Geli?mekte olan bir ?lkede ven?z tromboembolizm tan? ve tedavisindeki gecikmeler
Mohammad Hossein RAHIMI-RAD1, Shaghayegh RAHIMI-RAD2, Sahar ZARRIN3
1 Urmia ?niversitesi T?p Fak?ltesi, Solunum Hastal?klar? B?l?m?, Urmia, ?ran,
2 Tabriz ?niversitesi T?p Fak?ltesi ??rencisi, Tabriz, ?ran,
3 Urmia ?niversitesi T?p Fak?ltesi, ?? Hastal?klar? B?l?m?, Urmia, ?ran.
?ZET
Geli?mekte olan bir ?lkede ven?z tromboembolizm tan? ve tedavisindeki gecikmeler
Giri?: Derin ven trombozu ve pulmoner tromboembolizmin h?zl? tan? ve tedavisi mortalite ve morbiditeyi azaltmaktad?r. Bu ?al??man?n amac?, geli?mekte olan bir ?lkede, derin ven trombozu ve pulmoner tromboembolizm tedavisindeki gecikmeleri ve ili?kili fakt?rleri ara?t?rmakt?r.?
Materyal ve Metod: Urmia, ?ran'da derin ven trombozu ve/veya pulmoner tromboembolizm tan?l? 353 hasta prospektif olarak ?al???ld?. Semptomlar?n ba?lang?? tarihi, klinisyen taraf?ndan yap?lan ilk de?erlendirme, tedavi ba?lang?c? ve tan?n?n do?rulanma bilgileri kaydedildi. Ayr?ca, baz? fakt?rlerle ili?kisi incelendi.
Bulgular: Semptomlar?n ba?lang?c?ndan tedavi ba?lanmas?na kadarki ortalama s?re 4.70 g?nd?, bu s?renin %89'u semptomlar?n ba?lang?c?ndan ilk medikal de?erlendirmeye kadar ge?en s?reydi (ortalama= 4.19 g?n). Semptomlar?n ba?lang?c?ndan tan?n?n do?rulanmas?na kadarki ortalama s?re 6.29 g?nd?. Ven?z tromboembolizmli 353 hastan?n 185 (%52.4)'i? semptomlar?n ba?lang?c?ndan sonra ilk iki g?nde, 168 (%47.6)'i iki g?nden sonra bir klinisyen taraf?ndan de?erlendirildi. Erken de?erlendirme ile ili?kili olan ve p de?eri < 0.05 olan fakt?rler, y?ksek e?itim d?zeyi, yak?n zamanda cerrahi, al?? varl???, bacakta ?i?meydi ve pulmoner tromboembolizmli hastalar?n derin ven trombozlu hastalara g?re daha erken de?erlendirildi?i saptand?. Ya?, cinsiyet, semptom say?s? ve ven?z tromboembolizm y?n?nden aile ?yk?s? ile ili?ki yoktu (p> 0.05). Y?ksek olas?l?k skorlu hastalarda ilk de?erlendirmeden tan?ya kadar ge?en s?re anlaml? olarak daha k?sayd?.
Sonu?: Ven?z tromboembolizmli hastalar?n ?o?unda tan? ve antikoag?lasyon tedavide gecikme vard?. Gecikmenin ba?l?ca nedeni hasta ile ili?kiliydi. Hastalar?n ven?z tromboembolizm konusunda fark?ndal???n? art?racak ve gecikmeyi k?saltacak stratejilere ihtiya? bulunmaktad?r.
Anahtar Kelimeler: Pulmoner tromboembolizm, derin ven trombozu, risk fakt?rleri, tan?da gecikme.
