Ast?m ve KOAH tedavisinde kullan?lan inhaler cihazlar hakk?nda
hekimlerin bilgi d?zeyleri ve g?r??leri: INTEDA-1 ?al??mas?
A. Zafer ?ALI?KANER1, Can ?ZT?RK2, Emel CEYLAN3, Sevgi PEKCAN4, ?zge YILMAZ5, Sami ?ZT?RK6,
Cenk CAN7, Osman ?ENER8, ?lk? YILMAZ TURAY9, Nihal KO?10, Ramazan ERSOY11
1 Necmettin Erbakan ?niversitesi Meram T?p Fak?ltesi, ?? Hastal?klar? Anabilim Dal?, Allerji ve
?mm?noloji Bilim Dal?, Konya,
2 Gazi ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara,
3 Adnan Menderes ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ayd?n,
4 Necmettin Erbakan ?niversitesi Meram T?p Fak?ltesi, Pediatrik G???sHastal?klar? Bilim Dal?, Konya,
5 Celal Bayar ?niversitesi T?p Fak?ltesi, Pediatrik Allerji ve G???sHastal?klar? Bilim Dal?, Manisa,
6 G?lhane Askeri T?p Akademisi, Haydarpa?a E?itim Hastanesi, Eri?kin Allerji ve ?mm?noloji Servisi, ?stanbul,
7 Ege ?niversitesi T?p Fak?ltesi, Farmakoloji ve Klinik Farmakoloji Anabilim Dal?, ?zmir,
8 G?lhane Askeri T?p Akademisi, ?mm?noloji ve Allerji Hastal?klar? Bilim Dal?, Ankara,
9 Atat?rk G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, G???s Hastal?klar? Klini?i, Ankara,
10 ?stanbul ?niversitesi Cerrahpa?a T?p Fak?ltesi, Fizyoloji ve Klinik Fizyoloji Anabilim Dal?, ?stanbul,
11 Yedikule G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, Eri?kin Allerji Hastal?klar? Klini?i,
?stanbul.
?ZET
Ast?m ve KOAH tedavisinde kullan?lan inhaler cihazlar hakk?nda hekimlerin bilgi d?zeyleri ve g?r??leri: INTEDA-1 ?al??mas?
Giri?: Bu yaz?da, hekimlerin inhaler tedavi konusundaki bilgi d?zeyleri ve g?nl?k pratiklerini g?z ?n?nde bulundurarak bu tedavilerle ilgili olas? problemlerin de?erlendirilmesi ve tart???lmas? ama?land?.
Materyal ve Metod: Bu ?al??ma, T?rkiye Solunum Ara?t?rmalar? Derne?i (TUSAD) ?nhalasyon Tedavileri ?al??ma Grubu (INTEDA) taraf?ndan ?ubat 2010-?ubat 2011 tarihleri aras?nda 10 ayr? merkezin kat?l?m?yla y?r?t?len prospektif, kesitsel bir anket ?al??mas?d?r. Bu ?al??mada, ?lkemizde ?al??man?n yap?ld??? d?nemde piyasada bulunan yedi ayr? cihaz de?erlendirildi. Aktif olarak solunum yolu hastalar?yla ilgilenen 684 hekimin g?nl?k pratikte kar??la?t?klar? sorunlar ya da hastalar? ile ilgili g?r??leri anket yoluyla elde edildi.
Bulgular: ?o?unlu?unu g???s hastal?klar? uzmanlar? (%37.5) ve pediatristlerin (%38.1) olu?turdu?u kat?l?mc?lar ortalama 11.6 ? 7.9 y?ld?r hekimlik yap?yordu. Hekimlerin inhalasyon cihazlar? ve uygulama teknikleri konusunda bilgi kayna?? ba?l?ca internet ve ila? bro??rleri olarak bildirilmi?ti. Kat?l?mc?lar?n yaln?zca %18.5'i inhaler cihazlarla ilgili bilgilerini yeterli buluyordu ve uygulama tekniklerini yeterince biliyordu. Kat?l?mc?lar?n ?o?unlu?u ila? uygulamas? konusunda hastalar?na kendilerinin bilgi verdi?ini ve bu e?itimin s?kl?kla s?zl? talimatlar ?eklinde oldu?unu bildirdiler. Hekimler, hastalar?n yakla??k %60'?n?n ilac?n? do?ru kulland???n? d???n?yorken, %40.7'sinin tedavi sonu?lar?n? olumsuz olarak etkileyebilecek kritik hatalar yapt???na inan?yordu. Hekimlerin inhaler cihaz se?iminde g?z ?n?nde bulundurdu?u en ?nemli kriterler, fiziksel yeterlili?i, cihaz kullanma becerisi ve hastan?n ya?? olarak bildirildi.
