Kontrols?z ast?m tan?s?yla izlenen ?zefageal akalazya olgusu
?m?r AYDIN1, Cabir Y?KSEL2, Timur TUNCALI3, Murat ?ZKAN2, Ak?n KAYA4, ?lker ?KTEN2,
Zeynep MISIRLIG?L1
1 Ankara ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?mm?noloji ve Allerji Bilim Dal?, Ankara,
2 Ankara ?niversitesi T?p Fak?ltesi, G???s Cerrahisi Anabilim Dal?, Ankara,
3 Ankara ?niversitesi T?p Fak?ltesi, T?bbi Genetik Anabilim Dal?, Ankara,
4 Ankara ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara.
?ZET
Kontrols?z ast?m tan?s?yla izlenen ?zefageal akalazya olgusu
Akalazya, alt ?zefageal sfinkterin yetersiz gev?emesi ve ?zefagusta peristaltizmin olmamas? durumudur. Nefes darl??? yak?nmas?yla kendini g?sterebilir. On sekiz ya??ndaki erkek hasta ?ks?r?k, nefes darl??? ve h?r?lt? yak?nmas?yla hastaneye ba?vurmu? ve ast?m tan?s? alm??t?r. Yak?nmalar?nda d?zelme olmamas? ?zerine ast?m tedavisi giderek art?r?lm?? ve en sonunda kontrols?z ast?m ?n tan?s?yla klini?imize y?nlendirilmi?tir. Akci?er grafisinde hafif ?st mediastinal geni?leme izlenirken, akci?er tomografisinde a??r? geni?lemi? ?zefagusun trakeaya bas? yapt??? g?r?ld?. Hasta akalazya ?n tan?s?yla g???s cerrahisi klini?ine nakledildi. ?zefagusun baryumlu grafisi ve endoskopik incelemesi akalazya tan?s?n? do?rulad?. Hastaya Heller miyotomisi ve ?zefagogastrostomi uyguland?. Ameliyattan bir hafta sonra hastan?n nefes darl??? d?zeldi. Ameliyat?n birinci y?l?nda spirometri ve akci?er grafisi tamamen normal bulundu. Yanl?? ast?m tan?s?yla gereksiz yere ast?m tedavisi alan bu akalazya olgusuyla zor ast?mda ay?r?c? tan?n?n ?nemini vurgulamak istedik.
Anahtar Kelimeler: Zor ast?m, kontrols?z ast?m, ay?r?c? tan?, ?zefageal akalazya.
SUMMARY
Oesophageal achalasia misdiagnosed as uncontrolled asthma
?m?r AYDIN1, Cabir Y?KSEL2, Timur TUNCALI3, Murat ?ZKAN2, Ak?n KAYA4, ?lker ?KTEN2,
Zeynep MISIRLIG?L1
1 Division of Immunology and Allergy, Department of Chest Diseases, Faculty of Medicine, Ankara University,
Ankara, Turkey,
2 Department of Chest Surgery, Faculty of Medicine, Ankara University, Ankara, Turkey,
3 Department of Medical Genetic, Faculty of Medicine, Ankara University, Ankara, Turkey,
4 Department of Chest Diseases, Faculty of Medicine, Ankara University, Ankara, Turkey.
Achalasia? is characterized by incomplete lower oesophageal sphincter relaxation and aperistalsis of the oesophagus. It may present with dyspnea symptom. An 18-years-old male patient applied to a clinic with the complaints of cough, dyspnea, wheezing and diagnosed as asthma. Although his asthma treatment was increased in time while he did not recover, he was reffered to our hospital with the diagnosis of uncontrolled asthma. On chest X-ray there was a mild upper mediastinal enlargement and chest computed tomography revealed an over-dilated oesophagus constricting the trachea. The patient was referred to chest surgery clinic with a suspected diagnosis of achalasia. Barium-oesophagogram and endoscopic evaluation of the oesophagus confirmed the diagnosis of achalasia. The patient underwent Heller myotomy and oesophagogastrostomy. He was recovered in one week after the surgery without any complaint of dyspnea. Spirometry tests and chest X-ray resulted normal in one year. With this case of achalasia who used asthma treatment unnecessarily,we wanted to emphasize the importance of differential diagnosis of difficult asthma.
Key Words: Difficult asthma, uncontrolled asthma, differential diagnosis, oesophageal achalasia
Tuberk Toraks 2013; 61(2): 147-151 • doi: doino: 10.5578/tt.5778
Geli? Tarihi/Received: 04/03/2013 - Kabul Edili? Tarihi/Accepted: 29/04/2013
INTRODUCTION
Achalasia is characterized by incomplete lower oesophageal sphincter (LES) relaxation, loss of enteric neurons and aperistalsis of the oesophagus (1). It can be seen in all ages with an incidence of 0.5-1 per 100.000. Here we present a case of achalasia misdiagnosed as asthma for four years.
