Kronik
obstr?ktif akci?er hastal???nda (KOAH) budesonid/formoterol sabit kombinasyon
kuru toz inhaler i?in kullan?m tekni?inin ve hasta memnuniyetinin
de?erlendirilmesi:
T?rkiye'de g?nl?k klinik uygulama verileri
Can
?ZT?RK1, Ak?n KAYA2, Cahit B?LG?N3, Leyla
Y?CESOY4, Belgin ?K?DA?5, Mustafa DEM?REL6,
?eyma
BA?LILAR7, Beng? ?AYLAN7, Tuncer ?ENOL8, Semih
A?ANO?LU9, Gonca CAN10,
Mustafa Ilgaz DO?RUL11,
Murat ?AM12, Nezaket ERDO?AN13, ?zg?r BATUM14,
Muzaffer Onur TURAN15,
Cahit DEM?R16, ?erife TORUN17,
Murat C?R?T18, Mehmethan TURAN19, Arif KELE?O?LU20,
Sava? YA?AR21, ?znur UZUNAY17, Kevser MELEK22,
Osman ALTIPARMAK23
1 Gazi ?niversitesi T?p Fak?ltesi, Ankara,
2 Ankara ?niversitesi T?p Fak?ltesi, Ankara,
3 SB Hendek Devlet Hastanesi, Sakarya,
4 ?zel IMC Hastanesi, Mersin,?
5 ?zel SEV Amerikan Hastanesi, Gaziantep,
6 Kayseri ?zel Sevgi Hastanesi, Kayseri,
7 SB ?mraniye E?itim ve Ara?t?rma Hastanesi, ?stanbul,
8 ?zel OSM Ortado?u Hastanesi, ?anl?urfa,
9 ?zel ?AR Hastanesi, Rize,
10 Bafra Devlet Hastanesi, Samsun,
11 ?ank?r? Devlet Hastanesi, ?ank?r?,
12 Nazilli Devlet Hastanesi, Ayd?n,?
13 ?zel Adana Ortado?u Hastanesi, Adana,
14 Bart?n Devlet Hastanesi, Bart?n,
15 Bolvadin Dr. Halil ?brahim ?zsoy Devlet Hastanesi, Afyonkarahisar,
16 Elaz?? ?zel Bronko-Med G???s Hastal?klar? Merkezi, Elaz??,
17 SB Beyhekim Devlet Hastanesi, Konya,
18 SB Buca Seyfi Demirsoy Devlet Hastanesi, ?zmir,
19 SB Sorgun Devlet Hastanesi, Yozgat,
20 SB D??kap? Y?ld?r?m Beyaz?t E?itim ve Ara?t?rma Hastanesi, Ankara,
21 SB Konya Numune Hastanesi, Konya,?
22 Kocaeli Derince E?itim ve Ara?t?rma Hastanesi, Kocaeli,?
23 SB Manisa Devlet Hastanesi, Manisa.
?ZET
Kronik obstr?ktif akci?er hastal???nda (KOAH) budesonid/formoterol sabit kombinasyon kuru toz inhaler i?in kullan?m tekni?inin ve hasta memnuniyetinin de?erlendirilmesi: T?rkiye'de g?nl?k klinik uygulama verileri
Giri?: Bu ?al??ma, kronik obstr?ktif akci?er hastal???nda (KOAH) s?kl?kla kullan?lan kuru toz inhalerlere ?zg? hasta uyumunun d?zeyini de?erlendirmek? ve se?ilmi? bir inhaler tipi olarak budesonid/formoterol sabit kombinasyon kuru toz inhaler i?in hasta memnuniyetinin ve inhaler kullan?m tekni?inin, T?rkiye genelinde g?nl?k klinik uygulamada hangi noktada oldu?unu g?zlemlemeye y?nelik olarak tasarland?.
Hastalar ve Metod: T?rkiye genelinde 25 farkl? poliklinikte y?r?t?len bu kesitsel ?al??maya toplam 442 KOAH hastas? (ortalama (SS) ya?: 63.2(10.6) y?l;? %76.5'i erkek) dahil edildi. Sosyodemografik ?zellikler, KOAH ?zellikleri, inhaler kullan?m tekni?i ve kuru toz inhaler i?in hasta memnuniyetine dair veriler tek bir kesitsel vizitte kaydedildi.?
