Obstr?ktif uyku apne olgular?nda pozitif hava yolu bas?nc? tedavisine
erken yan?t?n de?erlendirilmesi: Tedavinin ya?am kalitesi ?zerine etkisi
?irin YURTLU, Nesrin SARIMAN, Ender LEVENT, Ak?n Cem SOYLU, S?meyye ALPARSLAN, Attila SAYGI
Maltepe ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, ?stanbul.
?ZET
Obstr?ktif uyku apne olgular?nda pozitif hava yolu bas?nc? tedavisine erken yan?t?n de?erlendirilmesi: Tedavinin ya?am kalitesi ?zerine etkisi
Giri?: ?al??mam?zda; obstr?ktif uyku apne (OSA) tan?s?yla pozitif hava yolu bas?nc? (PAP) tedavisi planlanan hastalar?n Calgary uyku apne ya?am kalitesi indeksi [Calgary Sleep Apnea Quality of Life Index (SAQLI)], Epworth uykululuk ?l?e?i (EU?) ve obstr?ktif uyku apne sendromu (OSAS) semptom sorgu anketini kullanarak tedavi uyumunu de?erlendirmeyi ve tedavinin ya?am kalitesi ?zerine erken d?nem etkilerini ara?t?rmay? planlad?k.
Hastalar ve Metod: ?niversite hastanesi Uyku Laboratuvar?nda; uyku ile ilgili yak?nmalar? nedeniyle poliklini?imize ba?vuran ve polisomnografi testi uygulanarak OSA tan?s? alm??, PAP cihaz?yla devaml? PAP tedavisi planlanan, ?al??maya kat?lmay? kabul eden eri?kin toplam 30 hasta (23'? erkek, 7'si kad?n) ?al??maya dahil edildi. T?m olgulardan yaz?l? onam al?nd?.
Bulgular: Olgular?n genel verileri, OSAS semptomlar?, EU? skorlar? ve SAQLI de?erleri kaydedildi. Bir ay sonra yap?lan ikinci g?r??mede EU?, SAQLI ve OSAS semptom sorgulamalar? yenilenerek hastalar?n kazan?mlar? de?erlendirildi. ?al??maya al?nan t?m hastalar?n bir ay s?resince gece uyku boyunca cihaz? kulland?klar? saptand?. OSA olgular?nda PAP tedavisi ile "g?nd?z a??r? uykululuk hali"nde, "semptom sorgulama anketi" ve "Calgary ya?am kalitesi anketi" puanlar?nda anlaml? iyile?meler (p< 0.001) elde edildi. Apne hipopne indeksi puan?yla tedavi sonucu elde edilen duygu durum de?i?iklikleri aras?nda anlaml? ili?ki bulundu (r= -0.374, p= 0.045).
Sonu?: OSA olgular?n?n erken d?nemde PAP tedavisinden kayda de?er fayda sa?layabilece?i saptanm??t?r. Bu ?al??ma, hastalar?n hastal?klar?yla ilgili fark?ndal?klar?n?n artmas?n? ve tedavi s?resince tedavi kazan?mlar?n? daha iyi alg?lamalar?n? sa?lam??t?r. OSAS a??rl???n?n tedaviyle elde edilen duygu durum de?i?ikliklerinin belirleyicisi oldu?u ve hastal???n a??rl??? ne kadar fazla ise PAP tedavisiyle duygu durumdaki d?zelmelerin o kadar belirgin oldu?u g?r?lm??t?r.
Anahtar Kelimeler: Hasta uyumu, obstr?ktif uyku apne sendromu, pozitif hava yolu bas?nc? tedavisi, uyku apne ya?am kalitesi indeksi.
SUMMARY
Short-term positive airway pressure therapy response in obstructive sleep apnea patients: impact of treatment on the quality of life
?irin YURTLU, Nesrin SARIMAN, Ender LEVENT, Ak?n Cem SOYLU, S?meyye ALPARSLAN, Attila SAYGI
Department of Chest Diseases, Faculty of Medicine, Maltepe University, Istanbul, Turkey.
