Ya?l? hastada k???k pn?motoraks?n giri?imsel olmayan tedavisi
Katsunori KAGOHASHI1, Gen OHARA1, Koichi KURISHIMA1, Hiroaki SATOH1
1 Tsukuba ?niversitesi Mito T?p Merkezi, Solunum Hastal?klar? Anabilim Dal?, Ibaraki.
?ZET
Ya?l? hastada k???k pn?motoraks?n giri?imsel olmayan tedavisi
Ya?l? hastada k???k pn?motoraks?n giri?imsel olmayan tedavisi olduk?a nadir bildirilmi?tir. Toraks bilgisayarl? tomografide %20'nin alt?ndaki k???k pn?motorakslar?n giri?imsel olmayan ba?ar?l? tedavisi 3 hastada g?sterilmektedir. Akci?er grafisi ve dikkatli kardiyopulmoner monit?rizasyon ile k???k pn?motorakslarda giri?imsel olmayan tedavi ya?l? hastalarda bir se?enek olabilir.
Anahtar Kelimeler: Pn?motoraks, ya?l?
SUMMARY
Non-interventional management of small pneumothorax in the very elderly
Katsunori KAGOHASHI1, Gen OHARA1, Koichi KURISHIMA1, Hiroaki SATOH1
1 Department of Internal Medicine, Mito Medical Center, Tsukuba University, Ibaraki, Japan.
2 Division of Respiratory Medicine, Faculty of Medicine, Tsukuba University, Ibaraki, Japan.
The non-interventional management (NIM) of elderly patients with small pneumothorax has rarely reported. We show herein three elderly cases of successful treated with NIM for small pneumothorax (< 20% on chest computerized tomography scan). With adequate evaluation of chest radiographs and careful cardiopulmonary monitoring, we evaluated that NIM for small pneumothorax can be a possible therapeutic choice even in the elderly.
Key Words: Pnuemothorax; elderly.
Tuberk Toraks 2013; 61(4): 342-345 • doi:10.5578/tt.6585
Geli? Tarihi/Received: 01/11/2013 • Kabul Edili? Tarihi/Accepted: 17/11/2013
Introduction
Pneumothorax is common and potentially life-threatening (1,2). However, not every pneumothorax needs surgical intervention or thoracic tube drainage. Non-interventional management (NIM) of small pneumothorax (< 2 cm rim present between the lung edge and chest wall) may perform in selected groups of patients with stable cardiopulmonary condition (1,2,3). In the very elderly, however, NIM for small pneumothorax has not been well evaluated. We herein report successfully treated three elderly pneumothorax cases with NIM.
Case reports
Case 1
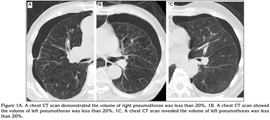
An 84-year-old man with chronic obstructive pulmonary disease (COPD) presented with dyspnea on exertion five days before visit to our hospital. He had a 35 pack-year smoking history. A plain chest radiograph demonstrated a curvilinear opacity adjacent to the left lateral chest wall. This appearance was suggestive of a small pneumothorax (< 2 cm rim present between the lung edge and chest wall). A chest computerized tomography (CT) scan demonstrated the volume of the pneumothorax was less than 20% (Figure 1A). Therefore, a chest drain was not inserted, with enough security in cardiopulmonary monitoring for a week. Over a period of three weeks, the pneumothorax resolved.
Case 2
An 81-year-old man with COPD presented with breathlessness on exertion two days before visit to our hospital. He had smoked 20 pack/years. A plain chest radiograph demonstrated a small pneumothorax. Arterial blood gas analysis revealed that PaO2 was 103.6 torr, PaCO2 49.7 torr, and pH 7.345 with 2 L/min oxygen. A chest CT scan showed the volume of the pneumothorax was less than 20% (Figure 1B). Without insertion of chest tube, he had enough security in cardiopulmonary monitoring for a week. Over a period of 10 days, the pneumothorax resolved.
Case 3
A 91-year-old man with COPD referred with dyspnea on exertion 6 days before visit to our hospital. He had an 80 pack/year and had medical history of left pneumothorax three times, which were treated with NIM. A plain chest radiograph demonstrated a curvilinear opacity adjacent to the left lateral chest wall. This appearance was suggestive of a small pneumothorax. A chest CT scan confirmed the volume of the pneumothorax was less than 20% (Figure 1C). With no chest tube insertion, cardiopulmonary monitoring was continued for a week. Over a period of two weeks, the pneumothorax disappeared.
