Mounier-Kuhn
sendromlu olguda malign fibr?z histiyositom metastaz?na ba?l?
ana hava yolu
obstr?ksiyonu
Levent
DALAR1, Emel ERY?KSEL2, Filiz KO?AR2, Ahmet
Levent KARASULU2, Nur ?RER2,
Sinem Nedime S?K?C?2, Sedat ALTIN2
1 Yedikule G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi,
7. G???s Hastal?klar? Klini?i, ?stanbul,
2 Yedikule G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, ?stanbul.
?ZET
Mounier-Kuhn sendromlu olguda malign fibr?z histiyositom metastaz?na ba?l? ana hava yolu obstr?ksiyonu
Malign fibr?z histiyositoma eri?kinlerde g?r?len yumu?ak doku sarkomlar? aras?nda s?k izlenen tiplerden biridir. Akci?er en s?k rastlanan metastaz alan?d?r. Mounier-Kuhn sendromu ise trakea ve bron?lar?n ileri derecede geni?lemesiyle karakterizedir. Ana hava yolu obstr?ksiyonu, endoluminal, ekstraluminal ya da her iki komponentin birarada oldu?u akci?er ve mediasten kitlelerinde kar??m?za ??kabilir. Bu yaz?da, nadir g?r?len bir klinik durumun dev mediastinal malign fibroz histiyositoma metastaz?na sekonder olarak olu?mas? ve di?er yandan kitlenin yol a?t??? ana hava yolu obstr?ksiyonunun ??z?lmesinde ya?anan zorluklar?n klinik ?nemini vurgulamak istedik. Mounier-Kuhn sendromu ve ana hava yolu obstr?ksiyonu birlikteli?i ve bu durumun y?netilmesinde ya?anan g??l?kler ?ngilizce literat?rde daha ?nce sunulmam??t?r.
Anahtar Kelimeler: Hava yolu, hava yolu stenti, histiyositom, obstr?ksiyon, trakea.
SUMMARY
Central airway obstruction due to malignant fibrous histiocytoma metastasis in a case with Mounier-Kuhn syndrome
Levent
DALAR1, Emel ERY?KSEL2, Filiz KO?AR2, Ahmet
Levent KARASULU2, Nur ?RER2,
Sinem Nedime S?K?C?2, Sedat ALTIN2
1 Clinic of 7th Chest Diseases, Yedikule Chest Diseases and Chest Surgery Training and Research Hospital,
Istanbul, Turkey,
2 Yedikule Chest Diseases and Chest Surgery Training and Research Hospital, Istanbul, Turkey.
Malign fibrous histiocytoma is one of the most observed soft tissue sarcomas seen in the adults. The most common metastasis region is the lung and metastasis. Mounier-Kuhn syndrome is characterized by the highly dilatation of the trachea and bronchi. We may encounter with the major airway obstruction in the endoluminal or extraluminal lung and mediastinal masses or those with both components together. In this article, we would like to highlight the occurrence of a rare seen clinical situation secondary to the giant mediastinal malign fibrous histiocytoma metastasis and the clinical difficulties experienced in resolving of the main airway obstruction caused by the mass. Since the lack of the similar studies conducted previously, we found the case worth presenting.
Key Words: Airway, airway stent, hystiocytoma, obstruction, trachea.
Geli? Tarihi/Received: 26/02/2011 - Kabul Edili? Tarihi/Accepted: 21/04/2011
INTRODUCTION
Malign fibrous histiocytoma (MFH) is one of the most observed soft tissue sarcomas seen in the adults. It is accounted for 10% of all the sarcomas (1). This sarcoma originates from the trunk of the extremities, and distant metastasis is observed in nearly 30 to 40% of the patients (2). The most common metastasis region is the lung and metastasis to the other areas out of the lung is extremely uncommon (2). Mounier-Kuhn syndrome has been first described by Mounier-Kuhn in 1932 and is characterized by the highly dilatation of the trachea and bronchi (3). We may encounter with the major airway obstruction in the endoluminal or extraluminal lung and mediastinal masses or those with both components together. Thermal methods, mechanical disobstruction and dilatation and stent insertion are used in the management of this clinical condition depending on the nature of the lesion (4).