Sonu?: Etkin inhaler i?in temel ?n ko?ul olan inhaler cihazlar?n uygun kullan?m?na ili?kin hekimlerin fark?ndal??? artm??t?r. Bu ?al??man?n sonu?lar? profesyonel bir hasta e?itimi i?in daha fazla giri?imin gerekli oldu?unu g?sterdi. Hasta e?itiminde hekimlere yard?mc? sa?l?k ?al??anlar?n?n destek olmas? ve hasta e?itimi i?in hekimleri motive edecek giri?imlere ihtiya? vard?r.
Anahtar Kelimeler: Ast?m, KOAH, inhaler cihazlar, hekim bilgisi, cihaz e?itimi.
SUMMARY
The knowledge and considerations of the physicians regarding the inhaler devices in asthma and COPD: the INTEDA-1 study
A. Zafer ?ALI?KANER1, Can ?ZT?RK2, Emel CEYLAN3, Sevgi PEKCAN4, ?zge YILMAZ5, Sami ?ZT?RK6,
Cenk CAN7, Osman ?ENER8, ?lk? YILMAZ TURAY9, Nihal KO?10, Ramazan ERSOY11
1 Division of Allergy and Immunology, Department of Internal Medicine, Faculty of Meram Medicine,
Necmettin Erbakan University, Konya, Turkey,
2 Department of Chest Diseases, Faculty of Medicine, Gazi University, Ankara, Turkey,
3 Department of Chest Diseases, Faculty of Medicine, Adnan Menderes University, Aydin, Turkey,
4 Division of Pediatric Chest Diseases, Faculty of Meram Medicine, Necmettin Erbakan University,
Konya, Turkey,
5 Division of Pediatric Allergy and Chest Diseases, Faculty of Medicine, Celal Bayar University, Manisa, Turkey,
6 Department of Adult Allergy and Immunology, Haydarpasa Training Hospital, Gulhane Military
Academy, Istanbul, Turkey,
7 Department of Pharmacology and Clinical Pharmacology, Faculty of Medicine, Ege University, Izmir, Turkey,
8 Department of Immunology and Allergy Diseases, Gulhane Military Medical Academy, Ankara, Turkey,
9 Clinic of Chest Diseases, Ataturk Chest Diseases and Chest Surgery Training and Research Hospital,
Ankara, Turkey,
10 Department of Physiology and Clinical Physiology, Faculty of Cerrahpasa Medicine, Istanbul University,
Istanbul, Turkey,
11 Clinic of Adult Allergy Diseases, Yedikule Chest Diseases and Chest Surgery Training and Research Hospital,
Istanbul, Turkey.
Introduction:The present paper was aimed at indicating and discussing the possible problems related to inhaler devices by considering the knowledge and practices of the physicians regarding the inhalation therapies.
Materials and Methods: The present study is a prospective, cross-sectional survey carried out by Turkish Respiratory Society? Inhalation Therapy Group? between February 2010 and February 2011 with a participation of ten individual centres. Seven inhaler devices that were available on the market in the country were assessed.? The data on the problems that 684 clinicians actively attending patients with respiratory disorders experienced in daily clinical practice or their evaluations of their patients were obtained through the questionnaire.
Results: The respondents, most of whom were pulmonologist (37.5%), and pediatrist (38.1%), had been,on average, 11.6? years in profession. The source of information on inhalers and administration techniques were reported to be mainly the internet and patient leaflets.? Of the participants only 18.5% reported to have had adequate knowledge of inhaler devices and proper administration techniques.? Most of the participants stated that they themselves provided the instructions of administration and that the method was often verbal explanation. The physicians believed that although approximately 60% of the patients used the drug correctly, 40.7% made critical mistakes to have adverse effects on the therapeutic outcome.? The most important criteria on which the physians lay greater emphasis in choosing the inhaler devices were the physical capability, skills and age of the patients.
Conclusion: The awareness of proper use of inhaler devices is a fundamental prerequisite for effective inhalation therapy has been improved in physicians. The results of the present study have shown that more effort is required for professional training. Assisting the physicans with medical personnel for training of the patients and educational motivation are required.