Introduction: We aimed to assess the compliance of obstructive sleep apnea (OSA) patients of whom we planned positive airway pressure (PAP) therapy by using "Calgary Sleep Apnea Quality of Life Index (SAQLI)","Epworth Sleepiness Score (ESS)","OSAS Symptoms Questionnaire (OSQ)" and, to investigate the early effects of treatment on the quality of life.
Patients and Methods: A total of 30 adult (male/female: 23/7) OSA patients who applied to Sleep Research Laboratory at the University Hospital, complaining of symptoms related to sleep and polysomnographically verified as OSAS with PAP therapy indications were included to the study. Their written consent were obtained.
Results: Characteristics of the patients, OSAS symptoms, ESS and SAQLI sores were recorded. After a month, on the second visit, ESS, SAQLI and OSAS symptoms questionnaire had been repeated. All the patients have routinely used PAP devices for a period of a month. PAP therapy provided significant improvements in excessive daytime sleepiness, symptoms questionnaire and SAQLI scores (p< 0.001). There was a significant correlation between apnea hypopnea index (AHI) score and the improvements in emotional functioning (r = -0.374, p= 0.045).
Conclusion: We concluded that the OSA patients can have remarkable benefits from PAP therapy during the early treatment period. This study increased the awareness of the patients about their illness and their perceived benefits related to PAP treatment. Emotional functioning improved prominantly as the disease's severity increased.
Key Words: Compliance, obstructive sleep apnea syndrome, positive airway pressure treatment, sleep apnea quality of life index.
Geli? Tarihi/Received: 18/05/2012 - Kabul Edili? Tarihi/Accepted: 20/09/2012
INTRODUCTION
Obstructive sleep apnea syndrome (OSAS) is a disease that necessitates regular and mostly a lifelong therapy. There are still difficulties in diagnosis and treatment although advances have been made in this area. Positive airway pressure (PAP) therapy is the gold standard and the most effective noninvasive treatment modality for OSAS patients. It can lead to a decline in daytime sleepiness and traffic accidents, control hypertension and cardiovascular diseases, improving sleep pattern and emotional functioning can prevent the negative outcomes of the disease (1,2). Many OSAS patients experience compliance problems during therapy. Approximately 15-30% of patients refuse to take PAP therapy from the beginning (before or during titration test) and 25-50% of those who accept the treatment fail to adhere the treatment optimally. In the long term, up to 25% of the patients stop using their devices (3). The problems related to mask and the devices are the mostly encountered complaints of the patients that affect adherence to PAP application (4,5,6). Early pattern of PAP use is critical to determine continued patterns of use. Patient acceptance and adherence to treatment are important factors that may improve treatment outcomes for OSAS.
To our knowledge studies regarding the quality of life, using disease specific questionnaires in Turkish OSA patients are scarce. We aimed to assess short-term PAP therapy response, the effects of treatment on the quality of life and, the compliance problems of OSA patients. Calgary sleep apnea quality of life index (SAQLI) questionnaire was a specifically designed questionnaire to evaluate OSAS patients that enabled us to assess the responses of OSA patients to the treatment (7). Besides SAQLI, Epworth sleepiness score (ESS), and OSAS symptoms questionnaire (OSQ) were also used in the study (8).
PATIENTS and METHODS
A total of 30 adult patients (aged > 18 years; male/female: 23/7) who applied to the sleep research laboratory at Maltepe University respiratory diseases department, between May 2010-May 2011 complaining of symptoms related to sleep and polysomnographically verified as OSA with PAP therapy indications and were included to the study. Eighty-two patients with diagnosis of moderate to severe OSA, of whom we planned PAP therapy, have been informed about the study. Titration PSG was performed within a week after the initial PSG. On the second visit, 30 of 82 patients agreed to participate. All the patients gave their written consent. In the same week,
1. OSAS symptoms questionnaire
2. ESS and
3. SAQLI were performed (7,8,9).
Patients with ESS ≥ 10 were considered having excessive day time sleepiness (8). The exclusion criterias were; significant nasal obstruction precluding PAP use, previous surgical intervention for OSA, taking supplementary oxygen and, severe psychiatric, respiratory and cardiovascular diseases.