Discussion
Pneumothorax is a potentially life-threatening condition. Traditionally, thoracic tube drainage or surgical intervention for majority patients is recommended; however, selected cases of small pneumothorax being successfully treated by NIM have been reported (1,2,3,4). In a recent review, Currie et al. reported that patients with a small pneumothorax (< 2 cm rim present between the lung edge and chest wall) with few symptoms did not require active intervention (2). While younger patients can be treated easily, however, the elderly may require special care because of their coexisting pulmonary or non-pulmonary diseases. It has been generally accepted that the management of a pneumothorax depends on the severity of symptoms, its size, and presence of underlying lung disease (1,2). Chest radiographs are notoriously poor at assessing the volume of pneumothorax, although recent guidelines published by the British Thoracic Society suggest that the size of a pneumothorax should be categorized according to the amount of air visible between the lung edge and chest wall (1). Additionally, we previously reported the importance of chest CT scan on pneumothorax in the elderly with anterior pneumothorax, which was not large pneumothorax on plain chest radiograph (5). Therefore, we suggested that the evaluation of pneumothorax on chest CT is essential and we treated above-mentioned three patients. In our case 1, the patient's condition was stable and he showed a good tolerance of small pneumothorax without thoracic tube drainage at the time of diagnosis. Therefore, NIM was continued and resulted in a good outcome. In case 2, although an early diagnosis of pneumothorax was made, NIM was selected, first because no severe hypoxia and second, after our experience with case 1, we thought that we would be able to manage the small pneumothorax conservatively. Case 3 was a non-agenarian with a medical history of left pneumothoraces. Taking into his poor general and cardiopulmonary condition, surgical treatment was not selected.
On the basis of the BTS guideline and our experience, we propose patient selection criteria for indicating NIM for pneumothorax in the elderly as follows; (a) Patients who are in a clinically stable condition at the time of presentation and remain so; (b) Pneumothorax smaller than 20% on chest CT scan; (c) Enough security in cardiopulmonary monitoring; (d) Treatment team which can cope with surgery treatment.
Our cases did meet these criteria, and they were successfully treated with NIM without continuous intrathoracic drainage. When cardiopulmonary condition deteriorates with increasing pneumothorax, the size of the pneumothorax turns larger than 20%, and dyspnea or chest pain fail to improve within 24 hour under NIM, surgical intervention should be considered without further delay.
It is difficult to compare mortality rates after surgical treatment with those after NIM for pneumothorax, because each case has different general conditions and surgical therapy is likely to be performed in very severe cases. A major problem of NIM is that a longer hospital stay may be required than for successful surgical therapy. Our three patients were discharged within three weeks, whereas successful surgical treatment usually requires a hospital admission of less than two weeks. However, the frequency of complications after surgery, such as leakage, and stricture seems to be relatively high in elderly pneumothorax patients coexisting with pulmonary emphysema or interstitial pneumonia (6,7). In these complicated patients, the hospital stay usually may be as long as that for conservative therapy. Furthermore, the thoracic tube drainage or surgical treatment is more expensive than conservative therapy (8). Thus, considering the mental as well as physical agony of surgery, NIM is likely to be considered, and can be appropriate if careful evaluation of the associated disease can be made, to avoid further invasive procedures or medication.
In summary, three elderly cases of small pneumothorax were successfully treated by NIM. With the development of imaging techniques such as CT scan, as well as improved cardiopulmonary monitoring, NIM for small pneumothorax can be a possible therapeutic choice even in the elderly. As NIM is likely to fail in the presence of additional medical complications, the cardiopulmonary condition should be examined carefully when NIM is carried out. When NIM fails to show any improvement, interventional therapy should be initiated without further delay.
CONFLICT of INTEREST
None declared.
REFERENCES
- Henry M, Arnold T, Harvey J. BTS guidelines for the management of spontaneous pneumothorax. Thorax 2003; 58(Suppl II): ii39?ii52.
- Currie GP, Alluri R, Christie GL, Legge JS. Pneumothorax: an update. Postgrad Med J 2007; 83: 461-5.
- Tschopp JM, Rami-Porta R, Noppen M, Astoul P. Management of spontaneous pneumothorax: state of the art. Eur Respir J 2006; 28: 637-50.
- Weissberg D, Refaely Y. Pneumothorax: experience with 1199 patients. Chest 2000; 117: 1279-85.
- Kikuchi N, Satoh H, Ohtsuka M, Sekizawa K. Anterior pneumothorax. J Emerg Med 2005; 29: 485-6.
- Videm V, Pillgram-Larsen J, Ellingsen O, Andersen G, Ovrum E. Spontaneous pneumothorax in chronic obstructive pulmonary disease: complications, treatment and recurrences. Eur J Respir Dis 1987; 71: 365-71.
- Picado C, G?mez de Almeida R, Xaubet A, Montserrat J, Letang E, S?nchez-Lloret J. Spontaneous pneumothorax in cryptogenic fibrosing alveolitis. Respiration 1985; 48: 77-80.
- Schramel FM, Sutedja TG, Braber JC, van Mourik JC, Postmus PE. Cost-effectiveness of video-assisted thoracoscopic surgery versus conservative treatment for first time or recurrent spontaneous pneumothorax. Eur Respir J 1996; 9: 1821-5.
Yaz??ma Adresi (Address for Correspondence):
Dr. Hiroaki SATOH,
Tsukuba ?niversitesi Mito T?p Merkezi,
?? Hastal?klar? Anabilim Dal?,
Miya-machi 3-2-7, Mito, 310-0015, Ibaraki - Japan
e-mail: hirosato@md.tsukuba.ac.jp