?nterstisyel akci?er hastal?klar?nda pulmoner rehabilitasyon
Dicle KAYMAZ1, P?nar ERG?N2, ?pek CANDEM?R2, Ezgi UTKU2, Ne?e DEM?R2,
Fatma ?ENG?L2, Nurcan EGESEL2, Pervin DEM?R3
1 Ankara Atat?rk G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, Pulmoner Rehabilitasyon
ve Evde Sa?l?k Hizmet Sunum Merkezi, Ankara,
2 Atat?rk G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, G???s Hastal?klar? Klini?i, Ankara
3 Y?ld?r?m Beyaz?t ?niversitesi T?p Fak?ltesi, Biyoistatistik Anabilim Dal?, Ankara
?ZET
?nterstisyel akci?er hastal?klar?nda pulmoner rehabilitasyon
Giri?: ?nterstisyel akci?er hastal?klar?, egzersiz dispnesi, egzersiz intolerans?, kuru ?ks?r?k ve ya?am kalitesinde bozulma ile karakterizedir. Bu ?al??mada ama?, pulmoner rehabilitasyonun interstisyel akci?er hastal?klar? ?zerine olan etkisini de?erlendirmektir.
Materyal ve Metod: ?nterstisyel akci?er hastal?klar? tan?s? olan ve merkezimize y?nlendirilen ayaktan takip edilen 10 hasta, 8 hafta yo?un pulmoner rehabilitasyon program?na al?nd?. Olgular?n; dispne alg?s? Medical Research Council ile, ya?am kaliteleri St. George Solunum Anketi (SGRQ) ile, v?cut kompozisyonlar? biyoelektriksel impedans y?ntemiyle, egzersiz kapasiteleri artan h?zda mekik y?r?me testi (AHMYT) ve endurans mekik y?r?me testi (EMYT) ile, anksiyete ve depresyonlar? ise hastane anksiyete depresyon skalas? (HADS) ile de?erlendirildi. ?al??maya al?nan hastalar?n pulmoner rehabilitasyon program? ?ncesi ve sonras? parametreleri kaydedildi.
Bulgular: Pulmoner rehabilitasyon program? sonras? olgular?n dispne alg?lar?nda (p: 0.023), anksiyete ve depresyon skorlar?nda iyile?me mevcuttu. (p: 0.026, p: 0.039). SGRQ'nun alt ba?l?I?? olan etki skorunda da istatistiksel anlaml? iyile?me saptand? (Z= 1.988; p= 0.047). Pulmoner rehabilitasyon sonras? AHMYT ortancas?nda 60 metre art?? saptanmas?na ra?men bu art?? istatistiksel anlaml?l??a ula?mad? (Z= 1.863; p= 0.063). Fakat bu art?? AHMYT i?in hesaplanan minimal klinik anlaml?l?k d?zeyinden daha fazlayd?.
Sonu?: ?al??mam?zdaki sonu?lar da kuvvetle g?steriyor ki pulmoner rehabilitasyonun interstisyel akci?er hastal?klar?n?n tedavisinde standart tedavi yakla??m? olmal?d?r ve olgular?n y?netiminde pulmoner rehabilitasyonun tan? a?amas?ndan itibaren mutlaka yer almal?d?r.
Anahtar Kelimeler: Pulmoner rehabilitasyon; interstisyel akci?er hastal?klar?; egzersiz kapasitesi.
SUMMARY
Pulmonary rehabilitation in interstitial lung diseases
Dicle KAYMAZ1, P?nar ERG?N2, ?pek CANDEM?R2, Ezgi UTKU2, Ne?e DEM?R2,
Fatma ?ENG?L2, Nurcan EGESEL2, Pervin DEM?R3
1 Ankara Ataturk Chest Diseases and Chest Surgery Training and Research Hospital, Pulmonary Rehabilitation
and Home Care Center, Ankara, Turkey,
2 Department of Chest Diseases, Ankara Ataturk Chest Diseases and Chest Surgery Training and
Research Hospital, Ankara, Turkey,
3 Department of Biostatistics, Faculty of Medicine, Yildirim Beyazit University, Ankara, Turkey.
Introduction: Interstitial lung diseases are characterised by dyspnea on exertion, low quality of life, cough and exercise intolerance. The aim of this study was to evaluate the effects of comprehensive pulmonary rehabilitation in patients with interstitial lung disease.
