RESEARC ARTICLE
Doi: 10.5578/tt.7013
Tuberk Toraks 2014;62(1):1-6

Sigara ve ?? Ortam Hava Kirlili?inin T?berk?loza Etkisi:
Sigara, T?berk?loz, ?? Ortam Hava Kirlili?i
Ay?e Bilge ?ZT?RK1, Zeki KILI?ASLAN2, Halim ??SEVER3
1 Medeniyet ?niversitesi, G?ztepe E?itim ve Ara?t?rma Hastanesi, Eri?kin Allerji ?nitesi, ?stanbul, T?rkiye
1 Adult Allergy Unit, Medeniyet University, Goztepe Training and Research Hospital, Istanbul, Turkey
2 ?stanbul ?niversitesi ?stanbul T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?stanbul, T?rkiye
2 Department of Chest Diseases, Faculty of Istanbul Medicine, Istanbul University, Istanbul, Turkey
3 ?stanbul ?niversitesi ?stanbul T?p Fak?ltesi, Halk Sa?l??? Anabilim Dal?, ?stanbul, T?rkiye
3 Department of Public Health, Faculty of Istanbul Medicine, Istanbul University, Istanbul, Turkey
?ZET
Sigara ve ?? Ortam Hava Kirlili?inin T?berk?loza Etkisi: Sigara, T?berk?loz, ?? Ortam Hava Kirlili?i
Giri?: Epidemiyolojik ?al??malar sigara ile t?berk?loz art??? aras?nda bir ili?ki bildirmesine ra?men, i? ortam hava kirlili?i ve t?berk?loz aras?ndaki ili?ki net olarak anla??lm?? de?ildir. S?n?rl? say?daki ?al??malar sigara ve i? ortam hava kirlili?inin t?berk?loz patogenezinde rol oynayabilece?ini d???nd?rmektedir. Bu ?al??mada, sigara ve i? ortam hava kirlili?inin aktif t?berk?loz riski ?zerine olan etkisini ara?t?rd?k.
Materyal ve Metod: Bu prospektif, ya?a g?re e?le?tirilmi? bir olgu kontrol ?al??mas?d?r. ?? y?z altm?? iki aktif t?berk?lozlu ve 409 sa?l?kl? kontrol ?al??maya dahil edildi. T?m kat?l?mc?lara y?z y?ze sigara i?me al??kanl???, miktar? ve sigara i?me s?resi, ki?i ba??na d??en oda say?s?, ailenin ayl?k geliri, ?s?nma sistemi ve ?evresel t?t?n duman? maruziyetini i?eren bir anket formu dolduruldu.
Bulgular: Sigara i?en hastalar sigara i?meyen hastalara k?yasla 5 kat daha fazla aktif t?berk?loz riskine sahipti (%95 CI: 3.2-7.5, p< 0.0001). Benzer ?ekilde, i? ortam? ?s?tmak i?in k?m?r veya odun kullanan hastalarda 1.6 kat daha y?ksek t?berk?loz riski vard? (%95 CI: 1.179-2.305, p< 0.003). Az gelirli ki?iler (< 200 Euro/ay) y?ksek gelirli olanlarla kar??la?t?r?ld???nda t?berk?loza sahip olma oran? 3.2 kat fazlayd? (%95 CI: 2.113-5.106, p< 0.0001). A??r sigara i?icisi olmak (≥ 20 paket/y?l, p< 0.0001) ve sigaraya ba?lama ya?? (< 16 ya?, p< 0.041) aras?nda anlaml? bir ili?ki vard?. ?evresel t?t?n duman? maruziyeti ve t?berk?loz aras?nda anlaml? bir ili?ki yoktu.
Sonu?: Sigara ve i? ortam hava kirlili?i t?berk?loz riskini art?rabilir. Sigara, sosyoekonomik ko?ullar, i? ortam hava kalitesi ve t?berk?loz aras?nda karma??k bir ili?ki vard?r. Sonu?lar?m?z, etkili bir i? ortam hava kalitesi kontrol?n?n t?berk?loz riskini ?nlemeye yard?mc? olabilece?ini d???nd?rmektedir.