Key Words: Asthma, COPD, inhalation devices, physician's knowledge, device education.
Tuberk Toraks 2013; 61(3): 183-192 ? doi:10.5578/tt.5343
Geli? Tarihi/Received: 19/04/2013 - Kabul Edili? Tarihi/Accepted: 13/05/2013
* Bu ?al??ma, EAACI Kongresi (11-15 Haziran 2011, ?stanbul, T?rkiye)'nde sunulmu? ve poster ?d?l? kazanm??t?r. Bu ?al??ma 18. ISAM Kongresi (18-22 Haziran 2011, Rotterdam, Hollanda)'nde sunulmu?tur.
** This study was presented in EAACI Congress 2011, 11-15 June, Istanbul, Turkey and won poster prize. This study was presented in ISAM 18th Congress 2011, 18-22 June, Rotterdam, Nederlands.
INTRODUCTION
Asthma and chronic obstructive pulmonary disease (COPD) have enormous effects on the individual, the families and the society. The prevalence of both diseases has been increasing in parallel with aging, increased environmental pollution and tobacco consumption, and exposure to biomass for heating and cooking. The treatment of patients with asthma or COPD, especially if moderate or severe, requires the regular administration of several drugs through inhalation (1,2). The wide variety and number of inhaler devices enables the physician to choose the appropriate aerosol treatment, but make it difficult for both the physician and the patient to choose appropriate device and to use it properly (3). Selecting an appropriate device for the individual patient and the clinical setting is critical to the success of therapy. The misuse of the devices has been found to be associated with decreased disease control in asthmatics (4,5).
It is known to the pulmonologists that the technical properties of the device system are important in improving the effectiveness of the inhaled medication (6). The newly designed inhaler devices are aimed at improving the lung deposition of inhaled medications, yet more important is the correct use of the technique (4,7).
Current guidelines on treating asthma and COPD recommend that the physician demonstrate the patient at the initial visit how to use the various devices, and then determine at regular follow-up visits if the device chosen is used properly (1,2). However, this is not the case in clinical practice as evidenced by the high percentage of healthcare professionals who are incapable of simply demonstrating correct use of inhaler devices (8,9).
The applications of portable inhalers beginning with the "hand-bulb nebulizer" in 1950's made presumably the most remarkable progress in its history when the first pMDI device was marketed in 1956 (10). However, there appeared some problems, such as improper inhalation and administration techniques, oropharyngeal deposition of inhaled medication, leading to a search for better inhalation therapies. The introduction of the first DPI in 1980s was believed to be beneficial in overcoming many problems concerned with the treatment of chronic respiratory tract diseases (9,10). However, the performance of the dry powder inhalers have been insufficient to control the disease process in both asthma and COPD. The physician often simply prescribes inhaler therapy, taking for granted that the patient could use it properly, whereas the majority of patients do not realize that the efficacy of inhaler therapy often depends on whether to use it correctly or not (11).
Today it is generally accepted that poor device use is one of the reasons for poor disease control. Patient-oriented studies have shown that the vast majority of the patients made mistakes with their inhalation devices which may compromise the therapeutic outcome (12). Failure to use inhaled medication properly may decrease the treatment efficacy. Thus the patient will avoid using the prescribed inhaled medication as he/she suspects of the treatment efficacy. Mishandling of inhaler devices decreases the compliance and adherence of the patient to the inhaled therapeutic regimen, compromising the treatment efficacy (13).
There are several reasons for inadequate inhaler use, such as inattentiveness, lack of consideration for therapy, mental or physical incapabilities. However, most important is that physicians have not duly considered the inhaled drug therapies, or that they have been insufficient to train the patient (9). The present study was carried out to inquire about the knowledge of and level of awareness of the inhalers exhibited by the physicians who attend the patients with asthma and/or COPD.
MATERIALS and METHODS
The INTEDA-1 study was a prospective, cross-sectional, questionnaire-based survey carried out by the Turkish Respiratory Society Inhalation Therapy Group (INTEDA) between February 2010 and February 2011 with a participation of ten individual centres. The study protocol and informed consent were approved by the Research Council and Ethics Committee of Gulhane Military Medical School.
The Study Population
The questionnaire was given to those who attend patients with asthma and COPD and prescribe inhaler drug and therapies. Those, such as pulmonologist, internist, and family physician who involve in the follow up of adult patients, and/or those such as pediatrist, family physician who follow up pediatric subjects were included in the study. The informed consent was obtained from each participant.