Materials and Methods: Data from patients who were referred to pulmonary rehabilitation? with the diagnosis of interstitial lung diseases were included to this study. Ten patients with interstitial lung disease participated to our outpatient, 8 weeks, comprehensive pulmonary rehabilitation programme. Dyspnea was assessed with the Medical Research Council (MRC) scale; health related quality of life was assessed with the St.George's Respiratory Questionnaire (SGRQ). Exercise capacity was measured using the incremental shuttle walk test (ISWT) and endurance? shuttle walk test (ESWT); anxiety and depression were assessed with the hospital anxiety depression scale (HADS).? All parameters were recorded before and after pulmonary rehabilitation programme.
Results: Dyspnea sensation, anxiety and depression? scores decreased after pulmonary rehabilitation? (p: 0.023, p: 0.026, p: 0.039 respectively). Also impact domains of SGRQ? significantly reduced (Z= 1.988; p= 0.047).The difference between median values of ISWT results before and after pulmonary rehabilitation was 60 meters. Although it was not statistically significant (Z= 1.863; p= 0.063), the level of increment was higher than the minimaly important clinical differance for ISWT.
Conclusion: Our results showed that comprehensive pulmonary rehabilitation programmes were benefical for patients with interstitial lung diseases and it should be regarded as a standard care in this population from the early stages
Key Words: Pulmonary rehabilitation, interstitial lung diseases, exercise capacity.
Tuberk Toraks 2013; 61(4): 295-302 • doi:10.5578/tt.6291
Geli? Tarihi/Received: 31/05/2013 • Kabul Edili? Tarihi/Accepted: 24/10/2013
INTRODUCTION
Interstitial lung diseases (ILDs) is a heterogeneous group of diseases such as idiopathic pulmonary fibrosis (IPF), acute and chronic interstitial pneumonia, connective tissue diseases, and sarcoidosis, which are largely a reason of inability (1,2,3). Patients with ILD frequently present with exertional dyspnea, dry cough, poor exercise capacity, low quality of life, decreased psycho-social status and impaired body composition. As it was shown in several studies, pulmonary rehabilitation is likely to improve these factors (4,5).
Indications for pulmonary rehabilitation patients with chronic obstructive pulmonary disease (COPD) have been well-known and well identified compared to those for ILD, and has lead to an increased referral of COPD patients to pulmonary rehabilitation programmes. In a review by Crouch et al. it was suggested that functional improvements of non-COPD patients in pulmonary rehabilitation programmes are similar those obtained in COPD patients (4). Foster et al. studied a heterogeneous group of 32 patients with non-COPD including ILD, bronchiectasis, fibrothorax, thoracoplasty, and neuromuscular abnormalities and noted that improvement with rehabilitation was only slightly less than that of COPD patients (6). In American College of Chest Physicians/American Association of Cardiovascular Pulmonary Rehabilitation (ACCP/AACVPR) guidelines, pulmonary rehabilitation in non-COPD patients is an effective and proven strategy of management with an evidence level of 1B (7).
Despite an increasing level of knowledge regarding the effectiveness of pulmonary rehabilitation in patients with ILD, characteristics which determine the success of pulmonary rehabilitation in ILD has not been identified clearly. In this study it was aimed to evaluate the effects of comprehensive pulmonary rehabilitation on dyspnea perception, exercise capacity, quality of life, body composition in patients with ILD.
