Sa? pulmoner ven atrezisi: Olgu sunumu ve literat?r?n g?zden ge?irilmesi
?erife SAVA? BOZBA?1, Birg?l VARAN2, ?ule AK?AY1
1 Ba?kent ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Ankara,
2 Ba?kent ?niversitesi T?p Fak?ltesi, Pediatrik Kardiyoloji Bilim Dal?, Ankara.
?ZET
Sa? pulmoner ven atrezisi: Olgu sunumu ve literat?r?n g?zden ge?irilmesi
E?lik eden do?umsal bir patoloji olmaks?z?n izole pulmoner ven atrezisi eri?kinlerde olduk?a nadir g?r?lmektedir, artm?? mortalite ve morbidite ile ili?kilidir. Hastalar tekrarlayan akci?er infeksiyonlar?, eforla geli?en nefes darl??? ve hemoptizi ?ikayetleriyle hastaneye ba?vurmaktad?rlar. ?ok nadir g?r?lmesi nedeniyle tan? ve tedavide birtak?m zorluklar ya?anabilmektedir. Bu yaz?da, eri?kin ya?ta saptanan izole pulmoner ven atrezili olgu nedeniyle tan? ve tedavi se?enekleri g?zden ge?irilmi?tir.
Anahtar Kelimeler: Pulmoner ven atrezisi, tekrarlayan akci?er infeksiyonu, pulmoner anjiyografi.
SUMMARY
Right pulmonary venous atresia: a case report and review of literature
?erife SAVA? BOZBA?1, Birg?l VARAN2, ?ule AK?AY1
1 Department of Chest Diseases, Faculty of Medicine, Baskent University, Ankara, Turkey,
2 Division of Pediatric Cardiology, Faculty of Medicine, Baskent University, Ankara, Turkey.
Isolated pulmonary vein atresia without associated congenital malformation is a very rare condition in adults. It is associated with significant mortality and morbidity. Recurrent pulmonary infections, dyspnea on exertion and hemoptysis may be the presenting complaints. Owing to the limited number of patients with this condition there may be some difficulties in it's diagnosis and therapy. We report an adult case with this rare congenital malformation and discuss it's diagnosis and management options.
Key Words: Pulmonary venous atresia, recurrent pulmonary infection, pulmonary angiography.
Geli? Tarihi/Received: 21/12/2010 - Kabul Edili? Tarihi/Accepted: 02/03/2011
INTRODUCTION
Unilateral pulmonary vein atresia without associated congenital abnormalities is a very rare clinic condition (1,2). It is of prognostic importance with significant mortality and morbidity. Patients suffering from this condition usually present with recurrent lung infections or hemoptysis in infancy or childhood (3). Dyspnea on exertion is another manifestation that usually seen in the late course of the disease (4). The diagnosis may be challenging. We report an adult patient with right pulmonary venous atresia and discuss the the diagnostic tests and therapeutic modalities.
CASE REPORT
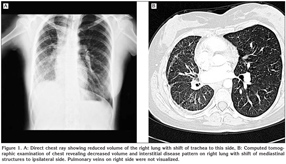
A 20-year-old female college student admitted to our clinic with dsypnea on exertion. She had this complaint for two years. On her past medical history she had pneumonia three years ago. On physical examination respiratory sounds were decreased on right hemithorax and cracles were heard on base of the right lung. Direct chest X-ray was obtained which revealed reduced volume of the right lung with shift of trachea to this side (Figure 1A). Computed tomographic examination of the chest showed decreased volume and interstitial disease pattern on right lung with shift of mediastinal structures to ipsilateral side. Right pulmonary veins were not identified on tomographic scans (Figure 1B). On transthoracic Doppler echocardiographic examination the right pulmonary veins were also could not be visualized. The estimated systolic pulmonary pressure on Doppler examination was normal. The right and left ventricular function were found as normal and interatrial and interventricular septums were intact. To confirm the diagnosis cardiac catheterization and pulmonary angiography were performed. On oxymetric study oxygen saturation was higher on right pulmonary artery than that of the left (99% vs. 89%, respectively). This finding suggested the presence of systemic arterial blood flow to pulmonary arteries on the affected side. On selected left pulmonary artery angiography the perfusion of the left lung was identified to be normal with normal pulmonary veins draining into left atrium (Figure 2A). However on selected right pulmonary angiography decreased perfusion of the right lung was noted and pulmonary veins on this side were not visualized (Figure 2B). Instead prominent intercostal arteries were identified supplying blood to the right lung. The patient was discussed with cardiologists and cardiovascular surgeons and conservative approach was chosen for her. She and her family were informed about this condition and close follow up were scheduled.