Questionnaire
The questionnaire of the study was revised by an exclusive council consisting of at least 12 specialists dealing with the subject. It was designed in two parts. The first part contained the age, gender, the date of graduation, the field of specialty, the academic degree, current institution and contact information of the participants. The second part consisted of a total of 21 questions, two of which were open and inquired about the experiences of the physicians concerned with mishandling inhaler devices and their considerations of the factors affecting the therapeutic outcome. The questionnaire covered questions concern with seven inhaler devices commercially available in Turkey (metered-dose inhaler, discus, turbuhaler, aerolizer, handyhaler, easyhaler and nebulizer). The reproduction, distribution, and recollection of the questionnaire were financed by Turkish Respiratory Society.
Study Project
The study was conducted in ten individual centers. Each center had its own researcher who conducted the study in the health centers and institutions of their own areas. The coordination of the study at each center was carried out by a supervisor by whom the collection, pre-evalution, and statistical analysis of the data were performed.
Statistical Analysis
Having been entered in variables into SPSS 15.0 for Windows, the results of the questionnaire were analyzed. The demographic data were designated as mean ? SD. The responses to the questions were displayed in "percentages" in the tables.
RESULTS
A total of 1000 questionnaires were given and 707 were returned. Table 1 shows the demographic and occupational features of the respondents. Twenty-two excluded from the analysis because their questionnaires were found not to be suitable enough for evaluation, the remaining 685 questionnaires were assessed. Overall response rate was 68.5%. The demographic and occupational characteristics of the physicians enrolled were presented at Table 1.
Of the participants, 50.2% were female and 49.8% were male, with the mean age being 35.40 ? 7.93 years. The mean tenure of the respondents was 11.57 ? 7.96 years, most of whom are pediatrists and pulmonologists, and work at the training and research hospitals as residence or specialist. Nearly half attended only adults.
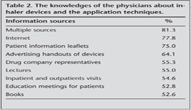
Several sources of information about inhaler devices and application techniques were described by the physicians. The answers to the question "What are the sources of your knowledge about inhaler devices and the application techniques?" are shown in Table 2. It is noteworthy that the most common source of information was stated to be the internet and the drug leaflets.
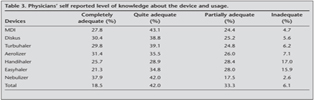
To the question of "whether their knowledge of inhalation devices and application techniques is satisfactory enough", only 18.5% answered that they had completely adequate knowledge of "all inhalation devices and administration techniques". Table 3 shows the physicians' self-reported level of general knowledge of administration techniques of different inhaler devices. The percentage of the answers of quite adequate, partially adequate and inadequate was found as 42.0%, 33.3% and 6.1%, respectively. The knowledge of the physicians concerning inhaler devices such as MDI, discus, turbuhaler, aerolizer, handihaler, easyhaler and nebulizer was evaluated separately for each device. The respondents found themselves completely satisfactory and highly satisfactory mostly on nebulizers, but felt themselves less adequate about easyhalers and handyhalers. The awareness of and level of knowledge about the newly-introduced devices are poorer.
To the question of "Who should provide the first training on inhalation devices to the patients?" most physicians (68.8%) answered that they provided the first device training for the patients on the inhaler therapy prescribed. The remaining include health care providers other than physicians, including nurses (16.2%), respiratory physiotherapists or technicians (3.4%) and residents (1.5%). Of the physicians, 10.2% stated that they were unable to provide initial education for various reasons.
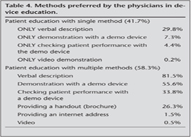
As to the first inhaler and reinforcement training, the question of "Which methods do you practice for the first training of inhaler device?" was asked. Physicians used more than one method for inhaler training; verbal explanation was stated to be the most common method. Table 4 summarizes the training methods for inhalation devices preferred by the physicians and the frequency of training.
The another question was "Are the time allocated for the first training for inhaler device and its application techniques adequate?". Time spent on the first education of patients for inhalation device use was considered adequate by 56.6% of the physicians (9.27 ? 6.18 minutes), but inadequate by 44.3% (3.69 ? 2.16 minutes). According to the answers in the questionnaire, it was found that 87.7% of the respondents gave reinforcement training at least once.
