RESEARC ARTICLE
Doi: 10.5578/tt.6226
Tuberk Toraks 2014;62(1):39-44

Ast?ml? ?ocuklarda Obezite Daha K?t? Kontrol ile ?li?kili mi?
?zge YILMAZ1, Ayhan S???T1, Arda BOZG?L2, Ahmet T?RKEL?1, ?ebnem KADER2, Hasan Y?KSEL1
1 Celal Bayar ?niversitesi T?p Fak?ltesi, Pediatrik Allerji ve Pulmonoloji Anabilim Dal?, Manisa, T?rkiye
1 Department of Pediatric Allergy and Pulmonology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
2 Celal Bayar ?niversitesi T?p Fak?ltesi, Pediatri Anabilim Dal?, Manisa, T?rkiye
2 Department of Pediatrics, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
?ZET
Ast?ml? ?ocuklarda Obezite Daha K?t? Kontrol ile ?li?kili mi?
Giri?: Ast?m ve obezite ili?kili hastal?klard?r ancak obezitenin ast?m a??rl???na etkisi hen?z net de?ildir. Bu nedenle, ?al??mam?z?n amac? obezite ile semptomlar ve ast?m kontrol anketi (ACQ) ile de?erlendirilen ast?m kontrol?n?n ili?kisini de?erlendirmektir.
Materyal ve Metod: ?al??maya 4-14 ya?lar? aras?ndaki 98 ?ocu?u ba?vuru s?ras?yla dahil ettik ve hastal?k ?zellikleri, a??rl?k parametreleriyle birlikte semptom skorlar?n? kaydettik. T?m ?ocuklar ACQ'yu doldurdu. ?ocuklar beden kitle indeksine g?re obez ve obez olmayan olarak s?n?fland?r?ld?. Obezite, beden kitle indeksinin 90 persentil ?zerinde olmas? ?eklinde tan?mland?.
Bulgular: Obez gruptaki (n= 27) ?ocuklar?n ortalama ya?? 8.1 ? 2.6 iken, obez olmayan gruptaki (n= 71) ?ocuklar?n ya?? 8.6 ? 2.9 idi (p= 0.41). Ast?m semptom skoru obez ve obez olmayan gruplar aras?nda anlaml? derecede farkl? de?ildi (p= 0.73). Obez gruptaki ?ocuklar obez olmayan gruptakilere g?re daha d???k ACQ puan?na sahipti (s?ras?yla 1.2 ? 0.9 ve 1.7 ? 1.0, p= 0.04) ancak bu farkl?l?k regresyon modelinde ya? ve cinsiyete g?re d?zeltme yap?l?nca kayboldu.
Sonu?: Bu ?al??man?n bulgular?, obezitenin, ya? ve cinsiyete g?re d?zeltme yap?ld???nda daha k?t? ast?m kontrol? ile ili?kili olmad???n? g?stermektedir.
Anahtar kelimeler: Ast?m, obezite, ast?m kontrol?, ast?m kontrol anketi, ?ocuk
SUMMARY
Is Obesity Related to Worse Control in Children with Asthma?
Introduction: Asthma and obesity are related diseases however the influence of obesity on asthma severity is not clear yet. Therefore, the aim of our study was to evaluate the association between obesity and asthma control evaluated on the basis of symptoms and asthma control questionnaire (ACQ).
Materials and Methods: We enrolled 98 children with asthma aged 4 to 14 years consecutively and recorded their disease characteristics and severity parameters as well as the symptom scores. All children filled in the ACQ. Children were classified as obese and non-obese according to body mass index. Obesity was defined as body mass index over 90th percentile.
Results: Mean age of the children in the obese group (n= 27) was 8.1 ? 2.6 while that in the non-obese group (n= 71) was 8.6 ? 2.9 (p= 0.41). Asthma symptom score in obese and non-obese groups were not significantly different (p= 0.73). Children in the obese group had lower ACQ scores when compared to the non-obese group (1.2 ? 0.9 vs 1.7 ? 1.0, p= 0.04) however this significance was lost when controlled for age and gender in the regression model.
Conclusion: The results of this study suggest that obesity is not significantly associated with worse asthma control when adjusted for age and gender.
