G?nl?k klinik uygulamada kronik obstr?ktif akci?er hastal???n?n
?iddetinin de?erlendirilmesinde elektrokardiyografinin rol?
Faruk AKT?RK1, ?smail BIYIK1, C?neyt KOCA?2, Mehmet ERT?RK1, Ahmet Arif YAL?IN1,
Ayfer Utku SAVA?3, Firuzan P?nar KUZER3, Fatih UZUN1, Ayd?n YILDIRIM1, Nevzat USLU1,
?a?lar ?UHADARO?LU4
1 SB ?stanbul Mehmet Akif Ersoy G???s Kalp ve Damar Cerrahisi E?itim ve Ara?t?rma Hastanesi,
Kardiyoloji Klini?i, ?stanbul,
2 ?stanbul ?niversitesi Kardiyoloji Enstit?s?, Kardiyoloji Anabilim Dal?, ?stanbul,
3 SB ?stanbul Mehmet Akif Ersoy G???s Kalp ve Damar Cerrahisi E?itim ve Ara?t?rma Hastanesi,
G???s Hastal?klar? Klini?i, ?stanbul,
4 Ac?badem ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?stanbul.
?ZET
G?nl?k klinik uygulamada kronik obstr?ktif akci?er hastal???n?n ?iddetinin de?erlendirilmesinde elektrokardiyografinin rol?
Giri?: Kronik obstr?ktif akci?er hastal??? (KOAH) kronik morbidite ve mortalitenin d?rd?nc? ?nde gelen nedenidir. Bron?iyal obstr?ksiyon ve artm?? pulmoner vask?ler diren? sa? atriyal fonksiyonlar? bozmaktad?r. Bu ?al??mada, KOAH hastalar?nda bron?iyal obstr?ksiyonun p dalga aks? ?zerine olan etkisini ve KOAH ?iddetini de?erlendirmede elektrokardiyografi (EKG)'nin yararl?l???n? ara?t?rmay? ama?lad?k.
Hastalar ve Metod: Doksan be? hasta (64'? erkek, 31'i kad?n) ?al??maya dahil edildi. Hastalar sin?s ritminde, normal ejeksiyon fraksiyonuna ve normal kalp bo?luk boyutlar?na sahipti. Hastalar?n solunum fonksiyon testleri ve 12 derivasyonlu elektrokardiyogramlar? ayn? g?n elde edildi. KOAH ?iddeti ile p dalga aks?, p dalga s?resi, QRS aks? ve QRS s?resini i?eren EKG bulgular? aras?ndaki ili?kiler ara?t?r?ld?.
Bulgular: Ortalama ya? 58 ? 12 y?l idi. Ortalama p dalga aks? 62 ? 18 derece idi. Bu ?al??mada, p dalga aks?, KOAH evreleri ve QRS aks? ile anlaml? pozitif korelasyonlar, fakat FEV1, FEF, BMI ve QRS s?resi aras?nda anlaml? negatif korelasyonlar ortaya koydu. KOAH evreleri artt?k?a p dalga aks? artmaktad?r.
Sonu?: Frontal p dalga aks?n?n vertikalizasyonu, p pulmonale gibi sa? kalp bo?luklar?n?n geni?lemesi ve hipertrofisinin di?er EKG de?i?ikliklerinin olu?mas?ndan ?nce KOAH'?n k?t?le?mesinin erken bir bulgusu olabilir. Sa? atriyal elektriksel aktiviteyi ve sa? kalp y?klenmesini yans?tan frontal p dalga aks?n?n vertikalizasyonu h?zl? hasta bak?lan poliklinik ortam?nda KOAH ?iddetinin ?abuk bir ?ekilde de?erlendirilmesinde yararl? bir parametre olabilir.
Anahtar Kelimeler: P dalga aks?, KOAH, spirometri, EKG.
