Sa?l?k ?al??anlar?n?n anafilaksi hakk?nda bilgi d?zeyi
Ay?e BA??IO?LU1, Elif YILMAZEL U?AR2
1 SB Erzurum B?lge E?itim ve Ara?t?rma Hastanesi, ?mm?noloji ve Allerji Klini?i, Erzurum,
2 Atat?rk ?niversitesi S?leyman Demirel T?p Merkezi Yakutiye Ara?t?rma Hastanesi, G???s Hastal?klar?
Anabilim Dal?, Erzurum.
?ZET
Sa?l?k ?al??anlar?n?n anafilaksi hakk?nda bilgi d?zeyi
Giri?: Bu ?al??mada, sa?l?k ?al??anlar?n?n anafilaksi hakk?nda bilgi d?zeyi kendilerinin doldurdu?u anketler arac?l???yla de?erlendirildi.
Materyal ve Metod:?al??maya 1172 ki?i kat?ld?. ?al??maya kat?lanlar?n en fazla birinci basamak ve en az ???nc? basamakta olmak ?zere yar?s? anafilaksiyle daha ?nceden kar??la?m??t? (p= 0.005).
Bulgular: Kat?l?mc?lar?n %84.7'si anafilaksi semptomlar?n? do?ru yan?tlad?. Grubun %62.6's? anafilaksi tedavi basamaklar?n? do?ru bilirken, %44.7'si anafilaksiden ??phelendiklerinde epinefrin hakk?ndaki uygulamay? do?ru buldu. Grubun ??te biri epinefrini do?ru uygulama bilgisine sahipti. ?al??anlar?n %85.2'si hastay? allerji klini?ine y?nlendirmeyi ?nermesine ra?men, %33.7'si en yak?n allerji klini?inin nerede oldu?unu bilmiyordu. Kat?l?mc?lar?n sadece %20.3'? epinefrin oto-enjekt?r?n? biliyordu.
Sonu?:Anafilaksi, ?al???lan yer, meslek ve uzmanl?k alan?ndan ba??ms?z olarak T?rkiye'nin kuzeydo?u anadolu b?lgesinde genelde yetersiz tan? konularak tedavi edilmektedir.
Anahtar Kelimeler: Anafilaksi, e?itim, epinefrin, sa?l?k ?al??anlar?.
SUMMARY
Level of knowledge about anaphylaxis among health care providers
Ay?e BA??IO?LU1, Elif YILMAZEL U?AR2
1 Clinic of Immunology and Allergy, Erzurum Regional Training and Research Hospital, Erzurum, Turkey,
2 Department of Chest Diseases, Suleyman Demirel Medical Center Yakutiye Research Hospital,
Ataturk University, Erzurum, Turkey.
Introduction: Level of knowledge about anaphylaxis was evaluated in health care providers by using a self-administered questionnaire.
Materials and Methods: A total of 1172 participants responded to the survey, and previously half of them had met a case with anaphylaxis with a highest rate in primary and a lowest rate in tertiary care (p= 0.005).
Results: 84.7% of participants answered the questions about the symptoms of anaphylaxis correctly. Although 62.6% of the group knew correctly anaphylaxis treatment steps, 44.7% of them agreed to administer epinephrine if they suspected of a subject with anaphylaxis. One third of the group indicated appropriate route of epinephrine administration. 85.2% of participants agreed to refer the patient to allergy clinic despite 33.7% of the group were unaware of where the nearest allergy clinic was. Only 20.3% of the respondents have heard about epinephrine auto-injector.
Conclusion: Anaphylaxis was often diagnosed and managed inadequately, regardless of practice location, employment status and speciality in north-eastern Turkey.
Key Words: Anaphylaxis, education, epinephrine, gap, health care provider.
Tuberk Toraks 2013; 61(2): 140-146 • doi: 10.5578/tt.4812
Geli? Tarihi/Received: 18/10/2012 - Kabul Edili? Tarihi/Accepted: 13/05/2013
INTRODUCTION
Anaphylaxis is an acute generalized allergic reaction that can be life-threatening (1). However importance of anaphylaxis is underestimated. In Turkey, rising incidence of anaphylaxis is of great concern with mostly undiagnosed or unreported cases. In a retrospective study from Turkey, 224 cases of anaphylaxis were reported in 137 children from 1999 to 2009 (2).
Previous studies indicated a significant deficit in appropriate management of anaphylaxis (3,4,5). Diagnosis and treatment of anaphylaxis are challenging because reactions may be quick, and severe, and had a lack of clear definition which can lead to under-diagnosis (1,6). Furthermore, there is no single test to diagnose anaphylaxis in routine clinical practice, and there is a lack in reaching the updated knowledge which may be due to unwillingness, or language problems in reading foreign articles (1,4). Even though anaphylaxis is examined in tertiary care, guidelines for the management of anaphylaxis highlight the important role of primary care providers in the recognition, and referral of patients to allergy clinics (1). Therefore, anaphylaxis management plans are increasingly being advocated to improve outcomes from acute episodes (7).