Anahtar kelimeler: T?berk?loz, sigara, i? ortam hava kirlili?i, ?evresel t?t?n duman?
SUMMARY
Effect of Smoking and Indoor Air Pollution on the Risk of Tuberculosis: Smoking, Indoor Air Pollution and Tuberculosis
Introduction: Although epidemiological studies have reported an association between smoking and increases in tuberculosis, the relationship between indoor air pollution and risk of tuberculosis is not fully understood. A limited number of studies have suggested that smoking and indoor air pollution may play a role in the pathogenesis of tuberculosis. In this study, we investigated the effect of smoking and indoor air pollution on the risk of active tuberculosis.
Materials and Methods: It is prospectively recorded age matched case-control study. Three hundred sixty two active tuberculosis cases and 409 healthy controls were included to the study. All participants were interviewed face to face by using a questionnaire including smoking habit, quantity and duration of smoking, number of room/person in the house, monthly income of the family, indoor heating system, and environmental tobacco smoke.
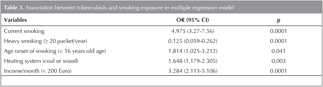
Results: Patients who smoke had a five fold (95% CI: 3.2-7.5, p< 0.0001) higher odds of having active tuberculosis compared with patients who do not smoke. Similarly, patients using coal or wood for indoor heating had a 1.6 fold (95% CI: 1.179-2.305, p< 0.003) higher odds having tuberculosis. People who have less income (< 200 Euro/month) had 3.2 fold (95% CI: 2.113-5.106, p< 0.0001) higher odds of having tuberculosis compared with people having high income. There was a significant correlation between heavy smoking (≥ 20 packet/year, p< 0.0001) and age onset of smoking (< 16 years of age, p< 0.041). There was no significant association between environmental tobacco smoke and tuberculosis.
Conclusion: Smoking and indoor air pollution may increase the risk of tuberculosis. There is a complex interaction between smoking, socioeconomic conditions, indoor air quality and tuberculosis. Our results suggest that effective indoor air quality control could help to prevent tuberculosis risk.
Key words: Tuberculosis, smoking, indoor air pollution, environmental tobacco smoke
INTRODUCTION
Tuberculosis is an epidemic airborne disease caused by Mycobacterium tuberculosis, which infects one third of the world's population (1). In 2008, tuberculosis incidence is 30 per 100.000 people, in Turkey and a total of 16.551 tuberculosis patients are detected by the dispensaries in 2010 (1). Tuberculosis incidence is decreasing over the time in Turkey by the effective treatment strategies. However it is still an important public health problem for our country.
Recent studies have demonstrated that increased respiratory health is strongly associated with clean environmental air (2). We spend most of our time indoors, so breathing healthy air where we live is critical. Based on the National Household Study conducted in 2003, smoking prevalence in adults is %32.1 (3). Smoking prevalence is much more in males and it is remarkable that many smokers are smoking mostly in their homes (4). There are many evidences that there is a strong association between indoor air quality, smoking and tuberculosis (5,6,7,8,9,10). However, the association between smoking, indoor air pollution and tuberculosis is not yet fully understood. In 2010, World Health Organisation (WHO) has proposed that greater emphasis be given to primary preventive activities addressing risk factors of tuberculosis (11). However, indoor air quality standards have not yet received sufficient attention in terms of tuberculosis care standards. In Turkey, people with low socioeconomic status, live in a crowded, small, and inadequate ventilated homes, particularly in large cities and the objective of this study is to investigate the effect of smoking and indoor air pollution on the risk of active tuberculosis in Istanbul.