MATERIALS and METHODS
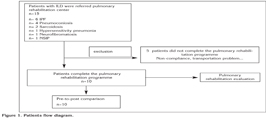
Fifteen patients who were referred to Ataturk Chest Diseases and Chest Surgery Training and Research Hospital Pulmonary Rehabilitation and Home Care Center with the diagnosis of ILD between 2006-2009 were included this study. The institutional ethics committee approved this study. A written informed consent was obtained from each patient before all the procedures. We obtained an approval from the administration of our institution to use patients' records and all the patients' confidentiality was maintained. Our study was retrospective, we used our institution's database so, we did not obtain ethics committee approval. Twelve (80.0%) patients were male and 3 (20.0%) patients were female. The mean age of these patients was 50.06 ? 16.47 years. Median value of cigaratte smoking was 5 [Interquartile Range (IQR)= 43] pack/years (mean 19.20 ? 21.52).
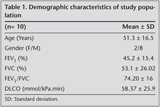
Six patients were diagnosed as IPF, four patients had pneumoconiosis (coal worker pneumoconiosis, silicosis, hemosiderosis, dental technician pneumoconiosis), two had sarcoidosis, one had neurofibromatosis, one had hypersensitivity pneumonia and last patient had non-specific interstitial pneumonia (NSIP). Five patients did not complete the pulmonary rehabilitation programme due to not being able to obtain permission from their work, transportation problems, and noncompliance to the pulmonary rehabilitation programme. Demographic characteristics of 10 patients who completed the pulmonary rehabilitation programme are given in Table 1. Patients diagram is shown as a flow diagram in Figure 1.
Patients underwent an 8-week hospital based outpatient comprehensive pulmonary rehabilitation and attended the rehabilitation unit on two half-days per week. Pulmonary rehabilitation programme consisting of: (a) educational support, covering the following topics: disease education and education of families, bronchial hygiene and breathing control techniques, energy conservation, relaxation. Each educational programme was 45 minutes long and repeated every month, (b) exercise training, (c) psychological counselling, (d) a nutritional intervention, if needed. Educational sessions were delivered by two chest physicians, two physical therapists, a dietician, two respiratory nurses and a psychologist.
Before and after the pulmonary rehabilitation programme dyspnea perceptions during the activities of daily living was assessed with Medical Research Council (MRC) scale, exercise capacity with Incremental Shuttle Walk Test (ISWT) and Endurance Shuttle Walk Test (ESWT), health related quality of life with a Turkish version of St. George Respiratory Questionnaire (SGRQ) that was previously to Turkish with a permission from Dr. Paul Jones. The body composition with bioelectrical impedance method and their psychological evaluation assessed with Turkish version of Hospital Anxiety Depression Scale (HADS). Since 1997, Turkish version of HADS is validated and found reliable in medically ill patients.
Exercise Programme
The exercise training programme was completely tailored to suit the needs of individual. In each patient, aerobic exercise and strength training for the upper and lower extremities were performed. Exercise training was carried out according to criteria as follows: minimum eight week period, three days a week (two days of which were in hospital under supervision and one day of which was without supervision). Aerobic exercise included cycle ergometer training (15 minutes/day), treadmill training (15 minutes/day), upper and lower extremity strength training (5-10 minutes/day). Patients were trained at 50% of peak workload and 60-85% of peak VO2. Exercises intensity was increased according to the patient progress. In four patients with severe dyspnea, muscle weakness, and serious pulmonary hypertension, neuromuscular electrical stimulation (NMES) and strength exercise had been applied in specific muscle groups (quadriceps and deltoid) in upper and lower extremities NMES, in symmetric biphasic wave form, was applied for 15 minutes in 300-400 ?s, 50 Hz at stimulation frequency during period, the intensity was increased to the level where contraction could be obtained and which the patient could tolerate.
Statistical Analysis
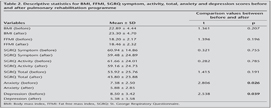
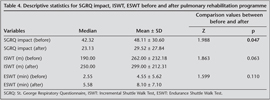
Unlike conventional methods, normally distributed variables (n< 30) was assessed with graphical and Shapiro-Wilks test. Descriptive statistics for the normally distributed variables [age, BMI, fat free mass index (FFMI), SGRQ symptom, activity and total, anxiety and depression scores] were given as mean ? standard deviation that is shown for each variable in Table 2. Descriptive statistics for variables which did not distribute normally (SGRQ impact, meters, endurance time and cigarette (pack/years) were given as median values. Categorical variables such as MRC and gender was given as percentage and number.