CASE REPORT
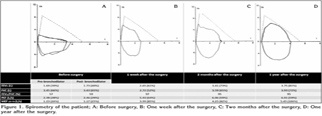
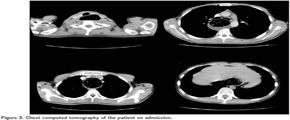
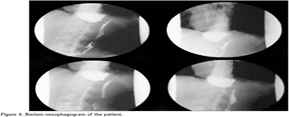
An 18-years-old male patient applied to a clinic with the complaints of cough, dyspnea, wheezing and diagnosed as asthma. A fluticasone/salmeterol combination inhaler therapy was prescribed. While he did not recover, inhaled steroid dosage was increased and montelukast was given as add-on-therapy. The patient was referred to our hospital with difficult asthma diagnosis. He reported cough increasing at night, regurgitation and dyspnea while eating. Spirometry revealed a non-reversible airway obstruction (Figure 1A). On chest X-ray there was a mild upper mediastinal enlargement (Figure 2A). Chest computed tomography revealed an over-dilated oesophagus constricting the trachea (Figure 3). The patient was referred to chest surgery clinic with a suspected diagnosis of achalasia. A clear narrowing of oesophagus at the oesophagogastric junction was seen in barium-oesophagogram (Figure 4). Oral intake was stopped and 3000 cc fluid was aspired with nasogastric tube. Endoscopic evaluation of the oesophagus revealed an increased pressure on lower oesophageal sphincter, dilated oesophagus without peristaltism. After left thoracotomy, increased pressure on lower oesophageal sphincter and dilated oesophagus was explored. The patient underwent Heller myotomy and oesophagogastrostomy. He was recovered in one week after the surgery without any complaint of dyspnea. Spirometry tests and chest X-ray resulted normal in one year (Figures 1B,1C,1D and Figure 2B).
On his visit after one year from the surgery, he looked pale and suffered from dyspnea for one month. Laboratory tests revealed a deep anaemia with a Hb value of 6.3 g/dL and a ferritin level of 1 ng/mL. The anaemia of the patient was considered to be due to his oesophagogastric surgery. He was consulted with the haematology clinic and iron defficiency anaemia diagnosis was confirmed. Upper gastroendoscopic examination resulted grade-C oesophagitis and alkaline reflux gastritis. After he was introduced oral iron tablets and proton pump inhibitors, his dyspnea recovered and laboratory test results were improved in three months.
The Allgrove (triple A) syndrome which is an autosomal recessive disorder was excluded from the case following a genetic work-up (2). The exclusion was based on the lack of family history and the absence of two other components, namely alacrima, and adrenocorticotrophic hormone (ACTH)-resistant adrenal insufficiency which are the characteristics of the triad beside achalasia (3,4). The patient was considered to have the non-syndromic (isolated) form of achalasia thereafter.
DISCUSSION
Achalasia is an idiopathic motility disorder of the oesophagus. During swallowing the lower oesophageal sphincter is unable to relax and there is no peristaltism along the oesophagus. The patients with achalasia usually suffer from progressive dysphagia and regurgitation and rarely chest pain, weight loss and dyspnea (1,5). Acute airway obstruction with stridor due to achalasia is also reported (6,7,8,9). Primary achalasia is usually seen in young patients while patients with secondary achalasia (pseudoachalasia, secondary to ie. tumors) are older with shorter duration of symptoms (5).
Isolated (or non-syndromic) achalasia is the most common form of achalasia and is mostly observed as sporadic cases. Albeit there have been repeated reports of familial achalasia, it's stated that the inheritance pattern in the majority of isolated achalasia cases is multifactorial hence complicating a phenotype-genotype correlation (10,11).
Diagnostic procedures include barium oesophagogram, upper endoscopy and oesophageal manometry (1). Among these, oesophegeal manometry is the gold standart. Aperistaltism, proximal dilatation of the oesophagus and high LES pressures are the typical findings of achalasia while appearance of oesophagus and LES pressures may be normal in some cases (5).