About the correct application rates of inhaler devices, the question "What are the correct application rates for inhalation devices by the patients in general in your opinion?" was asked. The estimation of the physicians about the percentage of the proper use of inhalation device is up to 60%, yet they believed that up to 40.7% of the patients made such mistakes as to affect the outcome of the treatment.
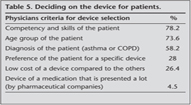
What criteria do you consider for the choice of inhaler devices? Of the participants 83.3% considered more then one criterion for the selection of inhaler. Criteria considered in device selection are summarized in Table 5. The physical capacities and skills, and age of the patients were the most important criteria the physicians considered in the selection of the inhaler. One important criterion was the type of disease (Table 5).
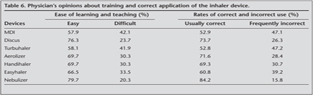
Physicians' opinions about the ease of learning and teaching inhalation devices and rates of correct use are summarized in Table 6. The physicians believed that nebulizers and discus were the easiest to teach and use, but MDIs and turbuhalers were the most difficult. They thought that nebulizers, discus, aerolizers and handyhalers were used more correctly, but MDIs and turbuhalers might be used inadequately (Table 6).
Inhaler Training Programmes for Physicians/Health Care Practitioners
Almost all the respondents agreed that the training and educational programmes on every aspects of inhalers for physicians and healthcare personnel were essential (98%). There was also consensus that the programmes would improve therapeutic compliance and the quality of life and decrease emergency department visits, hospitalization and therapeutic costs (97%). The programmes were also considered to improve mortality (88.7%).
Inhaler Mishandling
Seventy-five different patient errors in device use (a total of 789) were reported by the physicians. Among them (789 occurrences) were 51 errors that are "known" or "expected" (Table 7). The remaining 25 errors (200 occurrences) were those which were not directly related to inhalation technique and "unpredictable", such as drinking drug solutions, attempt to inhale the MDI drug sprayed into air or nasal route of administration. Most of the reported events regarding unusual use of inhalers was concerned with DPI. Some inhalation errors were reported with DPI, such as puncturing the capsule to inhale the drug, using turbohaler through an aerochamber, inhaling the powder of discus through a pipette.
DISCUSSION
The findings in the present study showed that physicians who prescribe inhalation therapies and devices may be in part responsible for the patient errors in device using patterns. To increase awareness, continued medical education activities about related topics must include the specific contents of inhaler treatment and the fundamentals of inhaled therapy. To increase the efficacy of the treatment and decrease the economic losses, the proper use of inhaler devices available and drug combinations by the patient must be promoted.
The present study was a research in which the knowledge and experiences on the inhaler devices were first inquired about in a comprehensive, multidisciplinary sample of physicians selected from a variety of specialists dealing with respiratory disorders in Turkey. The study group consisted of airway disease specialists, mostly pulmonologists and pediatrists, as well as internists, family physicians and medical practitioners.
The physicians involved in the study obtained the knowledge on the inhalers and inhalation techniques from various sources, such as internet and drug leaflets. However, there were a small number of clinicians who considered their own knowledge concerned completely satisfactory. The reason for this might be the failure of the clinicians to completely perceive the operating principles of the inhalers and the rationale for the inhaled therapies. When the physician's knowledge of the type of inhaler devices was evaluated for each device, the knowledge on the newly-introduced devices in our country was less satisfactory than that on the earlier ones (Table 3). The physicians indicated that they found themselves completely satisfactory and highly satisfactory mostly on nebulizers. The fact that 38% of those in the study group consisted of pediatrists and 37.5% pulmonologists may be a sufficient explanation for the adequate knowledge of nebulizer treatment, since the nebulizer treatment is the earliest inhaled treatment modality most commonly used by that group of physicians.
Approximately 70% of the physicians in the study group stated that they themselves provided the initial training and education about the inhaler devices prescribed to the patients, whereas 10% reported that they were unable to do so for various reasons. It has been reported that in some institutions, a nurse experienced on inhaled therapies carried out the task of instruction by 16.6%. Some studies reported that several methods, mostly verbal instructions and demonstrations, were employed in inhaler training and education (14,15). In addition, some studies have shown that the patients tended to be instructed by their own physicians, and through demonstration. In our previous study in which various methods of inhaler therapies were compared, and the patient preferences were assessed, 73.2% of the subjects stated that they preferred to obtain initial inhaler education from the physician who prescribed the inhaler treatment. Among the preferred ways of inhaler training were demonstration (56.3%), video (19%), and brochures and leaflets (18%) (16). The studies concerned have showed that correct device handling has to a large extent improved the therapeutic outcomes (17).