Key words: Asthma, obesity, asthma control, asthma control questionnaire, child
INTRODUCTION
There is a relationship between the trend towards obesity and asthma. Moreover, it has been reported that asthma symptoms are associated with obesity (1). Different hypothesis has been proposed regarding this relationship between obesity and asthma. First one relies on the facts that obesity leads to a decrease in lung volumes including the tidal volume which may increase airway obstruction, adipose tissue derived hormones and cytokines such as leptin, adiponectin, tumor necrosis factor and interleukins play an inflammatory role (2). Moreover diseases associated with obesity such as gastro-esophageal reflux and sleep disordered breathing may worsen asthma (2). However, there are contradictory results in both adult and childhood researches about the association of obesity with severity of asthma (2,3,4,5,6). Some report that obesity increases asthma symptom and severity while some report that obesity does not have a significant influence on asthma severity and control (3,4,5,6).
Current guidelines including the Global Initiative for Asthma (GINA) support the idea that asthma treatment needs to be based on patient reported outcomes and control (7). It has been emphasized that health related quality of life needs to be included in the concept of control besides symptom control. This requires the use of validated questionnaires for estimation of control since subjective evaluation of the physician may not be adequate (8,9). Moreover, many different factors including socioeconomic status, mood of the child and parent as well as treatments used may influence asthma control (10,11). Therefore, it is important to assess different factors that may influence asthma control to target them in the action plan of asthma treatment. Therefore, the aim of this study was to evaluate the association between obesity and asthma control evaluated on the basis of symptomatology and quality of life (QoL).
MATERIALS and METHODS
Study Population
Ninety eight children aged between 4 and 14 years diagnosed with asthma were included in the study before any treatment was initiated. Children who had received inhaled steroid treatment before and the ones who didn't agree to participate were excluded.
Study Design
At the time of enrollment, disease characteristics of the children including number of exacerbations, requirement of nebulized bronchodilators, requirement of hospitalization days, presentation to an outpatient department or emergency department for asthma symptoms during the previous three month period were recorded. Moreover, asthma symptom score was also reported. Asthma control questionnaire (ACQ) was applied to all the children at the time of enrollment.
Heights of all children included in the study were measured via a stadiometer and weight was measured by an electronic scale under the supervision of the researchers. Weight was measured on a scale by the pediatrician in charge of the study. Body mass index (BMI) was calculated according to the formula [weight (kg)/(height (m)2]. BMI percentiles were classified according to four standardized percentile curves as 75th percentile, 76th to 90th percentile, 91st to 95th percentile, and 96th to 100th percentile (12). Children with a BMI over 90th percentile were defined as obese.
The study was approved by the Institutional Ethic Boards of Celal Bayar University and carried out in accordance with principle of Declaration of Helsinki.
Asthma Control Questionnaire
Asthma control questionnaire developed by Juniper et al. aims to assess the adequacy of asthma control and is composed of 7 questions (13). Five of the questions are about symptoms of asthma during the previous 7 days and one question is about inhaled bronchodilator use during the same time period. The last question is about FEV1% predicted which is filled in by clinical staff. However, because this study included children aged between 6 and 15 and since most of the children did not cooperate with spirometry adequately, this last question was not assessed in our study. It has been shown that shortened versions of ACQ omitting the FEV1 question is also valid in clinical trials (14).
Patient Reported Asthma Symptom Score
Asthma symptom score that was used in this study included 5 items reflecting chronic asthma symptoms such as dyspnea, tightness in chest, day-time wheeze, nocturnal wheeze, daily performance during the previous three months period (15). Scoring of the items increase from 0 to 3 as the severity increased. Total score is expressed as sum of all item scores.
Statistical Analysis
Chi-square test was used to compare the frequencies of gender between the obese and non-obese groups. Non-parametric tests were used to compare age means and asthma characteristics like days of hospitalization and number of exacerbations during the last three months and acq scores since these values were not normally distributed. Regression model was formed between presence of obesity, gender and age and ACQ score. p values less that 0.05 were regarded as statistically significant.
RESULTS
Sociodemographic Characteristics of the Study Population
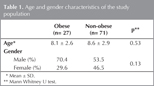
Mean age of the children in the obese group (n= 71) was 8.1 ? 2.6 while that in the non-obese group (n= 27) was 8.6 ? 2.9 (p= 0.53). Gender distribution was similar between the two groups (p= 0.13) (Table 1).
Asthma Characteristics of the Study Population
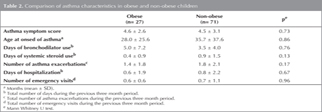
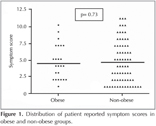
Asthma characteristics of the obese and non-obese groups were not statistically different (Table 2). Asthma symptom score in the obese group was 4.6 ? 2.6 while that in the non-obese group was 4.5 ? 3.1 (p= 0.73) (Figure 1). Age at onset of asthma symptoms was reported as 28.0 ? 25.6 months in obese children whereas that in the non-obese children was 35.7 ? 37.6 months (p= 0.86). Disease severity characteristics including days of bronchodilator and systemic steroid requirement as well as number of asthma exacerbations during the previous three month period were similar between the two groups (p> 0.1 for all). Number of hospitalization days and emergency department visits were not statistically different in obese and non-obese groups, either (0.6 ? 1.9 vs. 0.8 ? 2.2, p= 0.67 and 0.6 ? 0.6 vs. 0.7 ? 1.1, p= 0.96 respectively) (Table 2).