In this article, we would like to highlight the occurrence of a rare seen clinical situation secondary to the giant mediastinal MFH metastasis and the clinical difficulties experienced in resolving of the main airway obstruction caused by the mass. Since the lack of the similar studies conducted previously, we found the case worth presenting.
CASE REPORT
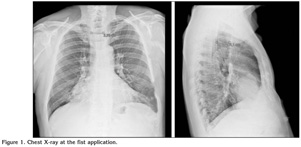
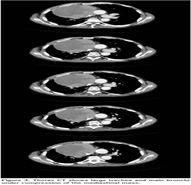
A 58-years-old male patient presented to the orthopedic clinic due to swelling in the left elbow in January 2009. Diagnosis of malignant fibrous histiocytoma was established following the excisional biopsy, and the metastasis screening was performed. After the excision, there was not tumor cell defined in the surgical borders of the mass. At the same period, a mass of 4 cm was detected in the right lung (Figure 1). However, the patient refused further analysis and examinations and left the hospital. After two months, he referred to the same clinic once again on the re-development of swelling in the left elbow. The mass was totally excised, and chemoradiotherapy was recommended. The patient was guided to our clinic on the growth of the lung mass compared to two months ago. MFH diagnosis was established with the mediastinoscopy, but an operation was not performed for the mass due to the high preoperative risk (Figure 2). Following the diagnosis in April 2010, on the CT ordered because of the rapid progression of the mass and onset of the respiratory distress, the mass was defined to almost completely obstruct both bronchial entries, creating pressure at the level of main carina (Figure 3).
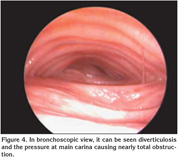
On the bronchoscopy, distal part of the trachea and both bronchial entries were seen to be prominently obstructed at the carinal level (Figure 4). There was not an additional finding defined on the chest graphy in this period suggesting additional pathologies would lead to dyspnea such as pulmonary embolism. Stent insertion was planned due to the severity dyspnea during the patient's daily activity. At the first process, palliation of the obstruction was tried to be obtained using a Dumon silicon Y stent of 18 x 14 x 14 mm. However, the stent was removed to prevent the possible migration and chronic coughing since the tracheal leg was moving because of the trachea was highly expanded. Only with insertion of the silicon Dumon stent to the left main bronchus the passage was provided. The patient was transferred to the intensive care unit as intubated and extubated at the 8th hour. The case with partly improved respiratory distress at that period was taken to the service. He was intubated again and taken to the intensive care unit on the re-development of the respiratory distress. On the bronchoscopy, the stent inserted to the left main bronchus was seen to be at the place, but the pressure was persistent at the supracarinal level and the lumen was seen to be prominently obstructed. The case was considered as the ventilator related pneumonia due to the definition of progressive leukocytosis and increase in the secretion quantity, and an appropriate antibiotherapy was introduced with piperacillin/tazobactam 4 x 4.5 and ciprofloxacin 200 mg 2 x 1. However, the patient was lost at the 12th day of the re-intubation because of the multiorgan failure developed due to sepsis, despite all the treatment interventions.
DISCUSSION
MFH, is one of the most common soft tissue sarcomas seen in the adults. It often originates from the trunk of the extremities. Distal metastasis is developed in nearly 30 to 40% of the cases and the most common location is the lung. Development of the distal metastasis without the lung is very uncommon (1,2).
Since the lung is the most common metastasis region, this leads to development of the metastases involving both parenchymal and endobronchial areas. It often involves only the lung parenchyma and endobronchial metastasis is extremely rare (5,6,7). Surgical resection of the mass is frequently necessary for the definitive diagnosis and the treatment. Interventional methods such as the surgery and laser are the main treatments of choice. Whereas metastasectomy is the preferred method in the metastases involving the parenchyma.