Bulgular: Hastalar?n temel ?zellikleri orta ve a??r KOAH (%78.1), y?ksek oranda d?zenli ila? kullan?m? (%89.4) ve ortalama 33.7 ayl?k Turbuhaler? re?etelendirme s?resi, erkek hakimiyeti (%76.5), ilk??retim d?zeyinde e?itim (%85.7), ?ehirde ya?am (68.3), eski sigara i?icili?i (%61.1) ve ev d???nda ge?irilen s?renin ≥ 4 saat/g?n olmas? (%62.0) ?eklinde belirlendi. ?nhalasyon tekniklerinin hastalar?n b?y?k ?o?unlu?unda (≥ %94) do?ru ?ekilde ger?ekle?tirildi?i ancak ?zellikle daha ya?l? grupta olmak ?zere (p< 0.05), cihaz?n a??zdan uzak tutularak nefesin cihaz i?ine nefes ?flenmeden bo?alt?lmas? (%71.9) ve nefesin 5-10 saniye s?resince tutulmas? (%78.3) gibi inhalasyon manevralar?n?n daha d???k oranda do?ru ?ekilde yap?ld??? tespit edildi. Toplamda, ya? ve e?itim seviyesinden ba??ms?z ?ekilde, hastalar?n %73.3'? inhalasyon uygulamas? yaparken inhalasyon cihaz?n? do?ru kulland?klar?n? hissettiklerini ve %86's? inhalasyon cihaz?ndan genel olarak memnun kald?klar?n? belirtti.
Sonu?: T?rkiye klinik uygulama verilerini yans?tan bulgular?m?z, hastalar?n b?y?k ?o?unlu?unun e?itim d?zeyinden ba??ms?z ancak inhalasyon manevralar?nda ya?la artan hata oran? temelinde, Turbuhaler? kullan?m?n? do?ru ?ekilde yapabildi?ini g?stermektedir. Turbuhaler? hastalar?n b?y?k ?o?unlu?u taraf?ndan kullan?m kolayl???, ta??nabilirlik ve i?e yararl?k a??s?ndan olduk?a elveri?li bulunmu? ve hastalar?n %73'?n?n inhaler cihaz? do?ru kulland?klar?na dair kendilerine g?vendi?i, %86's?n?n ise ya? ve e?itim d?zeyinden ba??ms?z olarak inhaler tedavisinden memnun oldu?u anla??lmaktad?r.
Anahtar Kelimeler: KOAH, hasta profili, inhaler teknikleri, hasta memnuniyeti, eri?kinler, kesitsel, T?rkiye.
SUMMARY
Evaluation of inhaler technique and patient satisfaction with fixed-combination budesonide/ formoterol dry-powder inhaler in chronic obstructive pulmonary disease (COPD): data on real-life clinical practice in Turkey