Materials and Methods
Cases-Controls
This matched case control study was conducted in Istanbul. Cases were 362 new tuberculosis patients receiving their treatments in Yedikule Centre for Chest Diseases and Thoracic Surgery and Sureyyapasa Centre for Chest Diseases and Thoracic Surgery. Cases were defined as men aged between 15-70 years who were sputum smear and/or culture positive for pulmonary tuberculosis. Men aged 15-70 years who were screened and declared not to have tuberculosis formed the control group. Since the prevalence of tobacco smoking among women in Turkey is low 18%, women were not included in this study (3). The patients having diabetes, HIV infection, chronic kidney failure, and receiving any immunosuppressive drugs were also excluded. Age matched 408 healthy controls were selected from subjects who applied to dispensaries and screened by chest symptoms and chest radiograph for health report.
Exposure to Tobacco and Indoor Air Pollution
After informed consent was obtained, an experienced pulmonologist administered a questionnaire containing demographic information, smoking habits, quantity and duration of smoking, number of room/person in the house, monthly income of the family, indoor heating system, and environmental tobacco smoke. All participants were interviewed face to face by using this questionnaire. Smoking status classified as current smoker (current smoker is someone who has smoked greater than 100 cigarettes in lifetime and now smokes every day or some days), never-smoker (never smoker is someone who currently does not smoke any cigarettes and has not smoked greater than 100 cigarettes in lifetime), ex-smoker (ex-smoker is someone who used to smoke cigarettes regularly and not smoking at least a year) and passive smoker (passive smoker is someone who has not smoked and exposed to environmental tobacco smoke in the home) (12). Also an adopted questionnaire was used to define environmental tobacco smoke in details (13). Indoor air pollution exposure was defined as use of solid fuel such as coal, and wood for indoor heating. The study was approved by local ethic committee.
Statistical Analysis
The null hypothesis is that exposure to indoor air pollution and tobacco smoking is not associated with tuberculosis. The smoking habit and exposure to indoor air pollution as defined above are the main risk factors. The association between tuberculosis and potential risk factors was investigated. Chi-square and Student's t-test were used for categorical and continuous variables, respectively. An independent association between tuberculosis and smoking and indoor air pollution was assessed using a multiple logistic regression model. Factors which were significantly associated with tuberculosis in the univariate analysis were selected as variables for the logistic regression model. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to indicate the model findings. Statistical significance was defined for p values less than 0.05. SPSS Microsoft Windows Release 10.0 was used for statistical analysis.
Results
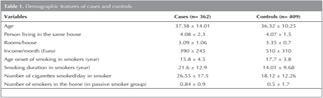
The mean age of the cases and controls were 37.38 ? 14.01 and 36.32 ? 10.25 years, respectively. Demographic details of the cases and controls are given in Table 1. Among the 362 cases, 74.7% (n= 270) were current smokers. 293 (89.3%) patients were smokers (current + ex-smoker). The age onset of smoking was < 16 years of age in 60% of the cases. Among the tuberculosis cases 55.3% (n= 200) were heavy smokers (≥ 20 packet/year), and 55% of the non-smokers are exposed to environmental tobacco smoke.
Among the control group, 55% (n= 225) were current smoker. 255 (62%) patients were smokers in control group. The age onset of smoking was < 16 years of age in 41% of the controls. Among the tuberculosis cases 23.5% (n= 96) were heavy smokers (≥ 20 packet/year), and 44% of non-smoker are exposed to environmental tobacco smoke.
The proportion of cases using coal or wood for heating in their home was 71.9% (n= 260). Among the controls, 232 subjects (57%) were using coal and wood for heating. Among cases, there was a mean of 3.08 (range 1-23) persons living in their house, and a mean of 2.09 (range 1-8) rooms per house. The proportion of cases who had 1 or more people per room was 41.1%, and among controls 48.5%. 82% of the subjects had low income (< 200 Euro/month). Among the controls, 9.1% of the subjects had less than 200 Euro incomes per month.