In a disease series of Syri et al. with 103 patients, complete resection was performed at 93 cases, and one patient was preoperatively lost. Survival rate of 5 years was found as 21% (8). Mediastinal metastasis is uncommon but it may primarily result from the anterior mediastinum (9). In our study, despite the tumor formed in the right forearm was operated; the patient was referred again to the hospital after six months because of the growth of the mass exciting in the anterior mediastinum at the admission. On the bronchoscopy ordered in that period, the trachea and main bronchi were found normal except a slight pressure and the diagnosis was achieved through the mediastinoscopy. There was not a response obtained to the treatment in the patient with chemotherapy applied due to the resection could not be implemented. On the bronchoscopy performed because of the progressive dyspnea, diffuse diverticulosis was seen trachea and distal part, and both main bronchi were seen to be obstructed due to the anterior pressure at the carinal level on the expiration. Certain difficulties were experienced in the management of the obstruction at this stage. First, stents with diameters suitable for the highly expanded trachea and bronchi are not available. This situation can be overcome only with the stents produced on a special order. Dutau et al. resolved the obstruction developed as a result of the tracheal compression in a similar case with tracheomegaly using a metallic covered stent of 28 mm and they followed-up the patient without complications for two years by "weaning" (10). However, in our country it takes at least three weeks to reach to the stents via a special order. Therefore, inaccessibility of the stents has hampered overcome the carinal obstruction.
Number of the previously reported cases with Mounier-Kuhn syndrome in the literature is about 100 (11). The anomalies monitored in this lesion include the following criteria: diameter of the right main bronchus must exceed 2.4 cm and the left main bronchus 2.3 cm and the diameter of the trachea is expected to exceed 3.0 cm. According to the study by Menon et al., the diameter of the transverse trachea was 21 mm in the females with Mounier-Kuhn syndrome diagnosis and the diameter of the sagittal trachea 23 mm, while the diameter of right main bronchus exceeded 19.8 mm and the left main bronchus 17.4 mm. Whereas in the males, the diameter of the transverse tracheas must exceed 25 mm and the sagittal diameter 27 mm. However, especially in the males, the right main bronchus was reported to be expected to be wider than 21.1 mm and the left main bronchus 18.4 mm (12).
Three subtypes of the Mounier-Kuhn syndrome have been described. Type 1 includes symmetric tracheal and bronchial expansion. Type 2 has an excentric expansion. And diffuse diverticulosis is observed together with the expansion of the distal bronchi in the Type 3. The muscularis mucosa layer has been thickened with the atrophy in the elastic fibers and this leads to the dilatation of the trachea (13). This situation causes the patient to present tendency to the infections. The exact and real reason of these changes is unknown. However, existing together with some hereditary conditions suggests its emerging as a part of the diffuse connective tissue disorder.
Our case also could be classified as Type 3 since the association with the diffuse diverticulosis. Although concomitant bronchiectasis and fibrosis are observed in most of the tracheobronchomegaly cases, there was not a similar situation in our patient (14). Also, observing of two simultaneous clinical conditions due to the connective tissue suggests an underlying disorder related to the function of the collagen and cartilage tissue of the case. On an increase of the respiratory distress, a silicon Dumon Y stent of 18 x 14 x 14 mm was tried. However, the stent remained moving on the carina after the insertion because of the highly expansion of the trachea. Since this condition was known to cause coughing and due to risk for the mucus retention and migration, the stent was removed. The patency of the left main bronchus was enabled by a Dumon silicon stent inserted. However, this situation did not lead to a significant resolving in the airway dynamic. In a previously reported study on a case with tracheobronchomegaly, tried a Freitag dynamic stent and achieved the extubation of the patient (15). Giannoni et al. suggested that the concomitant tracheobronchomalacia blocked the mucus expectoration, and this dynamic formation played a strong role in the obstruction. The subsequent resolving in the respiratory mechanic they obtained might suggest this clinical judgment was valid. Whereas in our case, mechanic narrowing to be in the forefront and lack of the Y stent in a suitable size lead not to obtain a permanent solution. The tracheal leg of the stent to be moving due to highly expanded trachea and diameters of the bronchi would make the respiratory mechanic disordered as well as lead to the formation of a coughing obviously disturbing the life quality. Also it was obvious not to contribute to the improving of the respiratory mechanic. Since a stent of 18 mm was inserted only into the left main bronchus and could not be into the right main bronchus and at the same time the compression at the low end of the trachea could not be resolved, the patient was lost. Availability of the suitable stent constitutes the key point for the management of this clinical condition required to be overcome despite it is uncommon.