Treatment of achalasia aims to relax LES with the result of improved oesophagus emptying and symptom relief of the patients (1). Both medical and surgical treatment options are available. Medical treatment includes medicines like calcium channel blockers, nitrates and phoshphodiesterase inhibitors which reduce LES pressure. Endoscopic botulinum toxin injection may provide a symptomatic improvement for dysphagia. Endoscopic balloon dilatation has been used for classic treatment of achalasia, outcomes of this treatment was found better than botulinum toxin injection but it seemed to fail for treatment in young patients and high initial LES pressures. Surgical treatment with laparoscopic myotomy has also been used for achalasia and reported to have less symptom recurrence rate when compared to botulinum toxin injection (12). According to European Achalasia Trial in 2010, pneumatic dilatation and Heller myotomy had high and similar success rates at the end of two years follow-up period (13).
Many authors suggest laparoscopic myotomy and partial fundoplication. The myotomy is usually 7-8 cm in lenght and entends for 2.5 cm onto the gastric wall. Thoracoscopic approach can be used for myotomy but laparoscopic approach is more suitable for fundoplication and provides a longer myotomy distance. In order to decrease postoperative reflux symptoms, it is suggested to perform fundoplication after myotomy (5). In our case, because of his young age, Heller myotomy was chosen for treatment option. The Dor fundoplication was performed after myotomy in order to relief his dysphagia symptom and prevent gastroesophageal reflux disease.
The reason for the misdiagnosis of this patient may be due to his presenting symptoms. As his major symptom was dyspnea and other classical symptoms like dysphagia, regurgitation and weight loss are not mentioned to the doctor, he was diagnosed as asthma initially. After he was given asthma treatment, he returned to his doctor because he did not recover. In this step, he should be evaluated for uncontrolled asthma. First, his therapy compliance should be checked. Second, the triggering factors for asthma symptoms should be evaluated and co-existing diseases that may deteriorate asthma control should be detected. Finally the diagnosis of asthma should be confirmed if there is no change in disease progress. In this case he was considered as asthma and step-up treatment is given during the follow-up period. When he was sent to our clinic for further treatment, it was necessary for us to confirm the asthma diagnosis. At the end, the diagnosis was apart from asthma. With this case of achalasia who used asthma treatment unnecessarily,we wanted to emphasize the importance of differential diagnosis of difficult asthma
CONFLICT of INTEREST
None declared.
REFERENCES
- Fisichella PM, Carter SR, Robles LY. Presentation, diagnosis and treatment of oesophegeal motility disorders. Dig Liver Dis 2012; 44: 1-7. Epub 2011 Jun 22.
- MIM 231550 (http://omim.org/entry/231550)
- Allgrove J, Clayden GS, Grant DB, Macaulay JC. Familial glucocorticoid deficiency with achalasia of the cardia and deficient tear production. Lancet 1978; 1: 1284-6.
- Prpic I, Huebner A, Persic M, Handschug K, Pavletic M. Triple A syndrome: genotype-phenotype assessment. Clin Genet 2003; 63: 415-7.
- Patti MG, Herbella FA. Achalasia and other esophageal motility disorders. J Gastrointest Surg 2011; 15: 703-7.
- Tasker AD. Achalasia: an unusual cause of stridor. Clin Radiol 1995; 50: 496-8.
- Panzini L, Traube M. Stridor from tracheal obstruction in a patient with achalasia. Am J Gastroenterol 1993; 88: 1097-100.
- Arcos E, Medina C, Mearin F, Larish J, Guarner L, Malagelada JR. Achalasia presenting as acute airway obstruction. Digest Dis Sci 2000; 45: 2079-84.
- Dunlop SP, Travis SP. Achalasia presenting as acute stridor. Eur J Gastroenterol Hepatol 1997; 9: 1125-8.
- ACHALASIA, FAMILIAL ESOPHAGEAL. MIM 200400 (http://omim.org/entry/200400)
- Gockel HR, Schumacher J, Gockel I, Lang H, Haaf T, N?then MM. Achalasia: will genetic studies provide insights? Hum Genet 2010; 128: 353-64.
- Zaninotto G, Annese V, Constantini V, Del Genio A, Costantino M, Epifani M, et al. Randomized controlled trial of botulinum toxin versus laparoscopic Heller myotomy foe esophageal acalasia at a minimum 6 year follow-up. Ann Surg 2004; 239: 364-70.
- Boeckxstaens GE, Annese V, des Varannes SB, The European Achalasia Trial: a randomized multi-center trial comparing endoscopic pneumodilatation and laparascopic myotomy as primary treatment of idiopathic achalasia. Gastroenterol 2010; 138(Suppl 1): S53.
Yaz??ma Adresi (Address for Correspondence):
Dr. ?m?r AYDIN,
Ankara ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
?mm?noloji ve Allerji Bilim Dal?,
06100 Dikimevi, ANKARA - TURKEY
e-mail: mdomuraydin@gmail.com