure 1). When right posterolateral thoracotomy procedure performed, a mass located in the lower lobe primarily, invading the middle and upper lobes via transfissural way, was observed. Right pneumonectomy with mediastinal lymph node sampling was done after (Figure 2). The histopathological examination was reported as localized fibrous tumor. Because of the large size of tumor (21 x 19 x 14 cm), involving necrosis and mitotic activity of 5 at times in each 10 high magnification field, lesion was assessed as malignant. The patient was discharged on postoperative day 5 without any morbidity. No additional therapy was recommended by the oncologists for the patient.
Discussion
Even though localized fibrous tumors of the pleura are reported in all age groups, they are most common in the 5th and 6th decades of life. They were first classified in 1931 by Klemperer and Rabin as diffuse mesothelioma and localized mesothelioma. No difference has been noted in its prevalence among male and females. More than 50% of the patients are asymptomatic (1). These tumors are mostly detected incidentally in chest X-rays. Depending on their localization, chest pain, dyspnea and hemoptysis may be seen. Malignant tumors have an increased chance of being symptomatic. More rarely, systemic symptoms such as fatigue, sweating, weight loss, osteoarthropathy, clubbing and hypoglycemia may be seen. Hypertrophic pulmonary osteoarthropathy (Pierre-Marie-Bamberge syndrome) was defined in 20% of the cases (4,5). Osteolysis may develop due to the hyaluronic acid synthesized by the tumor, followed by new bone formation. There is ample evidence for the role of the insulin-mimicking growth factor II released from the tumor cells in causing hypoglycemia (Doege-Potter syndrome). Three or four months after the resection of the tumor, hypoglycemia usually disappears. The incidence of hypoglycemia is reported as 2-4% in the literature (4,6). While our patient displayed dyspnea and clubbing due to the tumor invading a large lung parenchyma area, osteoarthropathy or hypoglycemia symptoms were not detected.
Thorax computerized tomography is the golden standard imaging method for these patients. However, as there is lung parenchyma around tumors developing from the interlobar fissure, distinguishing them from intraparenchymal masses is rather difficult (1). While surgery was planned for our patient owing to the extrapulmonary mass showed radiologically in the preoperative period, intraoperative exploration showed that lesion was intraparenchymal. Magnetic resonance imaging has a limited role in the diagnosis of pleural diseases. However, it clearly shows the relationship between mediastinal and major vascular structures with localized fibrous tumors. When the tumor is localized on the diaphragm, it assists the establishment of intrathoracic localization. The transthoracic needle biopsy performed before surgery for diagnostic purposes generally remains non-diagnostic. Cytopathological examination is also rather difficult (6). Invasive procedures were not considered for preoperative diagnosis of our patient.
Complete surgical resection is the primary treatment method for all localized fibrous tumors, whether benign or malignant (4). The suggested distance for surgical margins without a tumor is 1-2 cm. While wedge resection is sufficient for pedicled tumors, resection may be difficult in broad based tumors. Lobectomy or pneumonectomy may be required at times. Making an intraoperative pathological assessment with frozen section before resection can only be helpful in determining safe surgical margins. If parietal pleura invasion is seen, extrapleural dissection is necessary (1,7). Parietal pleura invasion was not seen in our case. Pneumonectomy was performed as the vascularly rich tumor tissue made it difficult during dissection to control bleeding and showing a complete intraparenchymal location.
The best prognostic determinant for localized fibrous tumors, regardless of displaying benign or malignant behavior, is whether complete resection was performed or not. Prognosis is worse in recurrence seen patients. If the recurring tumor is resectable, re-resection may be considered. Recurrence rate in benign pedicled tumors is less than 2%. In broad based, invading tumors with benign behavior, is under 8%. In malignant pedicled tumors, recurrence rate is 14%, and in broad based, invading tumors with malignant behavior it rises to 63%. Adjuvant therapy is recommended only for the patients in the latter group. All these recurrence rates are valid for patients in whom complete resection can be performed. Chest X-rays and thorax computerized tomography is recommended every six months during the first 2 years, and once yearly thereafter in the follow-up period (1,8). The 6 months follow-up of our patient showed no clinical or radiological finding of recurrence.
CONFLICT of INTEREST
None declared.
REFERENCES
- de Perrot M, Fischer S, Br?ndler MA, Sekine Y, Keshavjee S. Solitary fibrous tumors of the pleura. Ann Thorac Surg? 2002;74(1):285-93.
- Travis WD, Brambilla E, M?ller-Hermelink HK, et al. WHO Classification of Tumours Pathology and Genetics of the Lung, Pleura, Thymus and Heart IARC Press, Lyon, 2004:141-4.
- Hirai A, Nakanishi R. Solitary fibrous of the pleura with hypoglycemia associated with serum insulin-like growth factor II. J Cardiovascular Surg 2006;132:713-4.
- Cardillo G, Carbone L, Carleo F, Masala N, Graziano P, Bray A, et al. Solitary fibrous tumors of the pleura: an analysis of 110 patients treated in a single institution. Ann Thorac Surg? 2009;88(5):1632-7.
- Harrison-Phipps KM, Nichols FC, Schleck CD, Deschamps C, Cassivi SD, Schipper PH, et al. Solitary fibrous tumors of the pleura: results of surgical treatment and long-term prognosis. J Thorac Cardiovasc Surg 2009;138(1):19-25.
- Rena O, Filosso PL, Papalia E, Molinatti M, Di Marzio P, Maggi G, et al. Solitary fibrous tumour of the pleura: surgical treatment. Eur J Cardiothorac Surg? 2001;19(2):185-9.
- Filosso PL, Asioli S, Ruffini E, Rovea P, Macri' L, Sapino A, et al. Radical resection of a giant, invasive and symptomatic malignant Solitary Fibrous Tumour (SFT) of the pleura. Lung Cancer? 2009;64(1):117-20.
- Graadt Roggen JF, Hogendoorn PCW. Solitary fibrous tumour: the emerging clinicopathologic spectrum of an entity and its differential diagnosis. Curr Diagnosis Pathol 2004;10:229-35.
Yaz??ma Adresi (Address for Correspondence)
Dr. B?lent Mustafa YEN?G?N
Ankara ?niversitesi T?p Fak?ltesi,
?bn-i Sina Hastanesi,
G???s Cerrahisi Anabilim Dal?,
ANKARA - TURKEY
e-mail: drbulent18@gmail.com