Smoking status, accompanying diseases (hypertension, diabetes mellitus, coronary artery disease, bronchial asthma, atopy, chronic obstructive airway disease, gastroesophagial reflux disease) were recorded. Questions about the OSAS symptoms were asked in two different ways: First, questions related to the most frequently encountered 18 OSAS symptoms were evaluated by using OSQ. Secondly, patients were asked to score the questions in part D of SAQLI. After a month on the second visit OSQ, ESS and all domains of SAQLI have been repeated. Patients' symptomatic reports were recorded. SAQLI questionnaire was translated into Turkish and a written consent was obtained from Flemons W.W. to use SAQLI in the present study (7).
Polysomnography
An overnight polysomnographic evaluation with a Compumedics E series sleep system (Compumedics Limited 2004, Australia) was performed in all subjects, according to internationally approved methods. This procedure consisted of polygraphic recordings from surface electrodes for electroencephalography (C3/A2 and O2/A1), electrooculography, electromyography (including the chin and lower-extremity muscles), and electrocardiography and from thermistor for nasal and oral airflow, tracheal sounds (via a microphone), and thoracic and abdominal respiration. Transcutaneous oxygen saturation was measured continuously with a finger-pulse oximeter. Positional changes during sleep were recorded.
During the test period, full-night video recordings were also executed. The test was terminated after final waking in the morning. Data were collected in computerized polysomnography system (ProFusion PSG 2 Software) and scoring was performed manually. One PSG scorer scored all studies.
Sleep was defined according to the criteria of Rechtschaffen and Kales (10). Respiratory events (obstructive, mixed, and central apneas) were scored according to American Academy of Sleep Medicine criteria (9). Hypopnea was defined as a ≥ 50% decrease in airflow that persisted for at least 10 seconds and was accompanied by a decrease of ≥ 3% in oxygen saturation or by EEG-recorded arousal using AASM-Alternate method (11). The apnea-hypopnea index (AHI) was defined as the number of apneic and hypopneic events that occurred per hour of sleep. The AHI, when associated with typical clinical features, was scored as follows: AHI ≥ 5 events per hour were diagnosed as OSAS; 15 ≥ AHI ≥ 5 events per hour; mild, 30 ≥ AHI > 15 events per hour; moderate, and > 30 events per hour; as severe OSA.
PAP therapy indication was determined according to AASM 2007 Report criteria (11). Titration to therapeutic PAP pressure levels was performed by an experienced technologist during a second night PSG. Objective measurements of PAP adherence was assessed by monitoring PAP usage per night using the Respironics Encore software program (Respironics, Murrysville, PA, USA) at the end of the study period (30 days).
Our study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of the Medical Faculty of Maltepe University. All the patients signed approved written consent forms.
Statistical Analysis
NCSS 2007 (Number cruncher statistical system) package programme was used for statistical analysis. T test was used for descriptive statistical methods (mean, standart deviation) and also for comparisons before and after the treatment. Mann-Whitney U test was used for comparison of paired groups. Numerical data were compared by chi-square test. Pearson correlation analysis was used to determine the associations between the variables. Results were considered as significant at a value of p< 0.05.
RESULTS
Of the 30 OSA patients who started PAP therapy after titration test 23 were male and seven were female. The mean age of the patients was 53.07 ? 12.49 years (31-81). Neck circumference measurement was 45.93 ? 5.69 cm (30-57). Sixteen patients had history of cigarette smoking (38.25 ? 39.24 packages/year). The mean hours/night of PAP usage was 5.6 ? 0.5 hours/night.