SUMMARY
Delays in diagnosis and treatment of venous thromboembolism in a developing country setting
Mohammad Hossein RAHIMI-RAD1, Shaghayegh RAHIMI-RAD2, Sahar ZARRIN3
1 Department of Respiratory Medicine, Faculty of Medicine, Urmia University, Urmia, Iran,
2 Tabriz University of Medical Students, Tabriz, Iran,
3 Department of Internal Medicine, Faculty of Medicine, Urmia University, Urmia, Iran.
Introduction: Rapid diagnosis and treatment of deep vein thrombosis and pulmonary thromboembolism reduce mortality and morbidity. The aim of this study is to investigate delays in treatment of deep vein thrombosis and pulmonary thromboembolism and related factor in a developing country.
Materials and Methods: We prospectively investigated 353 patients with diagnosis deep vein thrombosis and/or pulmonary thromboembolism in Urmia, Iran.? We recorded dates of symptom onset, initial visit by a clinician, initiation of treatment, and confirmation of diagnosis. We also analyzed relation with some factors.
Results: The mean interval from symptoms onset to initiation of treatment was 4.70 days, 89% of this interval was between onset of symptoms to first medical evaluation (mean= 4.19 days). Mean time from onset of symptoms to confirmation of diagnosis was 6.29 days. Of 353 patients with venous thromboembolism 185 (52.4%) visited by a physician within two days of onset of symptoms and 168 (47.6%) patients after two days. Factors that was associated with earlier seeking? with p value < 0.05 were pulmonary thromboembolism patients earlier than deep vein thrombosis, higher education, recent surgery, presence of cast, entire leg swelling. There was no association between age, gender, number of symptoms, and presence familial history of venous thromboembolism? (all p value > 0.05). The delays time from first visit to final diagnosis was significantly shorter in patients with high probability score.
Conclusion: Most patients with venous thromboembolism received anti-coagulation and diagnosis with delay. The main cause of delay is related to patient's delays. There is a need to improve people awareness about venous thromboembolism and to develop strategies to reduce delays.
Key Words: Pulmonary thromboembolism, deep vein thrombosis, risk factors, delayed diagnosis.
Tuberk Toraks 2013; 61(2): 96-102 • doi: 10.5578/tt.5348
Geli? Tarihi/Received: 05/01/2013 - Kabul Edili? Tarihi/Accepted: 23/04/2013
Introduction
Venous thromboembolism (VTE) including deep vein thrombosis (DVT) and pulmonary thromboembolism (PTE) are acute disease. Acute PTE is the cause of 50.000 to 200.000 death annually in the USA (1). Its mortality reported to be about 13% in first month? and? 35.3%? within three years after diagnosis. As many as 95% of PTE related deaths occur prior to diagnosis or within hours of the event (2,3,4). One study showed that patients diagnosed within 48 hours had better outcomes (5).
Despite the stated facts about VTE, delays in diagnosis and initiating treatment are a common problem. A study in USA reported delays in diagnosis in approximately 20% of patients with VTE. However, data about delays in the diagnosis of VTE in a developing country are sparse.
The aim of this study is to determine delays in diagnosis and treatment of VTE, and related factors in a developing country setting.
MaterialS and methods
We prospectively investigated 353 consecutive patients with imaging confirmed diagnosis DVT and/or PTE from May 2008 to August 2012. It was conducted at Imam Khomeini Hospital, a tertiary care hospital at Urmia University of Medical Sciences (Iran). It was approved by the university research council. The following information was collected:
a. Demographic data: i.e., age, sex, level of education,
b. Dates includes: the date of symptom onset, the date that the subject was first seen by medical personnel for these symptoms, the date that VTE treatment initiated, and the date on which the diagnosis was confirmed with imaging,
c. Presence of temporary risk factors for VTE at the time of symptoms onset and their relation with delays,
d. DVT or PTE probability scoring parameters on the day of admission to our center score (6,7).
Definition of Terms
1. Patients delay: Interval in days between onsets of symptoms to first seeking medical attention. It categorized as early, visit within two days of onsets of symptoms and late: after second day of symptoms onset.
2.? Diagnosis delay: Interval in days between first day seeking medical attention to final confirmatory imaging. It categorized as early, confirmation within first two days and late after second day of first seeking medical help.