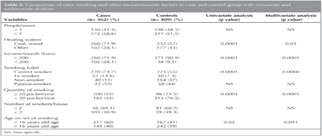
Table 2-3 show the results of univariate and multivariate analysis among the cases and controls. Patients who smoke had a 5 fold (95% CI: 3.2-7.5, p< 0.0001) higher odds of having active tuberculosis compared with patients who do not smoke. Similarly, patients using coal or wood for indoor heating had a 1.6 fold (95% CI: 1.179-2.305, p< 0.003) higher odds having tuberculosis. People who have less income (< 200 Euro/month) had 3.2 fold (95% CI: 2.113-5.106, p< 0.0001) higher odds of having tuberculosis compared with people having high income. There was a significant correlation between heavy smoking (≥ 20 packet/year, p< 0.0001) and age onset of smoking (< 16 years of age, p< 0.041). There was no significant association between environmental tobacco smoke and tuberculosis.
Discussion
In the present study, we have demonstrated that smoking and indoor air pollution increases the risk of tuberculosis. The odds ratio for smoking and indoor air pollution exposure obtained from the study is statistically significant. These findings suggest that there is a strong correlation between the indoor air pollutants such a tobacco and/or the other smokes from the heating systems and tuberculosis risk.
Epidemiological evidences are stronger to show this relationship between indoor air quality and tuberculosis. Klopppan C, et al. examined the estimated crude odds ratio of the association between tobacco smoking and tuberculosis was 2.48 (14). In the Gambhir HS, et al. study patients who smoke had a three fold higher odds of having tuberculosis compared with patients who do not smoke. Also they showed that the odds ratio for sputum positivity for acid fast bacilli among smokers was 4.6 times higher than non-smokers (10). In our study, the odds ratio of the association between tuberculosis and smoking was nearly five. We find higher odds from the other studies. It could be due to exposure of high amounts of tobacco smoke in our population. We used males and the smoking prevalence was 74.6%. Heavy smoking rate and early onset of smoking rate were also higher in our population.
Studies also investigated that exposure to solid fuels for heating or cooking was associated with tuberculosis. Gupta, et al. reported that those who used wood for cooking stoves were 2.5 times more likely to have tuberculosis (15). Mishra, et al. reported that cooking using biomass fuels is significantly associated with tuberculosis (adjusted OR 2.58, 95% CI 1.98-3.37) (16). Wang J, et al. also demonstrated that using solid fuel for cooking (OR 1.08, 95% CI 0.62-1.87) or heating (OR 1.04, 95% CI 0.54-2.02) was significantly associated with tuberculosis. Similarly, we found the same results that patients using coal or wood for indoor heating had a 1.6 fold (95% CI: 1.179-2.305, p< 0.003) higher odds having tuberculosis. In this study, we used male population so we did not examine the effect of using stoves for cooking in women. There could be different results for women which is the limitation of our study.
Epidemiological studies suggest a relationship between tuberculosis and indoor air pollution. However, the underlying mechanisms are not clear. Smoke particle size, form and surface chemistry are all related with the airway inflammation. A limited number of studies have suggested that tumour necrosis factor-alfa (TNF-α), interleukin-6 (IL-6) and IL-8 cytokines, nuclear factor-kB (NF-kB) activation and cellular lipid peroxidation are effective at the proinflammatory state and oxidative damage of the lungs (8). Further experimental studies are needed to clarify the pat hogenesis of tuberculosis on the patients exposed to air pollutants or tobacco smoke.
It is clear that tuberculosis is more prevalent among poor people. Socioeconomic status is an important risk factor for pulmonary tuberculosis mainly in people with a low income using stoves for heating. In this study we have used a monthly income for socioeconomic status. We examined that people who have less income (< 200 Euro/month) had 3.2 fold (95% CI: 2.113-5.106, p< 0.0001) higher odds of having tuberculosis compared with people having high income. Tobacco smoking had the highest risk in this study. Socioeconomic status had an association with tuberculosis, which was higher than the risk associated with using stoves for heating. There is a complex interaction between smoking, socioeconomic conditions, indoor air quality and tuberculosis.