As accompanying diseases; 18 (60%) had hypertension, 12 (40%) had gastroesophagial reflux disease, 9 (%30) had diabetes mellitus, 6 (20%) had chronic obstructive airway disease, 3 (10%) had bronchial asthma and, 2 (6.9%) had coronary artery disease. The most frequently encountered disease was hypertension.
To assess whether the patients had well understood SAQLI questionnaire questions, a-Cronbach coefficients of reliability were calculated. For SAQLI domains and total SAQLI, Cronbach coefficients of reliability were 0.838 and 0.952 respectively. All the scores were above the acceptable ranges.
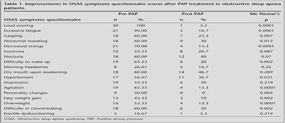
Mean body mass index (BMI) of the patients was 33.13 ? 7.78 kg/m2. There was no statistical difference between the mean body weight of the patients before and after the PAP therapy (p= 0.202). There was a decline in daytime sleepiness and, a statistically significant difference was found in mean ESS score after PAP therapy (10.07 ? 5.92 vs. 6.28 ? 3.58; p= 0.0001). There were statistically significant decreases in the scores of OSAS symptoms questionnaire after PAP therapy (Table 1). Loud snoring (100%) and excessive fatigue (90%) were the mostly encountered symptoms. When asked after PAP therapy; dry mouth (46.7%) and nocturia (40%) were the primary complaints.
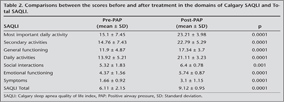
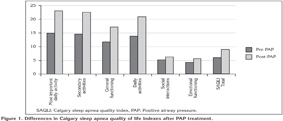
After 30 days of PAP therapy there were statistically significant increases in SAQLI both in domains and total scores. These increases were related with improvements of the symptoms (p= 0.0001) (Table 2) (Figure 1).
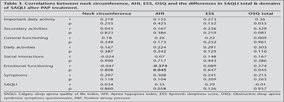
Differences in SAQLI total score and also in domains of SAQLI score related to PAP therapy were calculated. Correlations between the differences of these scores and; neck circumference, AHI, ESS score, OSAS symptoms questionnaire score were evaluated. A negative statistically significant relation between "AHI difference" and "emotional functioning difference" related to PAP therapy was found (r= -0.374, p= 0.045). There were not any statistical significant results in other parameters (p> 0.05) (Table 3).
The primary complaints of the patients before PAP therapy were: hypersomnia and falling asleep at any condition (13.8%), dry mouth upon awakening (13.8%), frequent awakening during the night (13.8%), and episodes of waking at night feeling short of breath or gasping for air. Their secondary complaints were: nocturia (17.2%); and the most frequent third complaint was feeling of restlessness and fatigue upon awakening.
The primary complaints of the patients after PAP therapy were: dry mouth and nasal stuffiness or congestion in the mornings (46.7%). Their secondary complaints were: restlessness and fatigue (13.3%),and frequent awakening during the night (13.3%). The most frequently preferred third answer was:"I have no complaints".
The most frequent complaints related to PAP device were: mask leaks (63.3%), frequent awakening during night sleep (50%), dry mouth and throat upon awakening (46.67%), disturbance due to nasal mask (40%), and redness or irritation where the mask or mask straps touch the skin (40%). None of the patients complained from earache, hoarseness, ache in the chin muscles or toothache.
DISCUSSION
In the present study we assessed the short-term response of OSA patients of whom PAP therapy had been started by using SAQLI as an assessment instrument. There were significant improvements in all parameters of SAQLI, ESS and in most frequently encountered symptoms of OSAS in a treatment period of 30 days.
AHI was a parameter that reflects the severity of the disease. The aim of the therapy was to decrease AHI level successfully from the first night of the titration test. AHI can be titrated to normal levels by continuous and regular use. PAP therapy reduces apneas and hypopneas, improves sleep quality, decreases OSAS symptoms and eliminates daytime sleepiness (4,12,13,14).