Can
?ZT?RK1, Ak?n KAYA2, Cahit B?LG?N3, Leyla
Y?CESOY4, Belgin ?K?DA?5, Mustafa DEM?REL6,
?eyma
BA?LILAR7, Beng? ?AYLAN7, Tuncer ?ENOL8, Semih
A?ANO?LU9, Gonca CAN10,
Mustafa Ilgaz DO?RUL11,
Murat ?AM12, Nezaket ERDO?AN13, ?zg?r BATUM14,
Muzaffer Onur TURAN15,
Cahit DEM?R16, ?erife TORUN17,
Murat C?R?T18, Mehmethan TURAN19, Arif KELE?O?LU20,
Sava? YA?AR21, ?znur UZUNAY17, Kevser MELEK22,
Osman ALTIPARMAK23
1 Gazi University Faculty of Medicine, Ankara, Turkey,
2 Ankara University Faculty of Medicine, Ankara, Turkey,
3 Hendek State Hospital, Sakarya, Turkey,
4 Private IMC Hospital, Mersin, Turkey,
5 Private SEV American Hospital, Gaziantep, Turkey,
6 Kayseri Private Sevgi Hospital, Kayseri, Turkey,
7 Umraniye Training and Research Hospital, Istanbul, Turkey,
8 Private OSM Ortadogu Hospital, Sanliurfa, Turkey,
9 Private SAR Hospital, Rize, Turkey,
10 Bafra State Hospital, Samsun, Turkey,
11 Cankiri State Hospital, Cankiri, Turkey,
12 Nazilli State Hospital, Aydin, Turkey,
13 Private Adana Ortadogu Hospital, Adana, Turkey,
14 Bartin State Hospital, Bartin, Turkey,
15 Bolvadin Dr. Halil Ibrahim Ozsoy State Hospital, Afyonkarahisar, Turkey,
16 Elazig Private Bronko-Med Chest Diseases Center, Elazig, Turkey,
17 Beyhekim State Hospital, Konya, Turkey,
18 Buca Seyfi Demirsoy State Hospital, Izmir, Turkey,
19 Sorgun State Hospital, Yozgat, Turkey,
20 Diskapi Yildirim Beyazit Training and Research Hospital, Ankara, Turkey,
21 Konya Numune Hospital, Konya, Turkey,
22 Kocaeli Derince Training and Research Hospital, Kocaeli, Turkey,
23 Manisa State Hospital, Manisa, Turkey.
Introduction: The present study was designed to evaluate inhaler techniques and patient satisfaction with fixed-combination budesonide/formoterol dry-powder inhaler chronic obstructive pulmonary disease (COPD) in Turkey in real-life clinical practice.
Patients and Methods: A total of 442 patients with COPD [mean (SD) age: 63.2 (10.6) years, 76.5% were males] were included in this cross-sectional study conducted at 25 outpatient clinics across Turkey. Data on socio-demographic characteristics, characteristics of COPD, inhaler technique and satisfaction with dry-powder inhaler were recorded at a single cross-sectional visit performed at the study enrolment.
Results: Patients were characterized by prominence of moderate to severe (78.1%) COPD, high rate of regular use of overall COPD medications (89.4%) and Turbuhaler? for an average of 33.7 months, predominance of males (76.5%), primary education (85.7%), urban location (68.3), ex-smokers (61.1%) and spending time outdoors for ≥ 4 hour/day (62.0%). Use of correct techniques was evident in majority of patients (≥ 94%), whereas inhalation maneuvers including breathing out gently away from mouthpiece without blowing into it (71.9%) and holding the breath for 5-10 seconds (78.3%) were performed correctly by lesser percent of patients especially in the older group (≥ 65 years, p< 0.05). Overall percent of patients with the feeling that she/he used the inhaler very/fairly correctly was 73.3%, while 86% of patients identified that they were very/fairly satisfied with the inhaler, irrespective of age and educational status.
Conclusion: In conclusion, our findings revealed the majority of patients are able to use Turbuhaler? correctly regardless of the educational status, while older age was associated with higher rate of errors in inhalation maneuvers in the real clinical practice in Turkey. Majority of our patients identified Turbuhaler? to be very/fairly convenient regarding ease of use, portability, and usability with an overall self-confidence in using the inhaler correctly among 73% and the satisfaction rate of 86%; irrespective of age and educational level.
Key Words: COPD, patient profile, inhaler techniques, patient satisfaction, adults, cross-sectional, Turkey.
Geli? Tarihi/Received: 20/11/2012 - Kabul Edili? Tarihi/Accepted: 19/12/2012
INTRODUCTION
Characterized by chronic airflow limitation that is not fully reversible and associated with significant morbidity and mortality worldwide, chronic obstructive pulmonary disease (COPD) is currently a global health priority in which effective management requires long-term adherence to pharmacotherapies (1,2,3).
Estimated to effect 23.6 million (13.9% of the adult population) people according to Global Initiative for Chronic Obstructive Lung Disease (GOLD) definition, with approximately 10% in severe or very severe stages of the disease that results from interaction between individual risk factors (like enzymatic deficiencies) and environmental exposures to noxious agents, like cigarette smoking, occupational dusts, air pollution and infections in childhood (1,2,4). Besides, any patient above the age of 40 is known to be at risk of this disease with higher risk of complications and increased morbidity from this disease in the advanced age (5).
Whilst no pharmacotherapies have been shown to modify the long-term decline of lung function in COPD patients, current guidelines note a preference for maintenance therapy with long-acting inhaled bronchodilators (e.g., beta-agonists and anti-cholinergics) which can control symptoms, improve health status, and reduce the exacerbations (1,4). Inhaled corticosteroids (ICSs) have also been associated with significant clinical benefits in patients with moderate-to severe COPD currently symptomatic on regular bronchodilator therapy; while the patients who used an ICS, a LABA, or an ICS plus a LABA were indicated to have better survival than patients who were only using short-acting bronchodilators (2). Hence being the cornerstone of therapy in COPD, drugs for inhalation including pressurized metered dose inhalers (pMDIs) and dry powder inhalers (DPIs) become the most commonly used devices (6).