Accompanying of a mesenchyme origin tumor to Mounier-Kuhn syndrome occurred also due to the supportive tissue abnormality is an extremely rarely observed clinical condition. Besides, development of the central airway obstruction despite highly dilatation and this obstruction could not be managed as required due to the lack of the suitable stent may lead the way for the future cases. Malignant obstruction developing in the highly expanded trachea and main bronchi may threaten the life and management of this situation may be challenging.
CONFLICT of INTEREST
None declared.
REFERENCES
-
Yousem SA, Hochholzer L, Malignant fibrous histiocytoma of the lung. Cancer 1987; 60:
2532-41.
[?zet] - Muler JH, Paulino AF, Roulston D, Baker LH. Myxoid malignant fibrous histiocytoma with multiple primary sites. Sarcoma 2002; 6: 51-5. [?zet] [PDF]
- Mounier-Kuhn P. Dilatation de la trachee: constatations radiographiques et bronchoscopiques. Tracheal diatation: radiography and bronchoscopy findings. Lyon Med 1932; 150: 106-9.
- Lund ME, Garland R, Ernst A Airway stenting applications and practice management considerations. Chest 2007; 131: 579-87. [?zet] [Tam Metin] [PDF]
- Ariba? OK, G?rm?? N. Obstructing endobronchial malignant fibrous histiocytoma. Eur J Cardiothorac Surg 2001; 19: 716-8. [?zet] [Tam Metin] [PDF]
-
Alhadab T, Alvarez F, Phillips NJ, Hauptman PJ. Malignant fibrous histiocytoma of the
lung presenting as bronchial obstruction in a heart transplant recipient. J
Heart Lung Transplant 2002; 21: 1140-3.
[?zet] - Aisner SC, Albin RJ, Templeton PA, Krasna MJ. Endobronchial fibrous histiocytoma. Ann Thorac Surg 1995; 60: 710-2. [?zet] [PDF]
- Suri RM, Deschamps C, Cassivi SD, Nichols FC 3rd, Allen MS, Schleck CD, et al. Pulmonary resection for metastatic malignant fibrous histiocytoma: an analysis of prognostic factors. Ann Thorac Surg 2005; 80: 1847-52. [?zet] [Tam Metin] [PDF]
- Tamura S, Imadachi H, Kakugawa T, Toyama H, Kinoshita A, Matsuoka Y, et al. Myxoid type of malignant fibrous histiocytoma in the anterior mediastinum; report of a case Kyobu Geka 2009; 62: 847-9. [?zet]
- Dutau H, Cavailles A, Fernandez-Navamuel I, Breen DP. Tracheal compression in a patient with Marfan's syndrome-associated tracheomegaly treated by an XXL stent: the largest diameter airway stent ever placed in a previously undescribed airway condition. Respiration 2009; 77: 97-101. [?zet]
- Falconer M, Collins DR, Feeney J, Torreggiani WC. Mounier-Kuhn syndrome in an older patient. Age and Ageing 2008; 37: 115-6. [?zet] [Tam Metin] [PDF]
- Menon B, Aggarwal B, Iqbal A. Mounier-Kuhn syndrome: report of 8 cases of tracheobronchomegaly with associated complications. South Med J 2008; 101: 14-5.
- Noori F, Abduljawad S, Suffin DM, et al. Mounier-Kuhn syndrome: a case report. Lung 2010; 188: 353-4. [?zet]
- Genta PR, Costa MVO, Stelmach R, Cukier A. A 26-year-old male with recurrent respiratory infections. Eur Respir J 2003; 22: 564-7. [Tam Metin] [PDF]
- Giannoni S, Benassai C, Allori O, Valeri E, Ferri L, Dragotto A. Tracheomalacia associated with Mounier-Kuhn syndrome in the intensive care unit: treatment with Freitag stent. A case report. Minerva Anestesiol 2004; 70: 651-9. [?zet] [PDF]
Yaz??ma Adresi (Address for Correspondence):
Dr. Levent Dalar,
Yedikule G???s Hastal?klar? ve
G???s Cerrahisi E?itim ve
Ara?t?rma Hastanesi Uyku Laboratuvar?,
Zeytinburnu, ?STANBUL - TURKEY
e-mail: leventdalar@gmail.com