Titration test is applied to determine the ideal pressures and type of the devices for the patients. Optimal titration and successful titration defines; AHI as being < 15 for moderate to severe OSAS and achieving a decrease of 50% in AHI for mild OSAS (15). In the present study successful and optimal titration criterias were assessed in all the patients.
In order to evaluate the compliance with PAP therapy and to be sure about an effective treatment duration, the patient has to use the device ≥ 4 hours per night in at least 70% of the scheduled treatment period (13). In general, 15-30% of the patients refuse treatment with PAP devices although they attend the titration test with OSA diagnosis and PAP therapy indication. Unfortunately, 20-25% of those who accept drop out since they claim that they do not have any benefits from the therapy (3,16). This decision negatively affects the success of the treatment. In the present study, adherence to PAP therapy was good. The mean hours/night of PAP usage was 5.6 ? 0.5 hours/night.
Neck circumference being < 37 cm and > 48 cm are found to be related with low and high risk for OSAS, respectively (17). In this study mean value of neck circumference measurements was 45.93 ? 5.69 cm (30-57 cm). About two-thirds of all people with OSAS are overweight or obese (18,19). Pieters et al. reported mean BMI as: 36 ? 6 kg/m2, Engleman et al. as: 33 kg/m2, Kribbs et al as: 39.5 kg/m2 (20). We reported a mean BMI of 33.13 kg/m2 in the present study.
There are studies reporting weight loss during PAP therapy (2). In the present study, follow-up period was short (30 days) therefore we could not find any statistically significant differences with regard to weight loss. Studies with short and long term results, claimed that there was not always a significant weight loss with PAP treatment (21).
OSAS is accepted as an independent risk factor for hypertension (1,22). Approximately 50% of those with sleep apnea have hypertension as an accompanying disease. In this study group similarly, the most frequently encountered accompanying disease was hypertension (60%). Sanner et al. reported hypertension in 50%; Bolitschec et al. in 21.3% of their patients (23,24). OSQ answers of the patients after PAP therapy showed improvements in weight gain and hypertension control (Table 3). We considered that objective comments about the outcomes of the accompanying diseases such as Diabetes Mellitus, obesity, hypertension, asthma and COPD could not be made within such a short period of time. Records of long follow-up periods such as six months to one year should be assessed to critize on marked differences in accompanying diseases.
Excessive daytime sleepiness is one of the cardinal symptoms of OSAS. PAP treatment eliminates daytime sleepiness and decreases ESS scores (24,25). Effective therapy improves sleepiness of both patients' and their bed partners (26,27). We eliminated excessive daytime sleepiness in 66% of the study patients.
In studies concerning compliance with PAP therapy with those patients using their devices regularly, declines in OSA symptoms and excessive daytime sleepiness are used as objective criteria to assess the outcomes (4,13). Regular use of the devices for a period of first three months is proposed as an important marker for long term compliance (15). There are studies showing the positive correlations between the compliance and benefits of the therapy (28-30). Avlonitou concluded that OSAS patients who adhere to nighttime CPAP therapy showed significant improvement of their quality of life, daytime sleepiness, and other symptoms after six months treatment (18). Sanner evaluated the long term effects (nine months) of PAP therapy and concluded that PAP therapy effectively improved the quality of life (23).
Cruz et al. assessed the response to nasal automatic PAP therapy of symptoms like fatigue, gasping, nocturia, nocturnal sweating, morning headaches, heartburn and erectile dysfunctioning after a treatment period of six months. They concluded that OSA patients benefit from PAP therapy in the treatment of wide range of symptoms and the treatment could improve quality of life also in non-sleepy OSA patients (31).
By eliminating snoring, PAP therapy leads to an increase in sleep quality. Symptoms of loud snoring (100%) and uncomfortable sleep (93.1%) declined to 3.3% and 16.7%, respectively. In a study of Meslier et al. including 3225 patients; the most frequent symptoms were snoring, restlessness, excessive daytime sleepiness, and fatigue. Eighty-seven percent of the patients experienced four of those five symptoms (4).