DISCUSSION
Pulmonary venous atresia is a rare condition which associated with congenital heart defects in around 1/3 of the cases (2). Isolated pulmonary vein atresia without associated congenital malformation is quite rare in adults. To our best of knowledge less than 50 case reports were published in medical literature to date, most of whom were infants (1,2,3,4,5,6,7).
It may have a grave prognosis. If left untreated mortality rate is reported to be as high as 50% (3).
Severe medial hypertrophy with intimal fibrosis is seen on histologic examination of pulmonary veins in affected individuals (8,9). The cause of pulmonary venous atresia is congenital in the majority of cases. However, occasionally it may be acquired. It can be seen as a complication of surgery, in conjunction with mediastinal tumors, infections, intracardiac tumors/thrombi (8).
Recurrent pulmonary infections are the basic feature of unilateral pulmonary venous atresia. Dyspnea on exertion, which is the main complaint in our case, is another common symptom. Occasionally hemoptysis may be the presenting complaint. Cyanosis is not expected unless associated with other congenital malformations. In affected cases symptoms usually seen during infancy or childhood.
As expected, in the affected lung gas exchange at the alveolar level is inadequate. A significant ventilation perfusion missmatch is evident. Due to hypoplasia of pulmonary arteries on the affected side systemic collaterals develop. This causes a left to right shunt. On oxymetric study high oxygen saturation on ipsilateral pulmonary artery should alert us about pulmonary venous atresia. In the present case oxygen saturation in the right pulmonary artery was equal to that of systemic blood. Computed tomography and magnetic resonance imaging are very helpful diagnostic tools in suspected cases. For definitive diagnosis pulmonary artery wedge angiography should be performed. In our case on selected right pulmonary angiography we confirmed the diagnosis of right pulmonary venous atresia.
Heyneman et al. reported three adult patients aged 25, 31 and 43 years with unilateral pulmonary venous atresia (1). Two of them were presented with significant hemoptysisa and one with recurrent episodes of pneumonia and progressive dyspnea. Two cases with hemoptysis had a history of associated congenital heart disease, ventricular septal defect that closed spontaneously in one and patent ductus arteriosus that closed surgically in another patient. And one of them had persistent superior vena cava. Pneumonectomy was performed in two while one patient with hemoptysis underwent bronchial artery embolization.
Owing to the limited number of patients with this condition data for long term follow up is very limited. Concerning the current evidence basically three therapeutic options are available. The first is conservative approach. As in our case, if the affected person has not frequent respiratory infections, has not significant symptoms and no pulmonary hypertension developed then this approach might be chosen. The second option is pneumonectomy, in which situation the removal of nidus for infection is aimed. Available evidence indicate that the outcome of pulmonary resection is satisfactory (8,10,11). This approach might especially be suggested in patients who suffer from recurrent pulmonary infections. In cases with pulmonary hypertension or significant hemoptysis pneumonectomy should also be considered as the therapy of choice. The third approach is reperative surgery. Experience is very limited and reported outcome with this type of surgery is not good (12). However it can be considered when this condition is detected early in life before irreversible changes develop in pulmonary tissue and circulation (13).