Poor handling and inhalation technique are associated with decreased medication delivery and poor disease control (7). In this respect, while can be particularly difficult for some patients, including the elderly and children, DPIs can be easier to use than pMDIs for some patients since they are breath activated, precluding the need for the patient to coordinate actuation with inhalation (6). DPIs, including Aerolizer, Diskus, Handihaler, and Turbuhaler, are flow dependent devices known to require minimal patient-device coordination (7).
Nevertheless, international guidelines for the management of COPD do not differentiate between various inhaler devices indicating that device selection should be based on the availability, cost of the device, patient and physician preference, and clinical setting (4,8).
The effectiveness of drugs for inhalation such as beta-2 agonists, anticholinergic agents or corticosteroids, has been reported to be influenced by many factors including age, gender and education of the patient, duration of disease, type of inhaler used, correct inhalation technique or use of several inhalers (6). Although successful management requires long-term adherence to pharmacotherapies in COPD and non-adherence is associated with increased mortality, morbidity, hospitalizations, and reduction in quality of life, adherence levels observed in real-life clinical practice (10-40%) were reported to be far lower than determined in clinical trials (70-90%) (1).
Given that complexity of the treatment regimen is considered amongst the factors that influence adherence to therapy and limited data available on patients' handling of their usual inhaler devices in real-life primary care or pulmonary clinical practice, this national observational cross-sectional study was designed to evaluate inhaler techniques and patient satisfaction with fixed-combination budesonide/formoterol DPI COPD in Turkey in the real-life clinical practice (1,7).
PaTIents and Methods
Study Population
A total of 442 patients with COPD [mean (SD) age: 63.2 (10.6) years, 76.5% were males] were included in this national, multi-center, non-interventional, observational cross-sectional study conducted at 25 outpatient clinics (chest diseases and internal medicine) across Turkey between August and October 2012. Data were collected at a single cross-sectional visit. Male or female patients of ≥ 40 years of age, diagnosed with COPD according to the ICD-10 criteria, under fixed-combination budesonide/formoterol DPI (Turbuhaler?) therapy for at least three months before the study enrolment were included. Pregnancy, treatment with pMDIs, ongoing participation to another randomized clinical trial and previous participation to the present trial were the exclusion criteria.
Written informed consent was obtained from each subject following a detailed explanation of the objectives and protocol of the study which was conducted in accordance with the ethical principles stated in the "Declaration of Helsinki" and approved by the institutional ethics committee.
Data Collection
Data on socio-demographic characteristics (age, gender, educational level, place of residence, family life, time spent per day outdoors and smoking), characteristics of COPD (duration, functional severity), treatment of COPD (inhaler therapy and other treatments), inhaler technique and patient satisfaction with DPI were recorded at a single cross-sectional visit performed at the study enrolment.
Patient Satisfaction
Patient satisfaction with fixed-combination budesonide/formoterol DPI (Turbuhaler?) was evaluated via face to face application of Turkish version of Feeling of Satisfaction with Inhaler (FSI-10) Questionnaire adapted in linguistic and cultural terms for Turkish patient population with COPD (Appendix A). The FSI-10 is a self-report instrument containing 10 questions, each with five possible responses on a 5-point Likert scale (very, fairly, somewhat, not very, hardly at all) scored from 5 to 1, respectively (maximum total score, 50). It assesses the level of satisfaction of patients with the inhaler and includes items on ease or difficulty of use, portability, and usability (9).
Inhaler Technique
Patients' inhaler technique was evaluated by physician's direct observation using the standardized suggested checklist of steps for the use of fixed-combination budesonide/formoterol DPI (Turbuhaler?) (Appendix B).
Statistical Analysis
Statistical analysis was made using computer software (SPSS version 13.0, SPSS Inc. Chicago, IL, USA). Chi-square (χ2) and Fisher tests were used for the comparison of categorical data, Mantel-Haenszel test for the analysis of linear relationship between ordinal variables and Mann Whitney U test for independent groups without normal distribution. Data were expressed as "mean (standard deviation; SD)", minimum-maximum and percent (%) where appropriate. p< 0.05 was considered statistically significant.