Cognitive disturbances and labile emotional functioning are also consequences of OSAS. They can affect patients' business life, social interactions, psychological health and life quality (15,32). Depression, agitation, disturbances in social relationships can be reversed with PAP treatment (2,33). OSQ answers after PAP therapy revealed statistically significant declines in complaints of agitation, personality changes, and concentrating difficulty.
Compliance increases in patients as the quality of life improves with the treatment (3,22,34). Questionnaires regarding general life quality are insufficient to assess the effects of OSAS and treatment parameters (24,35). We preferred to use SAQLI because it has been prepared specifically to evaluate the life quality of OSAS patients (36,37). In the domains of SAQLI; "secondary activities", "general functioning", "daily activities", "social interactions", "emotional functioning" mean scores were statistically significantly increased (improved) when compared before and after PAP therapy. OSAS patients usually complain about reduction in their daily performances (23). In the first part of SAQLI questionnaire problems with daily activities were evaluated. PAP therapy also provided significant improvements related with daily activities.
In a study investigating effects of PAP therapy 70% of the patients reported that their business life improved by PAP application (4). In "daily activities" section of Calgary SAQLI questionnaire work performance was questioned. We also found significant improvements in work performance of OSA patients as they regularly used their devices. Since PAP therapy leads to a decline in daytime sleepiness by restoring sleep architecture, patients feel energic and can concentrate well at their jobs. This result positively affects their business life.
The differences in SAQLI total score and also in domains of SAQLI score before and after PAP therapy were calculated. When the correlations between the pre-post differences of these scores and; neck circumference, AHI, ESS score, OSQ score were made, we only found a negative statistically significant relation between "AHI difference" and "emotional functioning difference" related to therapy (r= -0.374, p= 0.045). As a result, patients who had high AHI scores (severe disease) showed better responses in emotional functioning. There were significant improvements in emotions such as hopelessness, agitation, fear, irritability and tolerability. Improvements in psychological health increased the awareness of the patients and made them feel better. This result positively affected their life quality.
In the present study the most frequent complaints about PAP application were air leaks from the masks, dry mouth and throat upon awakening, and redness or irritation where the mask or mask straps touched the skin. One-third of the patients's bed partners complained from the noise of the device. It has been suggested not to use PAP devices without humidifiers more than four hours (38). In the study population 28 (98%) patients used humidifiers attached to PAP devices. One-third of the patients had changed their masks during treatment period because they had problems with their masks.
Fleury reported complaints about PAP therapy in 14 of 17 patients. Air humidifier was added in 12 of them and two patients had changed their masks (36). Sanders reported that 85% of OSAS patients using PAP therapy had problems with their masks and experienced nasal symptoms as dryness in the nose (2). Meslier observed that the most frequently encountered symptoms related to the therapy were dry mouth and throat (52.2%), and the noise of the device (47%) (4).
Limitation of the present study was the absence of a control group to compare the changes related to PAP therapy. This necessitated a group of moderate to severe OSA patients without PAP treatment (an untreated group). But we considered it not ethical to postpone the treatment of such patients with high AHI values, symptomatic and PAP therapy indicated.
Close follow-up protocols and informing people with possible side effects before starting therapy are very important to acquire the best adherence to the treatment (14). We propose that when the cases are evaluated as patient-based, compliance problems are detailed and patients are educated about their illness, PAP adherence rates and treatment outcomes will be improved. Positive changes in emotional functioning make patients feel better and the perceived benefits related to therapy can influence the quality of life.
In conclusion; OSA patients can have remarkable benefits from positive airway pressure therapy, even in the early treatment period. The present study increased the awareness of the OSA patients about their illness and their perceived benefits related to positive airway pressure treatment. Improvements related to positive airway therapy in the emotional functioning of OSA patients were more prominant as the severity of the disease increased. This result suggested that the severity of OSA (apnea-hypopnea index) was a determinant of treatment related changes in emotinal functioning. "Calgary sleep apnea quality of life index" questionnnaire can be used as an assessment instrument in the sleep outpatient clinics to evaluate response to the therapy.