Student t-test was performed to compare normally distributed variables before and after pulmonary rehabilitation programme. Wilcoxon signed rank test was performed to compare variables that did not distribute normally. Statistical analyses were performed using MS-Excel 2007 and SPSS for Windows Version 15.0 (SPSS Inc., Chicago, ILL, USA). Statistical significance was determined by p< 0.05.
RESULTS
The mean age of patients included in the study was 51.30 ? 16.55 years. In patients with ILD, diffusion capacity for carbon monoxide (DLCO) was also found to be decreased at rest (mean DLCO was 58.37 ? 25.97 % mmol/kPa.min). Two out of 10 patients did not show any compliance to the diffusion test. As shown in Table 1, patients had consistent mild restrictive defect in respiratory function test. Five out of 10 patients had also been using long term oxygen therapy at home.
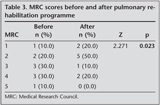
Grade 5 MRC dyspnea score was observed in only one patient (10%). Grade 4 was seen in 3 patients (30%), and 3 patients had grade 3 (30%). After pulmonary rehabilitation improvements in dyspnea sensation reached statistically significant level (Z= 2.271; p= 0.023). Before and after pulmonary rehabilitation MRC scores of patients who completed the study protocol was shown in Table 3.
Before the pulmonary rehabilitation programme, the mean distance walked in ISWT was 262.00 ? 232.18 m, whereas it was 299.00 ? 212.31 m at the end of the pulmonary rehabilitation. The difference between median values before and after pulmonary rehabilitation was 60 meters. Though, it was not statistically significant (Z= 1.863; p= 0.063), the level of increment in walking distance was higher than the minimally important clinical difference for ISWT. In ESWT patients walked 4.55 ? 5.62 (mean) minutes before and 8.10 ? 7.10 (mean) minutes after the PR programme. The improvements in endurance time did not also reveal any statistical significance (Z=1.599; p= 0.110).
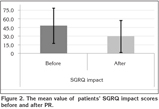
Health related quality of life before and after pulmonary rehabilitation programme were assessed by SGRQ which is composed of 3 domains (symptom, anxiety, impact) (Table 4). There were statistically significant improvements in SGRQ's impact score (Z= 1.988; p= 0.047). While the mean value of impact score before pulmonary rehabilitation was 48.11 ? 30.60, it was found 29.52 ? 27.84 after pulmonary rehabilitation (Figure 2). Statistically significant improvements were not observed in symptom, activity and total score (p= 0.755, 0.785 and 0.191, respectively).
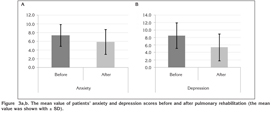
Anxiety and depression are the most important psychosocial problems that could frequently be observed in ILD. It was also evaluated in our study by using HADS, consisting of 14 items. Anxiety and depression scores after pulmonary rehabilitation showed statistically significant improvements (t= 2.806; p= 0.026 and t= 2.538; p= 0.039, respectively) (Figure 3a,b).
No statistically significant difference was observed in body mass index (BMI) and fat free mass index (FFMI), (t= 1.361; p= 0.207 and t= 1.396; p= 0.196, respectively).
DISCUSSION
Pulmonary rehabilitation has been defined as a ?multidisciplinary programme' of the care of patients with chronic respiratory impairment which is individually tailored and designed to optimize physical and social performance and autonomy (4,5). American Thoracic Society/European Respiratory Society Consensus Statement on pulmonary rehabilitation supports the use of pulmonary rehabilitation in the management of chronic respiratory disease regardless of cause. The data supporting its use was derived extensively from the studies of COPD, in which pulmonary rehabilitation has been shown to increase exercise endurance, decrease dyspnea, improve health related quality of life, and reduce health care costs. Increased perception of dyspnea was one of the most important reason for pulmonary rehabilitation programme in ILD. It is known that dyspnea perception could be very different among individuals who are even at the same level of ILD, and this difference increases with the progression of the underlying disease. In two different studies in which the effect of pulmonary rehabilitation in dyspnea perception in ILD had been analyzed, the authors reported significant improvements in MRC and dyspnea domain of chronic respiratory diseases questionnaire (8,9). In our study, like the other two studies, dyspnea perception was found to be improved significantly after an individually-supervised, eight-week pulmonary rehabilitation programme.