Results
Demographic and Basic Clinical Characteristics of Patients
A total of 442 patients with COPD were included in the cross-sectional study. The majority of the patients were male (76.5%), while the mean (SD) age was 63.2 (10.6) years. Having primary education (85.7%), living in a city (68.3%) and living with family (94.1%) were the other commonly identified characteristics. Most of patients were ex-smokers (61.0%) with an overall cigarette consumption of mean (SD) 45.3 (24.2) package year. Mean (SD) time spent per day outdoors was ≥ 4 hour/day in 62.0% of the study population (Table 1).
When evaluated with respect to age groups (< 65 years in 55.9% vs. ≥ 65 years in 44.1%); being female (p=? 0.002), having secondary education (p< 0.001), living in a city (p< 0.011), being a current-smoker (p<? 0.001) and spending time per day outdoors for ≥? 4 hour/day (p= 0.001) were significantly more common in the <? 65 years group compared with ≥ 65 years group (Table 1).
When evaluated with respect to educational level (≤? primary education in 85.7% vs. ≥? secondary education in 14.3%); being aged ≥? 65 years (p<? 0.001), lives in a town or village (p< 0.001) and being an ex-smoker (p< 0.021) were significantly more common in the ≤ primary education group compared with ≥ secondary education group (Table 1).
Characteristics of COPD with Respect to Age Groups and Educational Level
Time past since Turbuhaler? prescription was 33.7 (35.8) months in the overall population. Moderate COPD was determined in 43.0%, regular use of overall COPD medications in 89.4%, and medications other than Turbuhaler? in 93.9% (Table 2).
Milder forms of the disease were more common in patients aged < 65 years (p= 0.019) and patient with ≥ secondary education (p= 0.006) compared with groups of ≥ 65 years and ≤ primary education, respectively (Table 2).
There was no significant difference in the duration of Turbuhaler? use, regular use of COPD medications and use of medications other than Turbuhaler? with respect to age and educational level (Table 2).
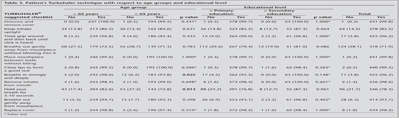
Patient's Turbuhaler Technique with Respect to Age Groups and Educational Level
Evaluation of patients' inhaler techniques according to Turbuhaler suggested checklist by physicians revealed use of correct techniques in most of the steps by majority of patients (≥ 94%), whereas inhalation maneuvers including breathing out gently away from mouthpiece without blowing into it (71.9%) and holding the breath for 5-10 seconds (78.3%) as well as one of the device-related manipulations (keeping inhaler upright, 85.5%) were performed correctly by lesser percent of patients than other steps in inhaler use (Table 3).
Patients in the < 65 years and ≥ 65 years of age were similar in terms of use of correct technique in steps other than breathing in strongly and deeply (98.0 vs. 93.8%, p= 0.025) and holding the breath for 5-10 seconds (82.6 vs. 72.8%, p= 0.013) both of which were determined to be performed by significantly higher percent of patients in the younger group compared to ≥ 65 years of age. There was no significant influence of educational level on inhaler technique (Table 3).
FSI-10 Questionnaire with Respect to Age Groups and Educational Level
Overall mean (SD) score obtained from FSI questionnaire was 43.9 (5.8) which indicates high level of satisfaction with Turbuhaler? in the study population. Mean (SD) FIS score was significantly higher in patients aged < 65 years than ≥ 65 years (44.7 vs. 42.9%, p= 0.0013). FIS scores were similar between patients with ≤ primary education and ≥ secondary education groups [43.7 (5.9) vs. 45.2 (4.7), p= 0.089].
Considering individual items, 75.7% of patients identified that it has been very/fairly easy to learn how to use the inhaler, 86.4% noted that it was very/fairly easy to prepare the inhaler for use and 83.4% identified that it was very/fairly easy to use the inhaler. Also, it was considered very/fairly easy by majority of patients to keep the inhaler clean and in good working condition (91.6%), to continue normal activities with the use of the inhaler (87.1%); to use inhaler in terms of size and weight (92.1%) and to carry inhaler with them (93.0%). Overall percent of patients with the feeling that she/he used the inhaler very/fairly correctly was 73.3%, while 86% of patients identified that they were very/fairly satisfied with the inhaler (Table 4).