AcknowleDgEments
The authors thank Flemons W.W. for the help and permission to use Calgary SAQLI questionnaire in the present study.
CONFLICT of INTEREST
None declared.
REFERENCES
- Bollig SM. Encouraging CPAP adherence: it is everyone's job. Respir Care 2010; 55: 1230-6.
- Giles TL, Lasserson TJ, Smith BH, White J, Wright JJ, Cates CJ. Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 2006; 3: CD001106.
- Olsen S, Smith S, Oei T. Adherence to continuous positive airway pressure therapy in obstructive sleep apnoea sufferers: a theoretical approach to treatment adherence and intervention. Clinical Psychology Review 2008; 28: 1355-71.
- Shapiro GK, Shapiro CM. Factors that influence CPAP adherence: an overview. Sleep Breath 2010; 14: 323-35.
- Sanders MH, Gruendl CA, Rogers RM. Patient compliance with nasal CPAP therapy for sleep apnea. Chest 1986; 90: 330-3.
- Meslier N, Lebrun T, Grillier-Lanoir V, Rolland N, Henderick C, Sailly JC, et al. A French survey of 3.225 patients treated with CPAP for obstructive sleep apnoea: benefits, tolerance, compliance and quality of life. Eur Respir J 1998; 12: 185-92.
- Flemons WW, Reimer MA. Measurement properties of the Calgary Sleep Apnea Quality of Life Index. Am J Respir Crit Care Med 2002; 165: 159-64.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 1991; 14: 540-5.
- Epstein LJ, Kristo D, Strollo PJ, Friedman N, Malhotra A, Patil PS, et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 2009; 5: 263-76.
- Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring system for sleep satges in human subjects. CA: Brain Information Service, Los Angeles, UCLA, 1968.
- Iber C, Ancoli-Israel S, Chesson A, Quan SF. The AASM Manu-al for the scoring of sleep and associated events: rules, terminology and technical specifications. 1st ed. Westchester, IL: American Academy of Sleep Medicine 2007.
- Mc Ardle N, Douglas NJ. Effect of continuous positive airway pressure on sleep architecture in the sleep apnea?hypopnea syndrome. Am J Respir Crit Care Med 2001; 164: 1459-63.
- Sin DD, Mayers I, Man GCW, Ghahary A, Pawluk L. Can positive airway pressure therapy improve the general health status of patients with obstructive sleep apnea? A clinical effectiveness study. Chest 2002; 122: 1679-85.
- Berg S. Obstructive sleep apnoea syndrome: current status. Clin Respir J 2008; 2: 192-201.
- Kushida CA, Chediak A, Berry RB, Brown LK, Gozal D, Iber C, et al. Clinical guideliness for the manual titration of positive airway pressure in patients with obstructive sleep apnea. Positive Airway Pressure Titration Task Force of the American Academy of Sleep Medicine Task Force Members. J Clin Sleep Med 2008; 4: 157-71.
- McArdle N, Devereux G, Heidarnejad H, Engleman HM, Mackay TW, Douglas NJ. Long-term use of CPAP therapy for sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med 1999; 159: 1108-14.
- Mc Nicholas WT. Diagnosis of obstructive sleep apnea in adults. Proc Am Thorac Soc 2008; 5: 154-60.
- Kribbs NB, Pack AI, Kline LR, Smith PL, Schwartz AR, Schubert NM, et al. Objective measurement of patterns of nasal CPAP use by patients with obstructive sleep apnea. Am Rev Respir Dis 1993; 147: 887-95.
- Avlonitou E, Kapsimalis F, Varouchakis G, Varvadas CI, Behrakis P. Adherence to CPAP therapy improves quality of life and reduces symptoms among obstructive sleep apnea syndrome patients. Sleep Breath 2012; 16: 563-9.