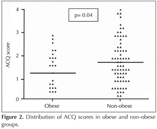
Asthma Control Questionnaire Scores of the Study Population
Children in the obese group had significantly lower ACQ scores when compared to the non-obese group (1.2 ? 0.9 vs. 1.7 ? 1.0, p= 0.04) (Figure 2). However, this significance was lost when controlled for age and gender in the regression model.
DISCUSSION
Asthma is more prevalent in obese individuals and both weight gain and weight loss influence asthma outcomes (2). Therefore, it has long been hypothesized that obesity is associated with asthma but the exact pathogenesis mechanism underlying this association is unclear (2). Some authors accuse obesity in pathogenesis of asthma while some regard obesity as the outcome and asthma as the risk factor (5). It has been demonstrated that obesity is an important determinant of reduced lung function test results and a risk factor for atopy in children (16). However, it has also been proposed that low energy expenditure due to the inactivity in asthma may be a risk factor for development of obesity (5). Therefore, there are many aspects to the association between asthma and obesity. Current guidelines set the target of asthma treatment as achievement of disease control including QoL besides symptom control (7). Many previous research have evaluated control in terms of symptomatology and requirement of medications but not QoL. Achievement of asthma control requires addressing many different factors that may influence it including sociodemographic characteristics, mood of the parent and child, medication adherence and many more (10,11). Therefore, it is important to assess different factors that may influence asthma control besides the treatment and the aim of this study was to evaluate the association between obesity and asthma control.
There are contradictory results about asthma control in patients with asthma. An adult study failed to find an association between asthma control and obesity using four different control questionnaires including ACQ and asthma control test (3). This is similar to our results, because influence of obesity on ACQ was lost when adjusted for age and gender in our population. On the other hand, contradictory to our results, another study on adult subjects has reported that obesity was associated with worse asthma outcomes using mini-Asthma Quality of Life Questionnaire, the Asthma Therapy Assessment Questionnaire (4). This difference might be attributable to the difference in the study populations because childhood asthma has many aspects different from adult asthma.
Similar studies have been performed on children, too. One of these studies demonstrated that asthma was associated with obesity however they failed to demonstrate a correlation between obesity and disease severity (5). However, they had classified asthma as mild-moderate and moderate-severe and not according to the control level and severity is not synonymous to control (5,17). Similarly, another study demonstrated that obesity was more common in children with asthma when compared to the general population. However, they also did not detect a difference in asthma control measured by asthma control test between obese and non-obese asthmatics (6). A study on adolescents with asthma demonstrated that obesity was more frequent and that was associated with higher asthma morbidity (18). This has lead to the conclusion coexisting obesity and asthma cases a dual burden (18). Obesity does not influence only disease severity but also response to inhaled corticosteroid treatment (19). Our study was a cross-sectional one therefore we did not analyze for response to treatment. But similar to above mentioned studies, our results indicated that ACQ scores were similar between obese and non-obese asthmatics when adjusted for age and gender. Adjustment for age and gender was performed because it has been reported that age might influence perception of asthma symptoms in children and that gender is a factor influencing asthma control (20,21).
Obese and non-obese children with asthma reported similar number hospitalization days, asthma exacerbations, days of bronchodilator requirement and emergence/department visits during the previous three month period. This was in concordance with the lack of difference between ACQ scores when adjusted for age and sex.
Moreover, our results did not show a significant difference in the age at onset of asthma findings and obesity. This is in contrast to the previous study in adolescent asthmatics that demonstrated a younger age of asthma onset in obese adolescents (18). However, this might be attributed to the relatively younger age group included in our study.
The results of our study demonstrated that asthma control was significantly worse in girls when compared to the boys but subjective reports of symptom scores were similar between the two genders. This is in concordance with previous studies which have also reported that association between asthma and obesity was influenced by gender and some has reported that BMI was associated with asthma in females but not in males (21,22).
Major limitation of this study was the absence of lung function test results. However, the aim of the study was to assess the association between obesity and asthma control using subjective and objective questionnaire based scoring therefore spirometry was not performed. Moreover, some children younger than five years age could not cooperate to perform spirometry. The second limitation is the cross sectional design which precluded us from making causal inferences. Our results did not show a significant association between asthma control and obesity however, a prospective study that assesses the change in asthma control with the change in BMI might give more information about this association.