In the conclusion, tuberculosis is a common health problem for our country. Smoking rates are decreasing in the public places by the smoke free laws. However many people are still continue to smoke in their homes. Not only smoking, using stoves for heating or cooking also increasing the level of smokes indoors. We all know that many people spend most of their times indoors. Therefore smoking cessation and to encourage indoor air quality standards could become a part of controlling strategy of tuberculosis epidemic in developing countries.
CONFLICT of INTEREST
None declared.
REFERENCES
- T.C. Sa?l?k Bakanl??? Verem Sava?? Daire Ba?kanl???. T?rkiye'de Verem Sava?? 2010 Raporu. Avaliable at: http://www.ehsm.gov.tr/Sub/verem_savas_dispanseri/files/dokumanlar/turkiyede_verem_savasi_2010_raporu.pdf
- American Thorasic Society Workshop Achieving Healty Indoor Air. Am J Respir Crit Care Med 1997;156(3 Pt 2):S31-64. Avaliable at: http://www.thoracic.org/statements/resources/archive/indoor1-33.pdf
- Bilir N, G??iz B, Y?ld?z AN. Assessing Tobacco Control Strategies in Turkey. Ankara. Hacettepe Public Health Foundation. International Development Research Center, 2003.
- Bilir N, G??iz B, Y?ld?z AN. Smoking Behaviors and Attitudes. Ankara. Hacettepe Public Health Foundation.International Development Research Center, 1997.
- Kan X, Chiang CY, Enarson DA, Chen W, Yang J, Chen G. Indoor solid fuel use and tuberculosis in China: a matched case-control study. BMC Public Health 2011;11:498.
- Gninafon M, Ade G, A?t-Khaled N, Enarson DA, Chiang CY. Exposure to combustion of solid fuel and tuberculosis: a matched case-control study. Eur Respir J 2011;38(1):132-8.
- Kolappan C, Subramani R. Association between biomass fuel and pulmonary tuberculosis: a nested case-control study. Thorax 2009;64:705.
- Gordon S, Rylance J. Where there's smoke... there's tuberculosis. Thorax 2009;64(8):649-50.
- Wang J, Shen H. Review of cigarette smoking and tuberculosis in China: intervention is needed for smoking cessation among tuberculosis patients. BMC Public Health 2009;9:292.
- Gambhir HS, Kaushik RM, Kaushik R, Sindhwani G. Tobacco smoking-associated risk for tuberculosis: a case-control study. Int Health 2010;2(3):216-22.
- L?nnroth K, Jaramillo E, Williams B, Dye C, Raviglione M. In: Blas E, Sivasankara Kurup A (eds). Equity, social determinants and public health programmes. Geneva: World Health Organization; Tuberculosis: the role of risk factors and social determinants 2010;12:219-241.
- US Centers for Disease Control and Prevention (2010). Health behaviors of adults: United States, 2005-2007. Vital and Health Statistics, Series 10, Number 245, Appendix II, p. 80.
- Nondahl DM, Cruickshanks KJ, Schubert CR. A questionnaire for assessing environmental tobacco smoke exposure. Environmental Research 2005;97:76-82.
- Kolappan C, Gopi PG. Tobacco smoking and pulmonary tuberculosis. Thorax 2002;57(11):964-6.
- Gupta BN, Mathur N, Mahendra PN, Srivastava AK, Swaroop V, Agnihotri MS. A study of household environmental risk factors pertaining to respiratory diseases. Energy Environment Monitor 1997;1(3):61?7.
- Mishra VK, Retherford RD, Smith KR. Biomass cooking fuels and prevalence of tuberculosis in India. Int J Infect Dis 1999;3(3):119-29.
Yaz??ma Adresi (Address for Correspondence)
Dr. Ay?e Bilge ?zt?rk
Medeniyet ?niversitesi, G?ztepe E?itim ve
Ara?t?rma Hastanesi,
Eri?kin Allerji ?nitesi,
Kad?k?y, ?STANBUL - TURKEY
e-mail: aysebilgeozturk@yahoo.com