While significantly higher percent of patients in < 65 years than in ≥ 65 years of age group identified that it was easy for them to learn how to use the inhaler (p= 0.019), to prepare the inhaler for use (p< 0.001), to use the inhaler (p< 0.001), to keep the inhaler clean and in good working condition (p= 0.012), to continue normal activities with the use of the inhaler (p= 0.002); percent of patients with the feeling that she/he used the inhaler correctly and satisfied with the inhaler were similar with respect to age groups (Table 4).
While significantly higher percent of patients in ≥ secondary education than in ≤ primary education group identified that it was easy for them to learn how to use the inhaler (p= 0.005), to use the inhaler (p< 0.002), to keep the inhaler clean and in good working condition (p= 0.009) as well as inhaler fitted their lips comfortably (p= 0.045), percent of patients with the feeling that she/he used the inhaler correctly and satisfied with the inhaler were similar with respect to educational level groups (Table 4).
Discussion
The findings of this real-life cross-sectional study revealed the profile of COPD patients admitting to chest diseases and internal medicine outpatient clinics across Turkey to be characterized by prominence of moderate to severe (78.1%) COPD, high rate of regular use of medications (89.4%) and Turbuhaler? for an average of 33.7 months, predominance of males (76.5%), primary education (85.7%), urban location (68.3%) and ex-smokers (61.1%) besides ability to spent time outdoors for ≥ 4 hour/day in 62.0% of the study population. Female gender, secondary education, urban location, current smoking, outdoor activities and milder form of the disease were characteristic for younger patients (< 65 years of age), while the older age (≥ 65 years of age), rural location, ex-smoking and more severe forms of the disease were determined more commonly in patients with lower educational level.
It is worth noting that while the tobacco consumption rate has been decreasing in the developed countries (to one-third in the U.S. since the 1950s), based on the data from official market selling rates it has been estimated to have tripled during the last 40 years in Turkey (10). In this regard, predominance of male patients both in the overall study population and in ≥ 65 years of age group in our study supports the previously reported high rate of COPD in the male population in Turkey which has been attributed to the higher smoking rate in the male population (3). Notably, our finding of very high active smoking rates among the younger population composed mostly of females and patients from urban location emphasize the statement that the increase in smoking among younger population may be a serious signal which indicates the maintenance of high smoking prevalence in the population the long term (3).
Considering the inhaler technique, our findings indicated that inhaler technique was correctly performed in majority of patients (≥ 94%) in most steps excluding inhalation maneuvers such as breathing out gently away from mouthpiece without blowing into it (71.9%) and holding the breath for 5-10 seconds (78.3%). While educational level was not associated with inhalation technique, inhalation maneuvers including breathing in strongly and deeply (98.0 vs. 93.8%) and holding the breath for 5-10 seconds (82.6 vs. 72.8%) were performed correctly by higher percent of younger patients.
Although using Turbuhaler? was identified to be much easier in terms of learning and putting into practice of the technique by significantly higher percent of younger patients (< 65 years) and patients with higher educational status (≥ secondary education) compared to older(≥ 65 years) patients and patients with lower educational status (≤ primary education), respectively; higher satisfaction with inhaler was identified in the group of younger age while there was no significant influence of educational level on FSI scores Nevertheless, overall 73.3% of patients confirmed the feeling that she/he used the inhaler very/fairly correctly, while 86% of patients were very/fairly satisfied with the inhaler.
Notably, given the COPD treatment regimens that increase the likelihood of higher medication adherence levels would be expected to contribute to improved disease management, regular use of COPD medications was reported in 89.4% of our patients irrespective of age and educational status (1).
In a past systematic review that analysed studies aimed at evaluating the quality of inhalation technique with well-established DPIs in both adult and pediatric patients with asthma or COPD, the most frequent errors related to Turbuhaler? use were reported to be failure to exhale before inhaling through their DPI, followed by incorrect inhaler positioning and failure by patients to breath hold (6). Accordingly, in our study population most common errors in Turbuhaler? use were failure to exhale before inhalation through inhaler (28.1%) followed by failure of patients to hold their breath after they had completed inhaling through the device (21.7%) and failure to keep inhaler upright (14.5%).
Identification of the critical errors of inhaler technique in almost one-third of our patients during physician evaluation corresponds to the lower limit of the range of rates of misuse (26-94%) reported for the Turbuhalers? and also quite in line with results of a past study on assessment of inhaler technique of the Turbuhalers?, Rotahalers? and Diskhalers? which showed that 40% of the patients were unable to perform all steps correctly (6,11). Indeed, these handling errors have been indicated to be significantly decreased with detailed and repeated education by the health care providers (7).