In an effort to improve the management of anaphylaxis, we sought to identify the gaps about anaphylaxis knowledge of non-allergist health care providers in north-eastern Turkey.
MATERIALS and METHODS
The study participants were recruited from health centres located in north-eastern Turkey (Erzurum, Kars, Bayburt, Artvin, Gumushane, Ardahan, Erzincan, Agri, and Igdir). A survey was mailed to every local provincial health directorates to deliver the survey to health care centres. The study was approved by the local ethics committee.?
Eligibility criteria were: female/male subjects between ages of 18-65 years, working in a government hospital of primary, secondary or tertiary care. The target population was the ones who could meet patients with anaphylaxis, including medical doctors as non-allergist specialists, general practitioners, medical students, nurses, and paramedics.
Primary care was used for the first point of consultation for all patients within the health care system. Secondary care was the health care services provided by medical specialists. Tertiary care was used for an advanced medical investigation, usually for inpatients and on referral from a primary or secondary health professional.
The investigators created a 26-item, written questionnaire as multiple choices refined by administration to and feedback by an allergist, and a pulmonologist (Table 1). The questions were designed from guidelines of anaphylaxis (1). Subjects were instructed to self-administer the questionnaire with no time limit. After completing the questionnaire, participants were given a guide of anaphylaxis management plan including the right answers of the questions.
p value < 0.05 was regarded as statistically significant. Groups were compared with chi-square test for categorical variables and with one-way ANOVA for quantitative variables.
RESULTS
Surveys were returned from eight of nine cities. An overall response rate was 17.8% (2.2%-47.4%). A total of 1172 participants with female predominance, aged from 18 to 51 years responded to the survey. The study population's practice location was composed of primary (32.5%), secondary (38.4%), and tertiary (29.1%) care. Most of the participants were working as nurse, while the others were physician, paramedic or medical student. Department of the health care providers was mainly composed of family and preclinical medicine followed by with internal medicine, surgery, emergency medicine, preclinical science.
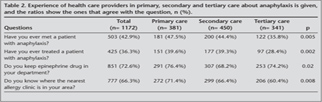
Slightly less than half of the study group had met a case with anaphylaxis (Table 2). Health care providers in primary health care had the most, and the ones in tertiary care had the least ratio of anaphylaxis experience (47.5% and 35.8%, p= 0.005). Almost one third of the group indicated that they had treated patients with anaphylaxis, with a lesser ratio in tertiary care providers compared to primary and secondary care providers (p= 0.002). Most of the participants indicated that they had epinephrine drug in their department, and this ratio was lesser in secondary care compared with primary and tertiary cares (p= 0.02). One third of the participants answered correctly where the nearest allergy clinic was, with a lowest ratio in tertiary care and highest ratio in primary care (60.4% and 71.4%, p= 0.008).
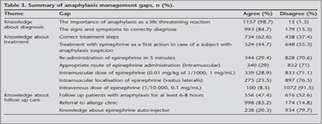
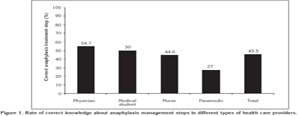
Almost all participants agreed that anaphylaxis was a life threatening reaction, whereas 84.7% of the group answered the questions about the symptoms of anaphylaxis correctly (Table 3). Although 62.6% of the group knew anaphylaxis treatment steps correctly, only 44.7% of them agreed that epinephrine should be administered as a first action if a patient was suspected of anaphylaxis. On the other hand 29.4% of the participants agreed that epinephrine might be re-administered in 5 minutes in case of no response. Knowledge about epinephrine administration was sufficient in less than one third of the group. Almost half of the participants agreed to follow up patients with anaphylaxis for at least 6-8 hours, and 85.2% of them agreed to refer the patient to an allergy clinic. However 20.3% of the respondents have heard about epinephrine auto-injector. Frequency of knowledge about how to manage anaphylaxis was sufficient in half of the group with a decreasing ratio as physicians, medical students, nurses and paramedics (p< 0.001) (Figure 1).
DISCUSSION
We evaluated the gaps in the evaluation of anaphylaxis in north-eastern Turkey where deaths from anaphylaxis by hymenoptera are not rare. Almost half of the study group had participated in the treatment of patients with anaphylaxis. Additionally, a few participants from tertiary care reported anaphylaxis experience which might be due to inadequate referral of anaphylaxis cases to tertiary care. Moreover, one third of the health care providers especially from secondary care reported that they didn't keep epinephrine drug in their clinic, in contrast to the statement of every step of health care should keep epinephrine independent of department type (1).
The knowledge level about anaphylaxis was found to be inadequate with many points including diagnosis, management and follow up. Even though the importance of anaphylaxis as a life threatening reaction was known by almost all health care providers, slightly less than all realised the signs and symptoms to diagnose anaphylaxis. Similarly, in a survey of paediatricians, nearly half of the respondents did not properly recognize and treat food-induced anaphylaxis (3). This lack of knowledge by health care providers mirrors that of previous studies as awareness of anaphylaxis was low in many countries (4).