3. Total diagnosis delay: Interval in days between first onsets of symptoms to final confirmatory imaging.
4. Delay in treatment, interval between onset of symptoms and initiation anti-coagulation.
Statistical Analysis
SPSS version 18 software is used.? Baseline characteristics are reported by descriptive analysis. Chi-square test is used to analyze the difference in frequencies between two groups.? p values < 0.05 are considered to be significant.
Results
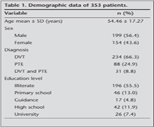
In this study 353 patients VTE (234 patients DVT only, 88 patients PTE only, 31 patients both PTE and DVT) were studied. The mean age of patients was 54.46 years. Of patients 199 (56.4%) were male and 154 (43.6%) were female. Table 1 shows baseline characteristics of patients.
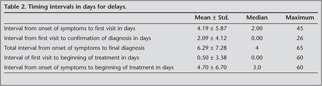
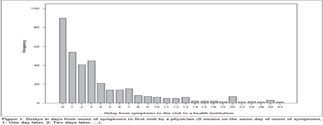
Mean interval from symptoms onset to initiation of treatment was 4.70 days, 89% of it was interval between onset of symptoms to first medical evaluation (mean= 4.19 days, for PTE patients 3.05 SD= 6.42 days for DVT patients 4.61 Sd= 5.78, and p= 0.037). Mean time from onset of symptoms to final diagnosis was 6.29 days. Most patents had initiation of treatment before confirmation of diagnosis, the mean time from first visit to final diagnosis 2.09 days and to beginning of treatment was 0.50 days. The Table 2 summarizes intervals time and Figure 1 shows distribution of time from onset of symptoms to first visit by a physician.
Of 353 patients, 90 (25.5%) patients found medical attention on the day of onset of symptoms, 298 (84.4%) received anticoagulation on first day of visit by physician and 195 (55.2%) had VTE confirmation on first day of visit.
Of 264 patients with DVT 52 (22.2%) found medical advice on the day of event and 58 (25%) patients after one week while patients with PTE 38 (31.9%) on day of symptom onset 16 (13.4%) after one week visited by a physician.
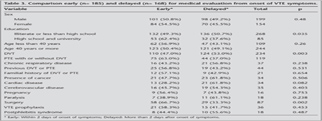
Of 353 patients with VTE 185 (52.4%) visited by a physician within two days of onset of symptoms and 168 (47.6%) patients visited after two days.
The comparison of related factors for these two groups is shown in Table 3. We found no difference in the gender and in the mean age of the two groups. There was also no statistically significant difference in the timing of seeking medical attention between patients younger than 40 year and patients older than 40 years. Patients with higher education level evaluated and diagnosed earlier. Patients with PTE had medical evaluation earlier than patients with DVT alone (p= 0.003).
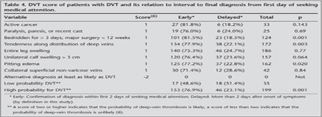
We recorded clinical probability of DVT and PTE on the day of admission to our center. The mean DVT probability score in 170 patients with final diagnosis of DVT within first two days of visit was 4.09 ? 1.32 and for 64 patients after the first two visit day was 3.20 ? 1.61 (p< 0.001). Table 4 summarized relation of diagnosis delay from first seeking medical attention to scoring system parameters, Bedridden or surgery, tenderness along distribution of deep veins, and pitting edema was significantly associated with early diagnosis (p< 0.005). Patients with high probability for DVT had significantly earlier diagnosis than those with low probability for DVT (p= 0.001). The mean Wells score in 71 patients with final diagnosis of PTE within first two days of visit was 5.33 ? 2.55 and for 47 patients with final diagnosis after the first two visit day was 3.96 ? 2.55 (p= 0.006). Patients with Wells probability score intermediate and high had earlier diagnosis than those with low probability (p= 0.024). Table 5 summarized diagnosis delay? relation to Wells PTE probability scoring parameters.
