Akci?er kanserli hastalarda mekik y?r?me testi ile de?erlendirilen egzersiz kapasitesi
postoperatif komplikasyon geli?imini ?ng?rebilir mi?
Yurdanur ERDO?AN1, Ersin G?NAY2, P?nar ERG?N3, Dicle KAYMAZ3, G?ktan TEM?Z4,
Nurettin KARAO?LANO?LU4
1 SB Ankara Atat?rk G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi,
7. G???s Hastal?klar? Klini?i, Ankara,
2 Afyon Kocatepe ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Afyonkarahisar,
3 SB Atat?rk G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, Evde Bak?m ve
Solunum Rehabilitasyon ?nitesi, Ankara,
4 SB Ankara Atat?rk G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi,
G???s Cerrahisi Klini?i, Ankara.
?ZET
Akci?er kanserli hastalarda mekik y?r?me testi ile de?erlendirilen egzersiz kapasitesi
postoperatif komplikasyon geli?imini ?ng?rebilir mi?
Giri?: ?al??mam?z?n amac?, akci?er kanseri rezeksiyon cerrahisinde postoperatif komplikasyon geli?iminde mekik y?r?me testinin rol?n? ara?t?rmakt?r.
Hastalar ve Metod: Erken evre akci?er kanseri tan?s? ile akci?er rezeksiyon cerrahisi i?in aday olan hastalar bu ?al??maya dahil edildi. ?al??maya kat?lan t?m hastalara egzersiz kapasitesinin de?erlendirilmesi i?in mekik y?r?me testi uyguland?.
Bulgular: ?al??maya 24 hasta dahil edildi. Ya? ortalamas? 46 ? 8.6 y?l idi. Pn?monektomi, lobektomi, bilobektomi ve wedge rezeksiyon s?ras?yla 11 (%46), 10 (%42), 2 (%8) ve 1 (%4) hastaya uyguland?. Postoperatif komplikasyon sadece alt? hastada geli?ti. Postoperatif komplikasyon geli?me riski ile ya?, artan h?zda mekik y?r?me testi, end?rans mekik y?r?me testi ve ak?m VO2 (mL/kg/dakika) ile de?erlendirilen egzersiz kapasitesi aras?nda istatistiksel olarak anlaml? bir ili?ki saptanmad? (p> 0.05).
Sonu?: Mekik y?r?me testleri (artan h?zda ve end?rans) akci?er kanseri rezeksiyonlar?nda postoperatif komplikasyonlar? ?ng?rmede s?n?rl? role sahiptir.
Anahtar Kelimeler: Egzersiz kapasitesi, akci?er kanseri, postoperatif komplikasyon, rezeksiyon, mekik y?r?me testi.
SUMMARY
Can exercise capacity assessed by the shuttle walk test predict the development of post-operative complications in patients with lung cancer?
Yurdanur ERDO?AN1, Ersin G?NAY2, P?nar ERG?N3, Dicle KAYMAZ3, G?ktan TEM?Z4,
Nurettin KARAO?LANO?LU4
1 Clinic of 7th Chest Diseases, Ataturk Chest Diseases and Chest Surgery Training and
Research Hospital, Ankara, Turkey,
2 Department of Chest Diseases, Faculty of Medicine, Afyon Kocatepe University, Afyonkarahisar, Turkey,
3 Home Care and Pulmonary Rehabilitation Unit, Ataturk Chest Diseases and Chest Surgery Training and
Research Hospital, Ankara, Turkey,
4 Clinic of Chest Surgery, Ataturk Chest Diseases and Chest Surgery Training and Research Hospital,
Ankara, Turkey.
Introduction: The objective of this study was to assess the role of shuttle walk test in predicting post-operative complications in lung cancer resection surgery.
Patients and Methods: A consecutive series of patients who were candidate for lung resection surgery with the diagnosis of early stage lung cancer were included to this study. All patients in this study evaluated for exercise capacity testing with shuttle walk test.
Results: Twenty for patients were included in this study. Mean age was 61.5 ? 8.6 years. Pneumonectomy, lobectomy, bilobectomy and wedge resection were performed in 11 (46%), 10 (42%), 2 (8%), and 1 (4%) patients, respectively. Complications occurred only in six patients. There was no statistically significant relationship between risk for development of post-operative complication and age, incremental shuttle walk test, endurance shuttle walk test and exercise capacity evaluated with peak VO2 (mL/kg/minute) (p> 0.05).