SUMMARY
The role of electrocardiography in evaluation of severity of chronic obstructive pulmonary disease in daily clinical practice
Faruk AKT?RK1, ?smail BIYIK1, C?neyt KOCA?2, Mehmet ERT?RK1, Ahmet Arif YAL?IN1,
Ayfer Utku SAVA?3, Firuzan P?nar KUZER3, Fatih UZUN1, Ayd?n YILDIRIM1, Nevzat USLU1,
?a?lar ?UHADARO?LU4
1 Clinic of Cardiology, Istanbul Mehmet Akif Ersoy Chest and Cardiovascular Surgery Training and
Research Hospital, Istanbul, Turkey,
2 Department of Cardiology, Istanbul University Cardiology Institute, Istanbul, Turkey,
3 Clinic of Chest Diseases, Istanbul Mehmet Akif Ersoy Chest and Cardiovascular Surgery Training and
Research Hospital, Istanbul, Turkey,
4 Department of Chest Diseases, Faculty of Medicine, Acibadem University, Istanbul, Turkey.
Introduction: Chronic obstructive pulmonary disease (COPD) is the fourth leading cause of chronic morbidity and mortality. Bronchial obstruction and increased pulmonary vascular resistance impairs right atrial functions. In this study, we aimed to investigate the effect of bronchial obstruction on p wave axis in patients with COPD and usefulness of electrocardiography (ECG) in the evaluation of the severity of COPD.
Patients and Methods: Ninety five patients (64 male and 31 female) included to the study. Patients were in sinus rhythm, with normal ejection fraction and heart chamber sizes. Their respiratory function tests and 12 lead electrocardiograms were obtained at same day. Correlations with severity of COPD and ECG findings including p wave axis, p wave duration, QRS axis, QRS duration were studied.
Results: The mean age was 58 ? 12 years. Their mean p wave axis was 62 ? 18 degrees. In this study, p wave axis has demonstrated significant positive correlations with stages of COPD and QRS axis but significant negative correlations with FEV1, FEF, BMI and QRS duration. P wave axis increases with increasing stages of COPD.
Conclusion: Verticalization of the frontal p wave axis may be an early finding of worsening of COPD before occurrences of other ECG changes of hypertrophy and enlargement of right heart chambers such as p pulmonale. Verticalization of the frontal p wave axis reflecting right atrial electrical activity and right heart strain may be a useful parameter for quick estimation of the severity of COPD in an out-patient cared.
Key Words: P wave axis, COPD, spirometry, ECG.
Tuberk Toraks 2013; 61(1): 38-42 • doi: 10.5578/tt.4101
Geli? Tarihi/Received: 25/05/2012 - Kabul Edili? Tarihi/Accepted: 19/12/2012
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a growing major public health problem. In 2020, COPD is projected to rank fifth worldwide in burden of disease, according to a study published by the World Bank/World Health Organization (1). Although COPD has received increasing attention from the medical community in recent years, it is still relatively unknown or ignored by the public as well as public health and government officials (2). In the United States, morbidity caused by COPD is approximately 4%, thus, COPD is ranked as the fourth leading cause of chronic morbidity and mortality after heart attacks, malignancies and strokes (3). COPD, leading reduced lung function, is a strong risk factor for cardiovascular events. COPD and heart diseases often co-exists. Therefore, in daily clinical practice, cardiologists frequently come across patients with COPD. Increased bronchial obstruction and increased pulmonary vascular resistance impairs right atrial functions. In this study, we aimed to investigate the effect of bronchial obstruction on P wave axis in patients with COPD and usefulness of electrocardiography (ECG) findings in the evaluation of severity of COPD classified by spirometry according to the updated new GOLD guidelines (2).
PATIENTS and METHODS
According to Global Initiative for Chronic Obstructive Lung Disease (GOLD) guideline, patients having the diagnosis of COPD were considered for the study (2). Patients who accepted to join in the study were informed about the purpose and methods of study and informed consent was obtained. Patients were in sinus rhythm on ECG and with normal ejection fraction and without significant heart valve disease; chamber dilatation and hypertrophy on echocardiography were included in this study. Patients having known congenital or acquired heart disease, hypertension, coronary artery disease, diabetes mellitus, renal or hepatic disease were excluded from this study. Patients meeting above inclusion and exclusion criteria were selected for the study. Twelve lead ECG and afterwards pulmonary function test according to GOLD spirometry guideline? were performed at the same day (4). Classification of severity of air flow limitation in COPD was made according to GOLD classification based on post-bronchodilator FEV1 (2). Electrocardiographic recordings were performed using General Electric MC 1600 ECG device (Chicago, IL, USA). The values of P wave axis, P wave duration, QRS axis and QRS duration are obtained from the computerized report on electrocardiogram. Correlations between the severity of COPD and ECG findings including P wave axis, P wave duration, QRS axis, QRS duration were studied.