The reduction in exercise capacity in ILD mostly occurs through different mechanisms which are closely related to each other. Although ventilatory and circulatory pathologies are the major determining factors for exercise restriction in ILD, the systemic manifestations of the underlying disease or peripheral and/or respiratory muscle dysfunction secondary deconditioning related to immobility are responsible for decrease in exercise capacity (10). In association with these facts, the study by Nishiyama et al. showed that quadriceps muscle strength significantly diminished in 41 patients diagnosed with IPF. They also found that peripheral muscle weakness was a determining factor for decreased exercise capacity (11). The results of this study indicate that peripheral muscle training is necessary for the patients with ILD. In our study, aerobic exercise and strength training were performed in six patients. Neuromuscular electrical stimulation (NMES) and strength training was applied to upper and lower extremities of four patients who could not carry out to endurance training due to severe dyspnea, muscle weakness and serious pulmonary hypertension. Increase in ISWT after pulmonary rehabilitation programme supports the suggestion that those patients also need exercise training programmes containing endurance and strength on peripheral muscles similar to those with COPD. Ferreira et al. also showed that ILD patients who had low 6MWT distance, had significant increase in mean distance after pulmonary rehabilitation programme (12). In the study by Naji et al, which was similar to ours, the exercise capacity was evaluated with ISWT, and a 61 m-increase was observed after pulmonary rehabilitation programme (9). In our study, an increase in ISWT was not found to be statistically significant. This problem may be solved by increasing the number of patients in the study. This finding might be associated with the fact that, exercise capacity of our patients were better in our study. However, Singh et al reported that minimal clinically important difference (MCID) for ISWT at group level should be 48 m for COPD patients (13). Although reference values for ISWT in ILD have not been standardized yet, improvements in exercise capacity were close to change in MCID levels in patients with COPD in our study.
As a result of the fact that most ILD have a characteristic rapid progression, deterioration in the quality of life of patients is an expected result. It was known that the major factors which affect the quality of life in patients with IPF were fatigue, immobility, disabilities during daily living, and working. Different questionnaires have been used in various studies to evaluate the quality of life in ILD. SGRQ was used in our study, and a statistically significant improvement was observed in SGRQ's impact score at the end of the pulmonary rehabilitation programme. In their study with 31 patients with ILD, Jastrezbski et al. reported a significant improvement in SGRQ impact, activity and total scores at the end of this pulmonary rehabilitation programme. Similar to our study, they observed no significant difference in SGRQ symptom scores which might be explained by the presence of questions specifically designed for COPD symptoms such as; cough, expectoration, whistling rales and breathlessness attacks, all of which could not be typically expected in pulmonary fibrosis (14). In another study, it was also indicated that World Health Organization Quality of Life questionnaire (WHOQOL-100) was a more suitable questionnaire in ILD patients than SGRQ (3).
In their study which covered 57 patients with ILD, Holland et al. stated that there was an increase in the quality of life at the end of an 8-week-pulmonary rehabilitation programme, but there was no difference compared with the control group after six months (8). It was also shown in our study that pulmonary rehabilitation programmes produced benefit in health related quality of life in patients with ILD. Psychological benefits of pulmonary rehabilitation can be accepted as gaining in the power to cope with the illness, an increase in sense of control and as a result of all, a fall in anxiety and depression levels. Statistically significant decrease in anxiety and depression scores after the pulmonary rehabilitation programme in our study underlines the importance of comprehensive pulmonary rehabilitation programmes in ILD. Another study reported a statistical improvement in the Center for Epidemiologic Studies-Depression (CES-D) score of twenty seven patients with ILD at the end of a pulmonary rehabilitation programme, which unfortunately did not lead to clinical improvement (12).