- Pieters T, Collard P, Aubert G, Dury M, Delguste P, Rodenstein DO. Acceptance and long-term compliance with nCPAP in patients with obstructive sleep apnoea syndrome. Eur Respir J 1996; 9: 939-44.
- Becker HF, Jerrentrup A, Ploch T, Grote L, Penzel T, Sullivan CE, et al. Effect of nasal continuous positive airway pressure treatment on blood pressure in patients with obstructive sleep apnea. Circulation 2003; 107: 68-73.
- Mc Nicholas WT, Bonsignore MR. Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J 2007; 29: 156-78.
- Sanner BM, Klewer J, Trumm A, Randerath W, Kreuzer I, Zidek W. Long-term treatment with continuous positive airway pressure improves quality of life in obstructive sleep apnoea syndrome. Eur Respir J 2000; 16: 118-22.
- Bolitschek J, Schmeiser-Rieder A, Schobersberger R, Rosenberger A, Kunze M, Aigner K. Impact of nasal continuous positive airway pressure treatment on quality of life in patients with obstructive sleep apnoea. Eur Respir J 1998; 11: 890-4.
- Johns MW. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest 1993; 103: 30-6.
- Mc Nicholas WT. Compliance with nasal CPAP therapy for obstructive sleep apnoea: how much is enough? Eur Respir J 1997; 10: 969-70.
- Ashtyani H, Hutter DA. Collateral damage: the effects of obstructive sleep apnea on bed partners. Chest 2003; 124: 780-1.
- Waldhorn RE, Herrick TW, Nguyen MC, O'Donnell AE, Sodero J, Potolicchio SJ. Long-term compliance with nasal continuous positive airway pressure therapy of obstructive sleep apnea. Chest 1990; 97: 33-8.
- Meurice JC, Dore P, Paquereau J, Neau JP, Ingrand P, Chavagnat JJ, et al. Predictive factors of long-term compliance with nasal continuous positive airway pressure treatment in sleep apnea syndrome. Chest 1994; 105: 429-33.
- Engleman HM, Asgari-Jirhandeh N, McLeod AL, Ramsay CF, Deary IJ, Douglas NJ. Self-reported use of CPAP and benefits of CPAP therapy: a patient survey. Chest 1996; 109: 1470-6.
- Cruz IA, Drummond M, Winck JC. Obstructive sleep apnea symptoms beyond sleepiness and snoring: effects of nasal APAP therapy. Sleep Breath 2012; 16: 361-6.
- Jennum P. Quality of life, co-morbidity and obstructive sleep apnoea. Clin Respir J 2010; 4: 129-30.
- Mun?oz A, Mayoralas LR, Barbe? F, Perica?s J, Agust?? AGN. Long-term effects of CPAP on daytime functioning in patients with sleep apnoea syndrome. Eur Respir J 2000; 15: 676-81.
- Olsen S, Smith S, Oei T, Douglas J. Health belief model predicts adherence to CPAP before experience with CPAP. Eur Respir J 2008; 32: 710-17.
- Young T, Peppard PE, Gottlieb DJ. Epidemiology of obstructive sleep apnea. Am J Respir Crit Care Med 2002; 165: 1217-39.
- Fleury B, Rakotonanahary D, Hausser-Hauw C, Lebeau B, Guilleminault C. Objective patient compliance in long-term use of nCPAP. Eur Respir J 1996; 9: 2356-9.
- Flemons WW, Tsai W. Quality of life consequences of sleep-disordered breathing. J Allergy Clin Immunol 1997; 99: 750-6.
- Akashiba T, Kawahara S, Akahoshi T, Omori C, Saito O, Majima T, et al. Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest 2002; 122: 861-5.
Yaz??ma Adresi (Address for Correspondence):
Dr. Nesrin SARIMAN,
Maltepe ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
Maltepe, ?STANBUL - TURKEY
e-mail: nessariman@yahoo.com