A group of pulmonologist from Brasil tried to identify which factors were considered in the choice of the inhaled therapies (6). Two thirds of the interviewees indicated that both inhaler and oral ways of treatment were equally important. More than 80% of the pulmonologists interviewed stated that the inhaler chosen was as important as or more important than the pharmacological agent prescribed and that device features were important as well. According to the interviewees, the simplicity of usage was the most important characteristic in the choice of the system. The percentage of the choice of the system by the phyisican is as follows: "simple to use" was cited by 38%, the degree of penetration in the bronchial tree was cited by 15% and the opinion of the patient was cited by 12%. It is noteworthy that the cost of the system was the least reported factor (7%) (6). In our study, the principal factors involved in the choice of the inhaler device for patients with asthma and COPD were the physical ability, skill, and age of the patients. The type of the device, however, was considered by the participants to be of little importance.
Inhaler choice by the physicians dealing with airway diseases is closely related to both the socioeconomic status and cultural background of the patient, and the level of development and health insurance systems of the country. A survey from Malaysia which inquired about asthma-specific prescribing practices of government and private doctors showed different preferences between them (18). Over half the government and private physicians chose MDI as their first choice device. MDI plus spacer ranked second by the government physicians (24.1%), while among private physicians, three types of inhaler devices (MDI plus spacer, turbuhaler, and nebulizer) ranked second (14.2% in each). The primary concerns for choosing inhaler devices were found different between the two groups. The majority of government physicians quoted technical ability as their primary concern, while cost and personal preferences ranked equally as main primary concerns with the private physicians (18). One remarkable result of the Malaysian survey was that private physicians prescribed oral bronchodilators more frequently. The most common reason for private physicians to prescribe oral preparation was the cost and the patient reluctance to use inhaler device. In contrast, inability to correctly handle inhaler device was the most quoted reason for government physicians. The adherence of the patients to inhaler devices was at average level according to Malaysian physicians. 17.3% of excellent compliance and 73% of average compliance were estimated by both physician groups (18).
Above mentioned study from Brasil attempted to identify the principal factors involved in the choice of the therapeutic regimen for asthmatics and patients with COPD. The principal factor cited was the information obtained from the results of clinical trials according to most respondents. This addresses the issue of the best clinical practices recommended. According to the responses obtained, the information made available by the pharmaceutical companies, whether on the internet, through symposia (conferences, seminars, etc.) or in visits made by the sales force to the office/hospital, has little or no effect on the choice of the medication. The same was true for the sponsorship, the financial support that the pharmaceutical industry provides in order to encourage physicians to participate in conferences, congresses (6).
One review of inhaler technique after training concluded that there was no difference in the ability of patients to use DPIs or MDIs (19). However, even with training, not all patients could use their inhalers correctly; this was true for both MDIs and DPIs (20,21). The most recent guidelines on asthma and COPD indicate that the most important requirement is that the chosen dispenser is used properly (1,2). This suggestion, based on the evidence that errors in use and maintenance are frequently made in all inhalation types of drug dispensers, requires that all medical staff pay more attention to the educational aspects of inhalation therapy (15,22,23). It is clear to all that medical personnel require more time to attend an individual patient (15). In our study, approximately nine-minute training has been found by the participants involved in the study to be satisfactory.
In conclusion, it is important to recognize that inhalation therapy is a complex way of treatment for both physicians and patients. The present study has shown that training patients as well as physicians is necessary to achieve the desirable therapeutic conditions, which was also emphasized by most of the participants. Practices of inhaled therapies require that a better communication with the patient be established and that additional time with the patient be spent. It is important that the physician be motivated to allocate optimum time for inhaled therapies during the routine activities, or be supported by health care practitioners, thus providing adequate adherence to proper use of inhalers and improving the clinical status and therapeutic outcome of the patient, thereby increasing the cost effectiveness. It is important to emphasize that the trainings and their sustainability to save more in health expenditures should be supported by such components of the health system as physicians, nurses, and volunteers and by those suppliers of placebo devices.
ACKNOWLEDGEMENT
This study partially funded by Turkish Respiratory Society.
CONFLICT of INTEREST
None declared.