Conclusion: Shuttle walk tests (incremental and enduronce) had a limited role in predicting post-operative complications in lung cancer resections.
Key Words: Exercise capacity, lung cancer, post-operative complication, resection, shuttle walk test.
Tuberk Toraks 2013; 61(1): 28-32 • doi: 10.5578/tt.3624
Geli? Tarihi/Received: 30/03/2012 - Kabul Edili? Tarihi/Accepted: 12/12/2012
Introduction
Though surgery remains the treatment of choice for resectable lung carcinoma, postoperative complications of lung resection appear to be a major problem especially in patients with co-existing disease (1). Incidence of postoperative complications after lung resection was reported as 24-48% while the mortality rates of lobectomy and pneumonectomy were 4% and 14%, respectively (1,2). The most common complications and the main determinant of mortality and morbidity after lung resection are cardiopulmonary complications (2,3). Preoperative exercise capacity is an independent predictor of peri-operative risks in lung resection surgery so in order to assist the prediction of surgical outcome, a number of exercise tests have been used (1,2,3).
In this study we investigated the relationship between exercise capacity assessed by shuttle walk test (SWT) and development of post-operative complication in patients who were candidate for lung cancer surgery.
PATIENTS and Methods
This study was performed in Home Care and Pulmonary Rehabilitation Unit with Chest Surgery Clinic in Ataturk Chest Diseases and Chest Surgery Training and Research Hospital between December 2007 and October 2008. Twenty-four consecutive patients who were candidate for lung resection surgery with the diagnosis of early stage lung cancer were included to this study. Pulmonary function test was performed for all patients. For evaluation of exercise capacity of these patients, field tests [Incremental Shuttle Walking Test (ISWT) and Endurance Shuttle Walking Test (ESWT)] were used. Peak VO2 was calculated with a formulation of [4.19 + (walking distance x 0.025)] (mL?min-1?kg-1) (4,5,6).
Exclusion criteria included recent myocardial infarction (within six weeks), unstable angina pectoris and disorders that might influence exercise performance such as back pain.
This study was approved by local ethics committee. Informed consents were obtained from each patient.
Shuttle Walking Test
The incremental shuttle walking test was performed similar to the method established by Singh et al. (5). The patients walked between two cones 10 m apart at an incrementally increasing pace. Each increment was signaled by a fully calibrated audiocassette. The end point was achieved when the patient could no longer maintain the required speed or became too breathless to proceed further or desaturation occurred.
The endurance shuttle walking test was performed similar to the method established by Revill et al. (6). Walking speed was adjusted from the level calculated from the walking distance on ISWT. Patients walked between two cones 10 m apart at this stable pace. Duration of this test was noted as endurance time (min).
Complications
Complications were defined as post-operative when they occurred within 30 days after resection.
These post-operative complications were defined as:
1. Prolonged mechanical ventilation (> 48 hour),
2. Hypoxemia,
3. Atelectasis on radiography,
4. Haemoptysis,
5. Empyema,
6. Death caused by respiratory insufficiency or heart failure.
Statistical Approach
Statistical analyses were performed using the SPSS 17.0 Base System and advanced statistics programs (SPSS, Chicago, IL, USA). Descriptive statistics were performed for all the recorded variables. The Pearson's correlation was used to find a correlation between post-operative complications and other study parameters. Threshold for statistical significance was set at 0.05.
Results
One (4%) female and 23 (96%) male patients were included in this study with age range from 43 to 75. Mean age was 61.5 ? 8.6 years. All of the patients were smoker. Mean value for cigarette usage was 50.5 ? 25.9 pack-year. There were only 10 patients (42%) with concomitant COPD. Pneumonectomy, lobectomy, bilobectomy and wedge resection were performed in 11 (46%), 10 (42%), 2 (8%), and 1 (4%) patients, respectively. Complications occurred only in 6 (25%) patients. There was no prolonged mechanical ventilation as postoperative complication. Demographic characteristics, pulmonary function test results, types of lung resection, complications, hospital stay data of 24 patients participated in this study are given in Table 1.
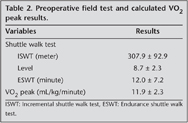
Shuttle walking test results (ISWT, ESWT, level) and calculated peak VO2 are given in Table 2.