Statistical Analysis
Values were given as mean ? SD. Comparisons of continuous variables between groups were made by Kruskal Wallis variance analysis test. Differences between groups were compared by Mann-Whitney U test. Analyses of categorical variables were made by Chi-square test. Associations between variables were analyzed by Spearman's Rho Correlation test. A p-value < 0.05 was accepted as the level of significance. The level of significance for pairwise comparisons was adjusted when multiple comparisons were performed (p< 0.05/2 = 0.025). Statistical analysis were made by SPSS software (Version 17.0, SPSS Inc, Chicago, IL, USA).
RESULTS
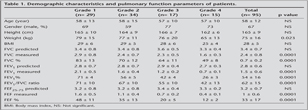
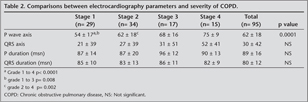
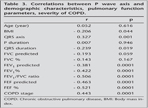
Ninety five patients (64 male and 31 female) included to the study. The mean age was 58 ? 12 years. Their mean P wave axis was 62 ? 18 degrees. Demographic characteristics and pulmonary function parameters of patients have been shown in Table 1. In our findings, P wave axis has showed significant positive correlations with grades of COPD. P wave axis increases with increasing stages of COPD. However, the severity of COPD has showed no significant correlation with P wave duration, QRS axis and QRS duration. Comparisons between ECG parameters and severity of COPD have been indicated in Table 2. In this study, P wave axis has demonstrated significant positive correlations with stages of COPD and QRS axis but significant negative correlations with FEV1, FEF, BMI and QRS duration. Correlations between P wave axis and demographic characteristics, pulmonary function parameters and COPD grade have been displayed in Table 3.
DISCUSSION
In this study, P wave axis has demonstrated statistically significant negative correlations with forced expiratory volume 1, forced expiratory flow, FEV1/FVC ratio, BMI and QRS duration. P wave axis has also had significant positive correlations with stages of COPD, which means that P wave axis increases with increasing stages of COPD. Higher degrees of P wave axis might point out higher stages of COPD. COPD has long been associated with verticalization of the frontal P axis (5). A vertical P wave axis (> 60?) could be used as a screening tool for obstructive pulmonary disease with 89% sensitivity and 96% specificity (6). Not too long ago, researchers pointed that the increasing verticality of P wave axis had a direct correlation with increasing degrees of airway obstruction (7). Bazuaye et al. reported that there was an inverse relationship between mean P wave axis and the FEV1 of predicted in Nigerians with COPD (8). Recently, Rachaiah and colleagues study, the P wave axis +90 degrees and above has been found to be associated with advanced airway obstruction (9). Similarly, the Thomas et al. study has reported that the P wave axis at > 60 degrees can be used alone with very high sensitivity (96%) and specificity (87%) to detect emphysema (10). Our results confirm these previous studies in patients with COPD classified by spirometry according to the updated new GOLD guidelines (2). One of the possible mechanisms of P wave axis verticalization in COPD patients is that the right atrium is tightly connected to the diaphragm via a pericardial ligament near the inferior vena cava (11). Thus, the right atrium will be inferiorly displaced by increasing flattening of the diaphragm (10). Our study reveals that increasing verticality of mean P wave axis is associated with increasing degree of disease severity.
In daily clinical practice, the evaluation of COPD patients with echocardiography may have some limitations. The absence of tricuspid regurgitation and right ventricular hypertrophy or dilatation may cause underestimation of severity of COPD by cardiologists. Transthoracic echocardiography, furthermore, may be impeded by poor visualization of acoustic echocardiography windows caused by the pathological changes associated with COPD. The inadequate visualization of echocardiography views may be related to air trapping. In fact, it has been reported that echocardiographic images were unsatisfactory in 10.4% of patients with COPD and this proportion increases to 35% in patients with severe COPD and to 50% in those with very severe airflow obstruction (12,13). In daily clinical practice, the ECG obtained easily in patients with COPD may give valuable clues in management of COPD.