Indeed, objective identification of critical errors and patients' own feelings about the correctness of their technique pointed out similar percentage of overall erroneous patients (almost 30%) in our study. Hence, it should be emphasized that despite the technical features of inhaler devices have improved constantly with time, the effectiveness in delivering drugs to the lungs depends on correctly performed inhalation maneuvers? with negative outcomes of incorrect use of inhalers most pronounced among patients with poor inspiration maneuvers (6,8,12).
In this regard, overall patient satisfaction of 86% in our study population despite errors in technique, most likely to complicate efficacy of the inhaler, in almost one third of patients, emphasize that relying on patients' judgment of their inhaler technique has not been recommended even with experienced inhaler users (8,13). Besides, while our patients had very satisfactory results during active checking of their inhaler technique by the physician, given that it is based on a single cross-sectional visit, it should be kept in mind that, past studies indicated that even when patients were able to demonstrate correct technique during consultation with a health professional, they may not maintain this standard at other times (8).
In fact, while it was consistently reported that risk of insufficient drug delivery may lead to poor drug efficacy and inadequate control of asthma and patients' inhaler technique can be improved by education given by health care professionals, inhaler technique has been seriously underestimated by healthcare professionals with lack of patient education on inhaler use in 25% of patients with COPD worldwide (6,8,14).
Given that even after training is provided, some patients will continue to have difficulties using inhalers properly, physicians seems responsible not only for demonstration of correct technique and correction of any specific errors identified but also for repeating instructions while actively checking the technique until the patient has all steps correct (8). Besides, health professionals should also make sure their own knowledge of correct technique is up to date before assuming their own technique is correct (13).
Albeit including patients over 40 years of age, overall technical success and patient satisfaction with Turbuhaler? use in our study seems unlike to previous studies reported up to 85% of patients do not use their inhalers correctly (6) and also supports the fact that DPIs, available since the 1970s, have been developed to make inhalation simple, without the need to coordinate inhalation and actuation which could be particularly in the elderly and children (6,15).
Hence, although we did not collect information about co-morbidities in the study population, our findings seems in line with the statement that many elderly people have poor inhalation technique most probably because of comorbidities that may interfere with proper handling technique such as arthritis, weakness or impaired dexterity or vision but only in terms of "breathing in strongly" and "deeply and holding the breath after removal of inhaler", since there was no influence of age in all other steps included in the inhaler technique (16).
Additionally, majority of our patients identified positive opinions regarding ease of use, portability, and usability of devices for delivery of inhaled corticosteroids with an overall high satisfaction rate of 86% of patients.
Inhalation devices with feedback mechanisms which guide patients through the correct inhalation maneuver would be ideal for an improved inhalation technique and, thereby, more appropriate asthma management (6). In this respect, newly developed training devices to optimise patients' breathing whilst using a DPI such as the Mag-Flos (Fyne dynamics Ltd., UK) and the In-Check Dial? (Clement Clarke International Ltd., UK) are promising in their easiness to use and ability to measurement of patient's inspiratory flow which enable inhalation technique to be learned and checked quickly (17,18). However, while useful for training patients how to inhale through a device, these devices are indicated to be free of teaching patients how to hold, prime and position their inhaler device for optimum benefit (6).
Since, proper handling of the inhaler devices is generally required as inclusion criteria of controlled clinical trials (7); these trials could be biased and may not reflect what actually happens in clinical practice (7). In this regard, our findings contribute to data on proper handling of inhaler devices in the real-life clinical practice in Turkey with substantial implications in clinical efficacy and disease control.
In conclusion, our findings related to evaluation of inhaler technique and patient satisfaction with Turbuhaler? in chronic obstructive pulmonary disease (COPD) in real life clinical practice revealed the majority of patients are able to use Turbuhaler? correctly regardless of the educational status, while older age was associated with higher rate of errors in inhalation maneuvers. Majority of our patients identified Turbuhaler? to be very/fairly convenient regarding ease of use, portability, and usability with an overall self-confidence in using the inhaler correctly among 73% of patients and the satisfaction rate of 86%; while satisfaction with inhaler was higher in patients with younger age. Regular assessment and reinforcement of correct inhalation technique by health professionals and caregivers as well as development of easy to use new DPIs with feedback mechanisms which guide patients through the correct inhalation maneuver seem to improve inhalation technique and, thereby, and COPD management. Moreover, future larger scale prospective studies that assess the incidence of incorrect inhaler technique with established DPIs in relation to implications for clinical efficacy and disease control are needed.