Discussion
Our study shows that mean interval between onsets of VTE symptoms to initiation of treatment is near to five days. This is while that it has been confirmed that early diagnosis and treatment reduces mortality for acute PTE (8).? It may also decrease the development of the post-phlebitis syndrome, and, chronic pulmonary hypertension following PTE (9,10). Non-specific symptoms and signs of VTE mimic other illnesses, and PTE is known as ?the Great Masquerader,? making diagnosis difficult even for experienced physicians.
In current study, most of the delay in the diagnosis and treatment of VTE represented the delay from symptom onset to the date of first medical evaluation. To our knowledge there are two studies that evaluated delay both DVT and PTE.? In a study by Elliot et al., with studying of 1152 patients with VTE (DVT n= 808, PTE n= 344) in North American hospitals, reported that the mean delay from symptom onset to medical attention was 2.9 days, which is shorter than the current study (4.19 days)(11). In second study by Ageno et al., among? 2047 patients (1505 with DVT and 542 with PTE) 64.0%? patients with PTE? 47.1% with DVT? had diagnosis less than five days (16).
In a study in Turkey the mean time from symptoms onset to the first admission to a health institution among patients with PTE was about 2.04 days which were shorter than our study for PTE patients (3.05 days) (12).
In a study by Jimenez Castro, of the 397 patients with acute PTE, 72 (18%) had a diagnostic delay while 325 (82%) did not, the median time from symptom onset to diagnosis was 7 days and 6% patients had a delay of more than 25 days (13).?
In Ireland, among 60 patients with PTE near to 50% of patients presented within 24 hours of onset of symptom, and 25% after one week (14). In current study, 31.9% of patients with PTE presented on day of onset of symptoms, which indicate a bad condition in a developing country setting.?
A study in Turkey among 156 with PTE showed that, 60.3% of them were admitted to a hospital within the first 24 hours of onset of symptom (12). In our study this rate was lower (22.2% for DVT and 31.9% for PTE).
In our study the delays from the date of first medical evaluation to the start of treatment is shorter than confirmation of VTE. It is a encouraging finding because guidelines recommend initiation of anticoagulation if clinical suspicion for PTE is high, even prior to confirmatory testing (15).
With regarding factors that affect on delays, as expected, first medical evaluation in patients with PTE occurred significantly earlier than those with DVT. It is in line with Ageno et al. study in Italy reported that delayed diagnosis 22.6% patients with DVT and in 16.2% with PTE (16). As also expected, patients with low education level had significantly delays in seeking medical attention. In a study by Bulbul et al. among patients with PTE, a high level of education were associated with longer patient delays, they didn't have explanation for it (12).? Our study showed that recent surgery, trauma and cast was associated with earlier seeking medical evaluation. Others also reported similar results (17,18). Similar to a large scale study in Italy (1505 with DVT and 542 with PTE) there was no relation between delays in seeking medical attention with gender, and age (16). Opposite to expectation patients with risk factors for VTE had not significantly earlier seeking medical attention which confirms of unawareness of lay persons about VTE risk factors. It is reported that current smoking and co-morbidity disease are associated with delayed diagnosis (12). We haven't investigated about relation with smoking, but our data did not showed relation with presence of cancer, heart disease, and chronic respiratory disease. We used the Wells scoring systems to determine the pre-test probability that a patient has DVT or PTE. The mean probability score in both DVT and PTE diagnosed in first two days of visit was significantly more than those diagnosed after two days of visit. This is expected and is in line with a study by Alonso-Mart?nez, where they showed that among 375 patients with PTE, those with a low Wells score show an increased time up to diagnosis (19).
Finding of this study, emphasis importance and essential role of public education for fast diagnosis and treatment of DVT and PTE. Similar to other common and serious disorders such as myocardial infarction, lay persons should learn to suspect for PTE for any unexplained shortness of breath, chest pain.
We conclude that there was a considerable delay from the onset of VTE symptoms to initiation of treatment, patients delays in seeking medical help constitute most part of this delay. Patients with high probability for VTE had earlier diagnosis. We suggest improving lay person's awareness about DVT and PTE, and their alarming symptoms.
