Primer spontan pn?motoraks, pn?momediastinum ve
ard?ndan geli?en subk?tan amfizemli bir olgu
Halil BEYD?LL?1, Ne?at?ULLU2, Serdar KALEMC?3, Mehmet DEVEER2, Serhat ?ZER4
1 Mu?la Devlet Hastanesi, Acil Klini?i, Mu?la,
2 Mu?la Devlet Hastanesi, Radyoloji Klini?i, Mu?la,
3 Mu?la Devlet Hastanesi, G???s Hastal?klar? Klini?i, Mu?la,
4 ?zmir Atat?rk E?itim ve Ara?t?rma Hastanesi, Dahiliye Klini?i, ?zmir.
Tuberk Toraks 2013; 61(2): 164-165 • doi:10.5578/tt.5089
Geli? Tarihi/Received: 13.03.2013 - Kabul Edili? Tarihi/Accepted: 03.04.2013
We report a case of spontaneous pneumothorax, pneumomediastinum and subcutaneous emphysema following a cough episode and have a mind to emphasize the clinical diagnosis of pneumothorax and pneumomediastinum presenting with shortness of breath and chest pain without any history of trauma.
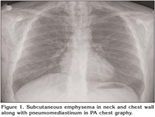
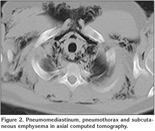
A 17 year-old male patient applied to emergency room with chest pain, mild dyspnea and rising swelling in neck following a cough two days ago. Chest X-ray and routine biochemical parameters were normal and he was recommended to apply to pulmonology outpatient clinic along with certain medical prescriptions. He reapplied to emergency room upon progressing complaints two days later. In the initial evaluation, the Glasgow Coma Scale was 15 while oxygen saturation 95%, arterial blood pressure 115/85 mmHg, heart rate 95/minute and body temperature 37.5?C. Respiratory examination revealed no abnormal finding, however, subcutaneous crepitations extending scapula were detected around neck region in palpation. No other systemic abnormalities were observed. Electrocardiography was normal. Those noted in PA-chest X-ray were subcutaneous air in bilateral neck and chest wall, together with pneumomediastinum (Figure 1). Pneumomediastinum, minimal pneumothorax and extensive air collection within soft tissues in whole chest wall and neck were observed in computed tomography taken for verification of pathological findings observed in chest X-ray (Figure 2). Having no history of smoking along with individual or familial disorder, he was diagnosed with Primary spontaneous pneumothorax (PSP). Despite extensive pneumomediastinum and subcutaneous emphysema, he had minimal pneumothorax and was admitted to inpatient clinic of pulmonology. Following high-frequency oxygen therapy (10 L/minute) in pulmonology clinic, his complaints and radiologic findings improved and he was discharged. Because this is an uncommon case, it has been thought to be presented here.
PSP most commonly presents clinically with dyspnea, chest pain and cough. Similarly, our case did with dyspnea and chest pain, and he was diagnosed and begun treatment two days later. It can be inferred when reviewing literature that more than 46% of PSP cases are diagnosed two or more days after the onset of symptoms. Major reason of such delay is thought to be patients not seeing a doctor despite having relevant symptoms (1). Another cause of such delay might be the insufficiency of direct PA-chest X-ray. Thus, lateral chest X-ray must necessarily be taken in such patients (2). There exist some studies indicating lateral chest X-ray to be as sensitive as computed tomography in detecting pneumothorax (3). In our case, lack of lateral chest graphy at initial evaluation led to a delay in diagnosis. At the second application, computed tomography was taken upon a suspicion for pneumothorax based on detection of subcutaneous emphysema, resulting in establishment of diagnosis.
Due to mild symptoms, extent of pneumothorax to be low but presence of pneumomediastinum and accompanying subcutaneous emphysema, we administered high-frequency oxygen therapy (10 L/minute) to our patient. We noted an improvement in pneumothorax and symptoms during follow-up. We inferred that oxygen alone can be adequate in treating non-traumatic pneumomediastinum and subcutaneous emphysema. We could not find any case of PSP, extensive pneumomediastinum plus subcutaneous emphysema following cough in literature.
CONFLICT of INTEREST
None declared.
REFERENCES
- O'Hara VS. Spontaneous pneumothorax. Mil Med 1978; 143: 32-5.
- Simsek F, Akcil M, Balkanay O, Demirkaya A, Kaynak K. Simultaneous bilateral spontaneous pneumothorax. Cerrahpasa Journal of Medicine 2008; 39: 37-40.
- Carr JJ, Reed JC, Choplin RH, Pope TL Jr, Case LD. Plain and computed radiography for detecting experimentally induced pneumothorax in cadavers: implications for detection in patients. Radiololgy 1992; 183: 193-9.
Yaz??ma Adresi (Address for Correspondence):
Dr. Serdar KALEMC?,
Mu?la Devlet Hastanesi,
G???s Hastal?klar? Klini?i,
MU?LA - TURKEY
e-mail: skalemci79@mynet.com