In our case no associated congenital heart disease was noted on echocardiographic, tomographic and catheter/angiographic evaluation. Our case is a very rare example of isolated pulmonary vein atresia in adulthood. She was presented with mild-moderate symptoms at an adult age with no restriction of daily activities. Therefore no intervention was suggested. We think that absence of pulmonary hypertension and no additional congenital malformation are the basic reasons for her well being to date. However, attention should be paid on the development of pulmonary hypertension in such cases. Therefore these cases should be followed up regularly for the development of pulmonary hypertension and respiratory symptoms. Pneumonectomy should be considered when pulmonary hypertension develop or recurrent pulmonary infections occur.
CONFLICT of INTEREST
None declared.
REFERENCES
- Heyneman LE, Nolan RL, Harrison JK, McAdams HP. Congenital unilateral pulmonary vein atresia: radiologic findings in three adult patients. Am J Roentgenol 2001; 177: 681-5. [?zet] [Tam Metin] [PDF]
- Pourmoghadam KK, Moore JW, Khan M, Geary EM, Madan N, Wolfson BJ, et al. Congenital unilateral pulmonary venous atresia: definitive diagnosis and treatment. Pediatr Cardiol 2003; 24: 73-9. [?zet]
- Cullen S, Deasy PF, Tempany E, Duff DF. Isolated pulmonary vein atresia. Br Heart J 1990; 63: 350-4. [?zet] [PDF]
- Harrison JK, Hearne SE, Baker WA, Van Trigt P, Leidig G, Bashore TM, et al. Esophageal varices in association with unilateral pulmonary vein atresia. Cathet Cardiovasc Diagn 1996; 38: 387-92. [?zet]
- Tissot C, Corbelli R, Aggoun Y, Beghetti M, da Cruz E. Bronchoscopic diagnosis of asymptomatic unilateral pulmonary vein atresia in an infant. Pediatr Cardiol 2008; 29: 976-9. [?zet]
- Ussia GP, Marasini M, Rimini A, Pongiglione G. Atresia of right pulmonary veins with intact atrial septum and major aortopulmonary collateral treated with percutaneous stent implantation and embolization. J Interv Cardiol 2004; 17: 183-87. [?zet]
- Wiebe S, Maclusky I, Manson D, Holowka S, Yoo SJ. Hemoptysis: a rare cause can be related to a bronchial varix due to pulmonary venous obstruction. Pediatr Radiol 2003; 33: 884-6. [?zet]
- Beerman LB, Oh KS, Park SC, Freed MD, Sondheimer HM, Fricker FJ, et al. Unilateral pulmonary vein atresia: clinical and radiographic spectrum. Pediatr Cardiol 1983; 4: 105-12. [?zet]
- Cabrera A, Vazquez C, Lekuona I. Isolated atresia of the left pulmonary veins. Int J Cardiol 1985; 7: 298-302. [?zet]
- Shrivastava S, Moller JH, Edwards JE. Congenital unilateral pulmonary venous atresia with pulmonary venoocclusive disease in contralateral lung: an unusual association. Pediatr Cardiol 1986; 7: 213-9. [?zet]
-
Swischuk LE, L'Heureux P. Unilateral pulmonary vein atresia. Am J Roentgenol 1980; 135: 667-72.
[?zet] [Tam Metin] [PDF] -
Shimazaki Y, Nakano S, Kato H, Ohtake S, Ikawa S, Miura T, et al. Mixed type of total
anomalous pulmonary venous connection with hemi-pulmonary vein atresia. Ann
Thorac Surg 1993; 56: 1399-401.
[?zet] - Argueta-Morales IR, Garg R, DeCampli WM. Diagnosis and management of congenital right pulmonary venous atresia. Cardiol Young 2009; 19: 648-51. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. ?erife SAVA? BOZBA?,
Ba?kent ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?, Bah?elievler
ANKARA - TURKEY
e-mail: drserifesavas@yahoo.com