However, our study has some limitations;
1. If healthy controls were included in this study, the changes of p wave axis could have been more clearly revealed.
2. The number of patients for each subgroup is not sufficient to give a cut off value of P wave axis.
3. Not Rated effective COPD treatment is the effect on P wave axis seems to be a limitation. In fact, it has been reported that effective treatment of COPD might alter the electrocardiographic changes in this disease (14). Verticalization of frontal P-wave axis may be an early sign of worsening of COPD, occurring prior to the onset of electrocardiographic findings such as P-pulmonale and right ventricular hypertrophy. Although the overlap of P wave axis values among groups makes it difficult to determine the severity of COPD simply by ECG, verticalization of frontal P-wave axis, which reflects right atrial electrical activity and strain, can be a useful contributor for the fast prediction of the severity of COPD in an out-patient cared to make a rough assessment.
Verticalization of the frontal P wave axis may be an early finding of worsening of COPD before occurrences of other ECG changes of hypertrophy and enlargement of right heart chambers such as p pulmonale. Verticalization of the frontal P wave axis reflecting right atrial electrical activity and right heart strain on ECG may be a useful parameter for quick estimation of the severity of COPD.
CONFLICT of INTEREST
None declared.
REFERENCES
- World Health Report, Geneva: World Health Organization. Available from URL: http://www.who.int/whr/en/statistics.htm; 2000
- From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2010. Available from: http://www.goldcopd.org/
- Hurd S. The impact of COPD on lung health worldwide: epidemiology and incidence. Chest 2000; 117: 1-4.
- Spirometry for Health Care Providers. Global Initiative for Chronic Obstructive Lung Disease (GOLD) Updated 2010. Available from: http://www.goldcopd.org/
- Spodick DH. Electrocardiographic studies in pulmonary disease: I. Electrocardiographic abnormalities in diffuse lung disease, II. Establishment of criteria for electrocardiographic interference of diffuse lung disease. Circulation 1959; 20: 1067-74.
- Zambrano SS, Moussave MS, Spodick DH. QRS duration in chronic obstructive lung disease. J Electrocardiograph 1974; 7: 35-6.
- Spodich DH, Hauger-Klevene JH, Tyler MJ. The electrocardiogram in pulmonary emphysema: relationship of characteristic electrocardiographic findings to severity of disease as measured by the degree of airway obstruction. Am Rev Respir Dis 1963; 88: 14-9.
- Bazuaye EA, Obasohan AO, Jarikre LN, Onadeko BO. Relationship of the ECG with ventilatory function tests in chronic obstructive lung disease (COLD) in Nigerians. Afr J Med Med Sci 1997; 26: 111-4.
- Rachaiah MM, Rachaiah JM, Krishnaswamy RB. A correlative study of spirometric parameters and ECG changes in patients with chronic obstructive pulmonary disease. Int J Biol Med Res 2012; 3: 1322-6.
- Thomas AJ, Apiyasawat S, Spodick DH. Electrocardiographic detection of emphysema. Am J Cardiol 2011; 107: 1090-2.
- Shah NS, Koller SM, Janover ML, Spodick DH. Diaphragm levels of determinants of p axis in restrictive versus obstructive pulmonary disease. Chest 1995; 107: 697-700.
- Boussuges A, Pinet C, Molenat F, Burnet H, Ambrosi P, Badier M, et al. Left atrial and ventricular filling in chronic obstructive pulmonary disease. An echocardiographic and Doppler study. Am J Respir Crit Care Med 2000; 162: 670-5.
- Hawkins NM, Petrie MC, Jhund PS, Chalmers GW, Dunn FG, McMurray JJV. Heart failure and chronic obstructive pulmonary disease: diagnostic pitfalls and epidemiology. Eur J Heart Fail 2009; 11: 130-9.
- Asad N, Johnson VMP, Spodick DH. Acute right atrial strain. Regression in normal as well as abnormal p-wave amplitudes with treatment of obstructive pulmonary disease. Chest 2003; 124: 560-4.
Yaz??ma Adresi (Address for Correspondence):
Dr. Faruk AKT?RK,
SB ?stanbul Mehmet Akif Ersoy
G???s Kalp ve Damar Cerrahisi
E?itim ve Ara?t?rma Hastanesi,
Kardiyoloji Klini?i,
?STANBUL - TURKEY
e-mail: farukakturk@gmail.com