Current anaphylaxis management guidelines recommend the use of epinephrine as a first line treatment, complemented by antihistamines and corticoids (1,8). Even though two third of the health care providers were able to answer the anaphylaxis treatment steps, less than half of the group were confident to administer epinephrine as a first action, and one third of them agreed to repeat epinephrine administration in case of no response. The reason of fail to use epinephrine as a first aid is probably due to its potential adverse effects (8). This fear can be defeated by the convincing effect of an evidence based education for the use of epinephrine in anaphylaxis in health care providers as reported before (9).
In this study, the rate of correct administration of epinephrine was very low. In a recent study, even in patients with severe anaphylaxis only 4% of them received epinephrine intramuscularly, whereas 8% received intravenously (8). Furthermore, education improved the correct use of epinephrine auto-injector from 23.3% to 74.2% in physicians (10).
Guidelines recommend that every patient who has experienced anaphylaxis should be referred to allergy clinic to get identified for the trigger(s) and for long-term management with an epinephrine auto-injector (1,8). In this study even though many practitioners indicated that patients with anaphylaxis should visit allergy clinic for further investigation, most of them were unaware of where the nearest allergy clinic was. Furthermore, only a quarter of the health care providers had heard about epinephrine auto-injector which might be due to its lack of availability in Turkey. This problem was also addressed in a study stating that epinephrine auto-injectors were available in 26 of 44 countries (9). Even though patients can have this drug by importing; it results with an increase in its cost. It is obvious that prevention of unavailability of epinephrine auto-injector will increase its prescription for the first-aid treatment of anaphylaxis.
Paramedics had the lowest ratio to correctly diagnose and manage anaphylaxis despite they were the first to confront with patients. Previously, it was reported that a large percentage of paramedics recognized classic anaphylaxis; however a very small percentage recognized atypical anaphylaxis (5).
The limitation of this study was the low response rates. However, this does not invalidate the study since the overall number of study participant is powerful enough to make a conclusion.
In conclusion, these results showed the current provision of anaphylaxis at least in this part of Turkey, which was often diagnosed and managed inadequately, regardless of practice location, employment status and speciality. Furthermore, experiencing anaphylaxis was not a frequent event in north-eastern Turkey. Therefore, a national educational programme should be developed to improve patient care and to prevent misdiagnosed cases and deaths from anaphylaxis. Findings from this study will be useful to provide a basis for developing interventional national strategies to resolve these deficiencies.
Conflict of interest
None declared.
REFERENCES
- Lieberman P, Nicklas RA, Oppenheimer J, Kemp SF, Lang DM, Bernstein DI, et al. The diagnosis and management of anaphylaxis practice parameter: 2010 update. J Allergy Clin Immunol 2010; 126: 477-80.
- Orhan F, Canitez Y, Bakirtas A, Yilmaz O, Boz AB, Can D, et al. Anaphylaxis in Turkish children: a multi-centre, retrospective, case study. Clin Exp Allergy 2011; 41: 1767-76.
- Krugman SD, Chiaramonte DR, Matsui EC. Diagnosis and management of food-induced anaphylaxis: a national survey of pediatricians. Pediatrics 2006;118; 554-60.
- Kahveci R, Bostanci I, Dallar Y. The effect of an anaphylaxis guideline presentation on the knowledge level of residents. J Pak Med Assoc 2012; 62: 102-6.
- Jacobsen RC, Toy S, Bonham AJ, Salomone JA, Ruthstrom J, Gratton M. Anaphylaxis knowledge among paramedics: results of a national survey. Prehosp Emerg Care 2012; 16: 527-34.
- Keskin O, Tuncer A. Anaphylaxis. Hacettepe T?p Dergisi 2005; 36: 98-104.
- Sin BA. Anaphylaxis. In: Candan I (ed). Medical Treatment. Ankara: ANTIP, 2003: 1261-71.
- Grabenhenrich L, Hompes S, Gough H, Ru?ff F, Scherer K, Pf?hler C, et al. Implementation of anaphylaxis management guidelines: a register-based study. PLoS One 2012; 7: 35778.
- Sin AB. Adrenalin autoinjector: properly used? Asthma Allergy Immunol 2009; 7: 1-2.
- Arga M, Bakirtas A, Turktas I, Demirsoy MS. Do pediatricians and the pediatric residents know how to use adrenalin autoinjector? Asthma Allergy Immunol 2009; 7: 26-31.
Yaz??ma Adresi (Address for Correspondence):
Dr. Ay?e BA??IO?LU,
SB Erzurum B?lge E?itim ve
Ara?t?rma Hastanesi,
?mm?noloji ve Allerji Klini?i,
ERZURUM - TURKEY
e-mail: aysebaccioglu@gmail.com