In conclusion, although asthma and obesity have been shown to be associated epidemiologically, the results of this study suggest that obesity is not significantly associated with asthma control when adjusted for age and gender. Moreover, asthma control is worse in females when compared to males. However, prospective cohort studies are needed to provide a more direct way of assessing the causal relationship between these two disease entities.
CONFLICT of INTEREST
None declared.
REFERENCES
- Tai A, Volkmer R, Burton A. Association between asthma symptoms and obesity in preschool (4-5 year old) children. J Asthma 2009;46:362-5.
- Shore SA. Obesity and asthma: lessons from animal models. J Appl Physiol 2007;102:516-28.
- Clerisme-Beaty EM, Karam S, Rand C, Patino CM, Bilderback A, Riekert KA, et al. Does higher body mass index contribute to worse asthma control in an urban population? J Allergy Clin Immunol 2009;124:207-12.
- Mosen DM, Schatz M, Magid DJ, Camargo CA Jr. The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol 2008;122:507-11.
- Gennuso J, Epstein LH, Paluch RA, Cerny F. The relationship between asthma and obesity in urban minority children and adolescents. Arch Pediatr Adolesc Med 1998;152:1197-200.
- Ross KR, Hart MA, Storfer-Isser A, Kibler AM, Johnson NL, Rosen CL, et al. Obesity and obesity related co-morbidities in a referral population of children with asthma. Pediatr Pulmonol 2009;44:877-84.
- The global strategy for asthma management and prevention (GINA) updated 2012. www.ginasthma.com
- Juniper EF. Assessing asthma control. Curr Allergy Asthma Rep 2007;7:390-4.
- Juniper EF, Bousquet J, Abetz L, Bateman ED; GOAL Committee. Identifying 'well-controlled' and 'not well-controlled' asthma using the Asthma Control Questionnaire. Respir Med 2006;100:616-21.
- de Vries MP, van den Bemt L, Lince S, Muris JW, Thoonen BP, van Schayck CP. Factors associated with asthma control. J Asthma 2005;42:659-65.
- Bender B, Zhang L. Negative affect, medication adherence, and asthma control in children. J Allergy Clin Immunol 2008;122:490-5.
- Hammer LD, Kraemer HC, Wilson DM, Ritter PL, Dornbusch SM. Standardized percentile curves of body-mass index for children and adolescents. Am J Dis Child 1991;145:259-63.
- Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J 1999;14:902-7.
- Juniper EF, Svensson K, M?rk AC, Stahl E. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med 2005;99:553-8.
- Yuksel H, Sogut A, Yilmaz O, Demet M, Ergin D, Kirmaz C. Evaluation of sleep quality and anxiety-depression parameters in asthmatic children and their mothers. Respir Med 2007;101:2550-4.
- Spathopoulos D, Paraskakis E, Trypsianis G, Tsalkidis A, Arvanitidou V, Emporiadou M, et al. The effect of obesity on pulmonary lung function of school aged children in Greece. Pediatr Pulmonol 2009;44:273-80.
- Lang DM. New asthma guidelines emphasize control, regular monitoring. Cleve Clin J Med 2008;75:641-53.
- Abramson NW, Wamboldt FS, Mansell AL, Carter R, Federico MJ, Wamboldt MZ. Frequency and correlates of overweight status in adolescent asthma. J Asthma 2008;45:135-9.
- Peters-Golden M, Swern A, Bird SS, Hustad CM, Grant E, Edelman JM. Influence of body mass index on the response to asthma controller agents. Eur Respir J 2006;27:495-503.
- Kopel SJ, Walders-Abramson N, McQuaid EL, Seifer R, Koinis-Mitchell D, Klein RB, et al. Asthma Symptom Perception and Obesity in Children. Biol Psychol 2009 Nov 24.
- Ahmad N, Biswas S, Bae S, Meador KE, Huang R, Singh KP. Association between obesity and asthma in US children and adolescents. J Asthma 2009;46:642-6.
- Sood A, Qualls C, Arynchyn A, Beckett WS, Gross MD, Steffes MW, et al. Obesity-asthma association: is it explained by systemic oxidant stress? Chest 2009;136:1055-62.
Yaz??ma Adresi (Address for Correspondence)
Dr. Hasan Y?KSEL
Celal Bayar ?niversitesi T?p Fak?ltesi,
Pediatrik Allerji ve Pulmonoloji Anabilim Dal?,
MAN?SA - TURKEY
e-mail: hyukselefe@hotmail.com