CONFLICT of INTEREST
None declared.
REFERENCES
- Burge AJ, Freeman KD, Klapper PJ, Haramati LB. Increased diagnosis of pulmonary embolism without a corresponding decline in mortality during the CT era. Clinical Radiology 2008; 63: 381-6.
- Spencer FA, Gore JM, Lessard D, Douketis JD, Emery C, Goldberg RJ. Patient outcomes after deep vein thrombosis and pulmonary embolism: the Worcester Venous Thromboembolism Study. Archives of Internal Medicine 2008; 168: 425-30.
- Saeger W, Genzkow M. Venous thromboses and pulmonary embolisms in post-mortem series: probable causes by correlations of clinical data and basic diseases. Pathology, Research and Practice 1994; 190: 394-9.
- Wood KE. Major pulmonary embolism: review of a pathophysiologic approach to the golden hour of hemodynamically significant pulmonary embolism. Chest 2002; 121: 877-905.
- Kline JA, Hernandez-Nino J, Jones AE, Rose GA, Norton HJ, Camargo CA Jr. Prospective study of the clinical features and outcomes of emergency department patients with delayed diagnosis of pulmonary embolism. Academic Emergency Medicine 2007; 14: 592-8.
- Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med 2003; 349: 1227-35.
- Kearon C. Diagnosis of pulmonary embolism. CMAJ 2003; 168: 183-94.
- Smith SB, Geske JB, Maguire JM, Zane NA, Carter RE, Morgenthaler TI. Early anti-coagulation is associated with reduced mortality for acute pulmonary embolism. Chest 2010; 137: 1382-90.
- Bernardi E, Prandoni P. The post-thrombotic syndrome. Curr Opin Pulm Med 2000; 6: 335-42.
- Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med 2004; 350: 2257-64.
- Elliott CG, Goldhaber SZ, Jensen RL. Delays in diagnosis of deep vein thrombosis and pulmonary embolism. Chest 2005; 128: 3372-6.
- Bulbul Y, Ayik S, Oztuna F, Ozlu T, Sahin S. The relationship between socio-demographic characteristics of patients and diagnostic delay in acute pulmonary thromboembolism. Upsala J Med Sci 2011; 116: 72-6.
- Jimenez Castro D, Sueiro A, Diaz G, Escobar C, Garcia-Rull S, Picher J, et al. Prognostic significance of delays in diagnosis of pulmonary embolism. Thrombosis Research 2007; 121: 153-8.
- Timmons S, Kingston M, Hussain M, Kelly H, Liston R. Pulmonary embolism: differences in presentation between older and younger patients. Age and Ageing 2003; 32: 601-5.
- Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ, et al. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2008; 133: 454S-545S.
- Ageno W, Agnelli G, Imberti D, Moia M, Palareti G, Pistelli R, et al. Factors associated with the timing of diagnosis of venous thromboembolism: results from the MASTER registry. Thrombosis Research 2008; 121: 751-6.
- Bulbul Y, Ozsu S, Kosucu P, Oztuna F, Ozlu T, Topbas M. Time delay between onset of symptoms and diagnosis in pulmonary thromboembolism. Respiration; International Review of Thoracic Diseases 2009; 78: 36-41.
- Ozsu S, Oztuna F, Bulbul Y, Topbas M, Ozlu T, Kosucu P, et al. The role of risk factors in delayed diagnosis of pulmonary embolism. Am J Emerg Med 2011; 29: 26-32.
- Alonso-Martinez JL, Sanchez FJ, Echezarreta MA. Delay and misdiagnosis in sub-massive and non-massive acute pulmonary embolism. Eur Int Med 2010; 21: 278-82.
Yaz??ma Adresi (Address for Correspondence):
Dr. Mohammad Hossein Rahimi-rad,
Imam Khomeini Hospital,
Bronchoscopy Unite,
URMIA - IRAN
e-mail: rahimirad@hotmail.com