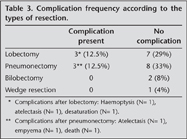
There was no statistically significant relationship between post-operative complication risk and age, amount of cigarette usage (pack-year), ISWT (meter), ESWT (minute), exercise capacity evaluated with peak VO2 (mL/kg/minute), FEV1 (L), FEV1 (%) and presence of COPD as a concomitant disease (p> 0.05). There was a statistically significant relationship between FEV1 (L) and ISWT (meter) (p= 0.007, r = 0.534) and VO2 peak (p= 0.007, r = 0.534). There was no statistical relationship between type of resection and post-operative complications (Table 3).
ISWT (m), ESWT, VO2 peak and FEV1 (L) and FEV1 (%) values was not decisive in the development of complications depending on the type of resection (lobectomy or pneumonectomy).
When the border of FEV1 (L) is taken 1.5 L and 2 L for lobectomy and pneumonectomy, respectively, and peak VO2 is taken 10 mL/kg/minute for all types of resection, these cut-off values and the type of resection did not have the effect for predicting complications.
Discussion
The relationship between postoperative complications and patient-related risk factors (cigarette smoking and advanced age) is not clearly demonstrated (1,2,3). Similar to previous reports, in our study, no relationship between development of postoperative complication and patient-related risk factors (age and smoking) was observed. It has been reported in previous studies that presence of COPD as a concomitant pulmonary disease have an important protective role in the development of post-operative pulmonary complications in lung resection surgery (7,8,9). In this study, we also did not observe any relationship between post-operative complications and presence of COPD as a concomitant disease in lung cancer patients.
To date, in the studies a correlation between the resection width and postoperative mortality and morbidity is reported. While segmental or "wedge" resections are carrying a low risk for developing post-operative complications, pneumonectomy has been reported to have the highest risk (3,8,9,10). In our study, no relationship was determined between types of resection and the development of post-operative complications.
Due to FEV1 % or measured absolute value (L) in preoperative pulmonary function tests is meaningful and easy method for the prediction of postoperative complications; it is implemented as a first step test (1,3). Also, calculation of predicted post-operative FEV1 via ventilation and perfusion scintigraphy or segment formula has important role in predicting complications. In our study, pre-operative FEV1 in predicting postoperative complications of global assessment of all types of resections was not effective. Additionally, it was not effective for comparison of the cut-off levels of preoperative FEV1 as 2 L for pneumonectomy and 1.5 L for lobectomy.
In order to assess functional capacity, maximal exercise testing [cardiopulmonary exercise testing and the ISWT and submaximal exercise tests (6MWT, stair-climbing tests)] can be used (11,12,13,14).
In some studies, although concordant relationship between cardiopulmonary exercise test results (measurement of maximal oxygen uptake) and predicted post-operative pulmonary complications have been reported, the controversial reports in the publications are also available (2,3,7,15). However, in our study, peak VO2 calculated via the walking distance of the ISWT was used for the evaluation of maximal exercise capacity and no effect in predicting for post-operative complications for resection surgery could be found.
There is evidence that tests such as the modified shuttle walk test, Cooper walk run test, and the multi-stage shuttle run test correlate better with oxygen consumption than the shuttle walk test (16,17,18). However, these procedures require vigorous exercise and, as such, would be inappropriate to perform in our patient population who are elderly. Another walk test often used is the six minute walk test. However, interpretation of the distance walked in six minutes is currently not well standardized (19). The SWT has been shown to be reproducible and a good predictor of the impact of breathlessness on functional capacity in patients with cancer (20). We therefore chose to perform the SWT as a reliable field test on our patients.
ISWT in preoperative evaluation of lung cancer was suggested to be used (7,12). Although the literature suggests the increased risk for postoperative complications in patients of which walking distance was shorter than 250 m, there are conflicting studies indicating the SWT as inadequate to predict complications (12).
Our study also did not demonstrate any benefit of ISWT in predicting the development of perioperative complications. Moreover, taking the cut-off for the walking distance as 250 m was not effective in predicting the development of complications.
Although there are some restrictions such as limited number of patients, nonhomogeneous distribution of types of resection, and participation of only one female patient, this is the first study evaluating the availability of ISWT in prediction of post-operative complications in patients candidate for resection surgery for lung cancer in our country population.
As a result, ISWT and ESWT had a limited role in predicting post-operative complications for patients candidate for resection surgery for lung cancer. Further investigations with wider series are warranted to determine availability of ISWT for predicting post-operative cardiopulmonary complications, especially in centers that cardiopulmonary exercise testing is not applicable.
Conflict of interest
None declared.