AcknowledgEment
The study is granted by AstraZeneca, Turkey. We thank to Prof. Nurhayat Yildirim MD, Prof. Abdullah Sayiner MD, Prof. Zafer Caliskaner MD, for their advisory support. We also thank to Cagla Ayhan, MD and Prof. Sule Oktay, MD, PhD. from KAPPA Consultancy Training Research Ltd, Istanbul who provided editorial support and Oguz Akbas, MD, PhD, and Arzu Calisgan M.Sc. from Monitor CRO, Istanbul for their support in statistical analysis, funded by AstraZeneca, Turkey.
Conflict of interest
None declared.
REFERENCES
- Toy EL, Beaulieu NU, McHale JM, Welland TR, Plauschinat CA, Swensen A, et al. Treatment of COPD: relationships between daily dosing frequency, adherence, resource use, and costs. Respir Med 2011; 105: 435-41.
- Cazzola M, Donner CF, Hanania NA. One hundred years of chronic obstructive pulmonary disease (COPD). Respir Med 2007; 101: 1049-65.
- Gunen H, Hacievliyagil SS, Yetkin O, Gulbas G, Mutlu LC, Pehlivan E. Prevalence of COPD: first epidemiological study of a large region in Turkey. Eur J Intern Med 2008; 19: 499-504.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2011 update. Available at, http://www.ginasthma.org/uploads/users/files/GINA_Report2011_May4.pdf
- Hardie JA, Vollmer WM, Buist AS, Bakke P, Morkve O. Respiratory symptoms and obstructive pulmonary disease in a population aged over 70 years. Respir Med 2005; 99: 186-95.
- Lavorini F, Magnan A, Dubus JC, Voshaar T, Corbetta L, Broeders M, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med 2008; 102: 593-604.
- Khassawneh BY, Al-Ali MK, Alzoubi KH, Batarseh MZ, Al-Safi SA, Sharara AM, et al. Handling of inhaler devices in actual pulmonary practice: metered-dose inhaler versus dry powder inhalers. Respir Care 2008; 53: 324-8.
- National Asthma Council Australia. Inhaler technique in adults with asthma or COPD. 2008.http://www.nationalasthma.org.au/uploads/content/237-Inhaler_technique_in_adultswith_asthma_or_COPD.pdf. Accessed on November 14, 2012.
- Perpina Tordera M, Viejo JL, Sanchis J, Badia X, Cobos N, Picado C, et al. Assessment of patient satisfaction and preferences with inhalers in asthma with the FSI-10 Questionnaire. Arch Bronconeumol 2008; 44: 346-52.
- World Bank data. www.worldbank.org/tobacco/pdf/country/Turkey
- van der Palen J, Klein JJ, Kerkhoff AHM, van Herwaarden CL. Evaluation of the effectiveness of four different inhalers in patients with chronic obstructive pulmonary disease. Thorax 1995; 50: 1183-7.
- Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J 2002; 19: 246-51.
- Basheti IA, Armour CL, Bosnic-Anticevich SZ, Reddel HK. Evaluation of a novel educational strategy, including inhaler based reminder labels, to improve asthma inhaler technique. Patient Educ Couns 2008; 72: 26-33.
- Sestini P, Cappiello V, Aliani M, Martucci P, Sena A, Vaghi A, et al. Prescription bias and factors associated with improper use of inhalers. J Aerosol Med 2006; 19: 127-36.
- Newman SP, Busse WW. Evolution of dry powder inhaler design, formulation, and performance. Respir Med 2002; 96: 293-304.
- Franks M, Briggs P. Use of a cognitive ergonomics approach to compare usability of a multidose dry powder inhaler and a capsule dry powder inhaler: an open-label, randomized, controlled study. Clin Ther 2004; 26: 1791-9.
- http://www.fyne.dynamics.com/articles/spec_magflo.htmS.
- Chrystyn H. Is inhalation rate important for a dry powder? Using the in-check dial to identify these rates. Respir Med 2003; 97: 181-7.
Yaz??ma Adresi (Address for Correspondence):
Dr. Can ?ZT?RK,
Gazi ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?,
ANKARA - TURKEY
e-mail: canozturk.gazi@gmail.com