CONCLUSION
Our study has shown that a comprehensive, hospital-based outpatient pulmonary rehabilitation programme provided improvement in dyspnea perception, exercise capacity, health associated quality of life, anxiety, and depression in patients with ILD. Under the support of above findings, it could be rationally suggested that a comprehensive, multidisciplinary, individually pulmonary rehabilitation programme should become a part of the standard care in patients with ILD. Patients may be referred to pulmonary rehabilitation programmes immediately after the diagnosis commenced without any delay. Nevertheless, encouraging results consistent with many previous studies warrant larger randomized and multicenter trials to evaluate whether a comprehensive, hospital-based outpatient pulmonary rehabilitation programme improves clinical outcome in patients with ILD at long-term.
CONFLICT of INTEREST
None declared.
REFERENCES
- An Official ATS/ERS/JRS/ALAT Statement. Idiopathic Pulmonary Fibrosis: Evidence-based Guidelines for Diagnosis and Management. Am J Respir Crit Care Med 2011; 183: 788-24.
- Crouch R, MacIntyre NR. Pulmonary rehabilitation of the patient with non-obstructive lung disease. Respir Care Clin N Am 1998; 4: 59-70.
- De Vries J, Seebregts A, Drent M. Assessing health status and quality of life in idiopathic pulmonary fibrosis. Which measure should be used. Respir Med 2000; 94: 273-8.
- Disease-specific approaches in pulmonary rehabilitation In; American Association of Cardiovascular and Pulmonary Rehabilitation's (AACVPR's) Guidelines for Pulmonary Rehabilitation Programs 3rd ed 2004: 73-5.
- Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. American Thoracic Society/European Respiratory Society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 2006; 173: 1390-413.
- Foster S, Thomas HM 3rd. Pulmonary rehabilitation in lung disease other than chronic obstructive pulmonary disease. Am Rev Respir Dis 1990; 141: 601-4.
- Pulmonary Rehabilitation: Joint ACCP/AACVPR Evidence-Based Clinical Practice Guidelines Chest 2007; 131(Suppl 5): 4S-42S.
- Holland AE, Hill CJ, Conron M, Munro P, McDonald CF. Short term improvement in exercise capacity and symptoms following exercise training in interstitial lung disease.Thorax 2008; 63: 549-54.
- Naji NA, Connor MC, Donnelly SC, McDonnell TJ. Effectiveness of pulmonary rehabilitation in restrictive lung disease. J Cardiopulm Rehab 2006; 26: 237-43.
- Holland AE, Hill C. Physical training for interstitial lung disease. Cochrane Database of Systematic Reviews Issue 4. Art. No. CD006322. 2008.
- Nishiyama O, Taniguchi H, Kondoh Y, Kimura T, Ogawa T, Watanabe F, et al. Quadriceps weakness is related to exercise capacity in idiopathic pulmonary fibrosis. Chest 2005; 127: 2028-33.
- Ferreira A, Garvey C, Connors GL, Hilling L, Rigler J, Farrell S, et al. Pulmonary rehabilitation in interstitial lung disease: Benefits and predictors of response. Chest 2009; 135: 442-7.
- Singh SJ, Jones PW, Ewans R, et al. Minimum clinically important improvement for the incremental shuttle walking test. Thorax 2008; 63: 775-7.
- Jastrzebski D, Gumola A, Gawlik R, Kozielski J. Dyspnea and qual?ty of life in patients with pulmonary fibrosis after six weeks of respiratory rehabilitation. J Phys and Pharma 2006; 57(Suppl 4): 139-48.
Yaz??ma Adresi (Address for Correspondence):
Dr. Dicle KAYMAZ,
Ankara Atat?rk G???s Hastal?klar? ve
G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi,
Pulmoner Rehabilitasyon ve
Evde Sa?l?k Hizmet Sunum Merkezi,
ANKARA - TURKEY
e-mail: dicleyilmaz@hotmail.com