REFERENCES
- Global Initiative for Asthma, guidelines www.ginasthma.com/
- Chronic obstructive pulmonary disease, guidelines. www.goldcopd.com/Guidelineitem.asp
- Everard ML. Regimen and device compliance: key factors in determining therapeutic outcomes. J Aerosol Med 2006; 19: 67-73.
- Berger W. Aerosol devices and asthma therapy. Curr Drug Deliv 2009; 6: 38-49.
- Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J 2002; 19: 246-51.
- Campos HS, Lemos ACM. Asthma and COPD according to the pulmonologist. J Bras Pneumol 2009; 35: 301-9.
- Dolovich M. Drug delivery systems for administration of inhaled therapy in patients with chronic obstructive pulmonary disease. American Health and Drug Benefits 2008; 1(Suppl 4): 12.
- Plaza V, Sanchis J, Roura P, Molina J, Calle M, Quirce S, et al. Physicians' knowledge of inhaler devices and inhalation techniques remains poor in Spain. J Aerosol Med Pulm Drug Deliv 2012; 25: 16-22. doi: 10.1089/jamp.2011.0895.
- Hanania NA, Wittman R, Kesten S, Chapman KR. Medical personnel's knowledge of and ability to use inhaling devices. Metered-dose inhalers, spacing chambers, and breath-actuated dry powder inhalers. Chest 1994; 105: 111-6.
- Anderson PJ. History of aerosol therapy: liquid nebulisation to MDIs to DPIs. Respir Care 2005; 50: 1139-50.
- Melani AS. Inhalatory therapy training: a priority challenge for the physician. ACTA BIOMED 2007; 78: 233-45.
- Molimard M, Raherison C, Lignot S, Depont F, Abouelfath A, Moore N. Assessment of handling of inhaler devices in real life: an observational study in 3811 patients in primary care. J Aerosol Med 2003; 16: 249-54.
- Melani AS, Bonavia M, Cilenti V, Cinti C, Lodi M, Martucci P, et al; Gruppo Educazionale Associazione Italiana Pneumologi Ospedalieri. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med 2011; 105: 930-8. doi: 10.1016/j.rmed.2011.01.005.
- Erickson SR, Landino HM, Zarowitz BJ, Kirking DM. Pharmacists' understanding of patient education on metered-dose inhaler technique. Ann Pharmacother 2000; 34: 1249-56.
- Capstick TG, Clifton IJ. Inhaler technique and training in people with chronic obstructive pulmonary disease and asthma. Expert Rev Respir 2012; 6: 91-103.
- Ceylan E, Akko?lu A, Erg?r G, Y?ld?z F, ?til O. Inhaler use and device preferences of asthmatic patients: role of education on appropriate device use. Turkish Respiratory Journal 2008; 10: 40-7.
- Schulte M, Osseiran K, Betz R, Wencker M, Brand P, Meyer T, et al. Handling of and preferences for available dry powder inhaler systems by patients with asthma and COPD. J Aerosol Med Pulm Drug Deliv 2008; 21: 321-8. doi: 10.1089/jamp.2007.0634.
- Loh LC, Wong PS. Asthma prescribing practices of government and private doctors in Malaysia- A nationwide questionnaire survey. Asian Pacific Journal of Allergy and Immunology 2005; 23: 7-17.
- Brocklebank D, Ram F, Wright J, Barry P, Cates C, Davies L, et al. Comparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literature. Health Technol Assess 2001; 5: 1-149.
- Lenney J, Innes JA, Crompton GK. Inappropriate inhaler use: assessment of use and patient preference of seven inhalation devices. EDICI. Respir Med 2000; 94: 496-500.
- R?nmark E, J?gi R, Lindqvist A, Haugen T, Meren M, Loit HM, et al. Correct use of three powder inhalers: comparison between Diskus, Turbuhaler, and Easyhaler. J Asthma 2005; 42: 173-8.
- Crompton GW, Barnes PJ, Broeders M, et al. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respir Med 2006; 100: 1479-94.
- Fink JB, Rubin BK. Problems with inhaler use: a call for improved clinician and patient education. Respir Care 2005; 50: 1360-74.
Yaz??ma Adresi (Address for Correspondence):
Dr. Sevgi PEKCAN,
Necmettin Erbakan ?niversitesi Meram T?p Fak?ltesi,
Pediatrik G???s Hastal?klar? Bilim Dal?,
KONYA - TURKEY
e-mail: emelceylan@ymail.com