REFERENCES
- Beckles MA, Spiro SG, Colice GL, Rudd RM; American College of Chest Physicians. The physiologic evaluation of patients with lung cancer being considered for resectional surgery. Chest 2003; 123 (1 Suppl):S105-S14.
- Richter Larsen K, Svendsen UG, Milman N, Brenoe J, Petersen BN. Exercise testing in the preoperative evaluation of patients with bronchogenic carcinoma. Eur Respir J 1997; 10: 1559-65.
- Colice GL, Shafazand S, Griffin JP, Keenan R, Bolliger CT; American College of Chest Physicians. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: ACCP evidenced-based clinical practice guidelines (2nd ed). Chest 2007; 132 (3 Suppl): S161-S77.
- Singh SJ, Morgan MD, Hardman AE, Rowe C, Bardsley PA. Comparison of oxygen uptake during a conventional treadmill test and the shuttle walking test in chronic airflow limitation. Eur Respir J 1994; 7: 2016-20.
- Singh SJ, Morgan MD, Scott S, Walters D, Hardman AE. Development of a shuttle walking test of disability in patients with chronic airways obstruction. Thorax 1992; 47: 1019-24.
- Revill SM, Morgan MD, Singh SJ, Williams J, Hardman AE. The endurance shuttle walk: a new field test for the assessment of endurance capacity in chronic obstructive pulmonary disease. Thorax 1999; 54: 213-22.
- Brunelli A, Salati M. Preoperative evaluation of lung cancer: predicting the impact of surgery on physiology and quality of life. Curr Opin Pulm Med 2008; 14: 275-81.
- Brunelli A, Refai M, Xiume F, Salati M, Marasco R, Sciarra V, et al. Evaluation of expiratory volume, diffusion capacity and exercise tolerance following volume, diffusion capacity and exercise tolerance following major lung resection: a prospective follow-up analysis. Chest 2007; 131: 141-7.
- Varela G, Brunelli A, Rocco G, Marasco R, Jimenez MF, Sciarra V, et al. Predicted versus observed FEV1 in the immediate postoperative period after pulmonary lobectomy. Eur J Cardiothorac Surg 2006; 30: 644-8.
- Villani F, De Maria P, Busia A. Exercise testing as a predictor of surgical risk after pneumonectomy for bronchogenic carcinoma. Respir Med 2003; 97: 1296-8.
- Girish M, Trayner E Jr, Dammann O, Pinto-Plata V, Celli B. Symptom-limited stair climbing as a predictor of postoperative cardiopulmonary complications after high-risk surgery. Chest 2001; 120: 1147-51.
- Win T, Jackson A, Groves AM, Sharples LD, Charman SC, Laroche CM. Comparison of shuttle walk with measured peak oxygen consumption in patients with operable lung cancer. Thorax 2006; 61: 57-60.
- Colman NC, Schraufnagel DE, Rivington RN, Pardy RL. Exercise testing in evaluation of patients for lung resection. Am Rev Respir Dis 1982; 125: 604-6.
- Markos J, Mullan BP, Hillman DR, Musk AW, Antico VF, Lovegrove FT, Carter MJ, Finucane KE. Preoperative assessment as a predictor of mortality and morbidity after lung resection. Am Rev Respir Dis 1989; 139: 902-10.
- Bolliger CT, Jordan P, Soler M, Stulz P, Gradel E, Skarvan K, et al. Exercise capacity as a predictor of postoperative complications in lung resection candidates. Am J Respir Crit Care Med 1995; 151: 1472-80.
- Bradley J, Howard J, Wallace E, Elborn S. Reliability, repeatability and sensitivity of the modified shuttle test in adult cystic fibrosis. Chest 2000; 117: 1666-71.
- Grant S, Corbett K, Amjad AM, Wilson J, Aitchison T. A comparison of methods of predicting maximum oxygen uptake. Br J Sports Med 1995; 29: 147-52.
- Leger LA, Lambert J. A maximal multistage 20-m shuttle run test to predict VO2 max. Eur J Appl Physiol 1982; 49: 1-12.
- American Thoracic Society. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med 2002; 166: 111-7.
- Booth S, Adams L. The shuttle walking test: a reproducible method for evaluating the impact of shortness of breath on functional capacity in patients with advanced cancer. Thorax 2001; 56: 146-50.
Yaz??ma Adresi (Address for Correspondence):
Dr. Ersin G?NAY,
Afyon Kocatepe ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
AFYONKARAH?SAR - TURKEY
e-mail: ersingunay@gmail.com