Diyabetik
ketasidozlu hastalarda pulmoner mukormikoz:
Olgu sunumu ve literat?r derlemesi
Afshin
MOHAMMADI1, Alireza MEHDIZADEH2, Mohammad GHASEMI-RAD1,
Homayone HABIBPOUR1, Arefeh ESMAELI3
1 Urmiye ?niversitesi T?p Fak?ltesi, Radyoloji Anabilim Dal?, Urmiye, Bat? Azerbaycan, ?ran,
2 Urmiye ?niversitesi T?p Fak?ltesi, Endokrinoloji ve Metabolizma Anabilim Dal?, Urmiye, Bat? Azerbaycan, ?ran,
3 Urmiye ?niversitesi T?p Fak?ltesi, Patoloji Anabilim Dal?, Urmiye, Bat? Azerbaycan, ?ran.
?ZET
Diyabetik ketasidozlu hastalarda pulmoner mukormikoz: Olgu sunumu ve literat?r derlemesi
Mukormikoz genellikle imm?ns?presif hastalarda g?r?len nadir bir f?rsat?? fungal infeksiyondur.? Mukormikozun, altta yatan veya predispozan duruma ba?l? olarak de?i?en ?ok say?da ba?vuru ?ekli bulunur. Biz, diyabetik ketoasidoz ve pulmoner ve rinoserebral mukormikozlu 56 ya??nda bir olgu sunuyoruz.
Anahtar Kelimeler: Mukormikoz, diabetes mellitus, akci?er.
SUMMARY
Pulmonary mucormycosis in patients with diabetic ketoacidosis: a case report and review of literature
Afshin
MOHAMMADI1, Alireza MEHDIZADEH2, Mohammad GHASEMI-RAD1,
Homayone HABIBPOUR1, Arefeh ESMAELI3
1 Department of Radiology, Faculty of Medicine, Urmia University, Urmia, West Azerbaijan, Iran,
2 Department of Endocrinology and Metabolism, Faculty of Medicine, Urmia University,
Urmia, West Azerbaijan, Iran,
3 Department of Pathology, Faculty of Medicine, Urmia University, Urmia, West Azerbaijan, Iran.
Mucormycosis is a rare opportunistic devastating fungal infection, which usually occurs in immunocompromised patients. Mucormycosis has multiple presentations that the predilection for one of these presentations varies with the either underlying or predisposing condition. We present a case of pulmonary and rhinocerberal mucormycosis in 56-year-old man with diabetic ketoacidosis.
Key Words: Mucormycosis, diabetes melitus, lung.
Geli? Tarihi/Received: 02/03/2011 - Kabul Edili? Tarihi/Accepted: 21/04/2011
Mucormycosis is the name given to several different diseases caused by fungi of the order mucorales. The mucoraceae are ubiquitous fungi that are common inhabitants of decaying matter (bread moulds or decaying vegetable) (1). It is a rare opportunistic devastating fungal infection, which usually occurs in patients with soild organ transplantation, chronic renal failure, patients with neutropenia and those with poorly controlled diabetic (2). The manifestation of mucormycosis can be divided into at least six separate entities; cutaneous, rhino-cerebral, pulmonary, gastrointestinal, central nervous system and disseminated (3). The predilection for one of these presentations varies with the either underlying or predisposing condition. For example, patients with diabetes most often develop rhino-cerebral mucormycosis while neutropenic patients mostly develop pulmonary mucormycosis (4). Disseminated mucormycosis mostly occurs in patients with bone marrow transplants and acute leukemia. We present a case of pulmonary and rhinocerberal mucormycosis in 56-years-old man with diabetic ketoacidosis. To our best knowledge this is the first case of pulmonary and rhinocereberal mucormycosis reported in diabetic patients.
Case report
The patient was a 57-year-old man with 8-year history of diabetes mellitus (DM) under treatment with oral hypoglycemic medication. Patients had poorly controlled diabetes to abruption of his drug from 2 months ago. Patient had developed severe facial pain and paresthesia in the region of upper and lower jaw and headache one day after extraction of second molar tooth. He was referred to the neurologist with the probability of trigeminal neuralgia.
The patient was treated with oral analgesic but had not respond after 24 hour of treatment. The next day patient developed fever, polyuria, polydipsia, vomiting and later on lethargy by which patient was admitted.
On admission the patient was tachypnea (40 per minute), febrile (38.9 degree), had a pulse rate of 105 beats per minute and BP of 110/70 mmHg. While the patient was admitted he developed a seizure attach in the emergency room. All physical examinations were normal except for the mild bleeding at the extracted tooth side. Chest was also clear in auscultation.
Laboratory investigations revealed hemoglobin of 15.7 g/dL, total white blood cell of 17.100 WBC/mm3 (90% neutrophil) and ESR of 23 mm in 1st hour.
Serum biochemistry showed urea 30 mg/dL, creatinine 1.40 mg/dL, blood glucose level was 315 mg/dL, sodium 144 mmoll/L, potassium 4.6 mmol/L, liver enzyme and coagulation pannelwere all within normal range.
The arterial blood gas (ABG) revealed acidosis (pH 7.3, HCO3 10.2 mmol/L). EEG was also normal.
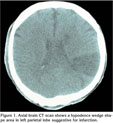
Urine analysis revealed a three plus glucose, the specific gravity was 1030 and three plus keton bodies. Chest X-ray was normal on admission. The computed tomographic (CT) study of brain, which was admitted on admission revealed a wedge shape hypo-dense area in the left parietal lobe without midline shift or hemorrhage, compatible with cerebral infarction (Figure 1).
The patient was transferred to intensive care unit (ICU) and four days later, in spite of the antibiotic therapy and normalization of blood tests and correction of acidosis patient was still complaining of jaw pain and headache and a fever. Patient also developed a left eye pain and the ecchymosis of corresponding eye and pain and erythema of hard palate.
Upon consultation with ophthalmologist and otolaryngologist a CT scan of the orbit and para-nasal sinuses was obtained which revealed opacification of left maxillary and ethmoid sinus without orbital involvement (Figure 2).
The patient was diagnosed with mucormycosis and after administration of amphotricine the otolaryngologist undertook surgical resection of the involved tissue. A left endoscopic maxillectomy was performed. Inferior and middle turbinate were resected due to extensive necrosis of left nasal cavity. Frontal and sphenoid sinuses were free of disease.
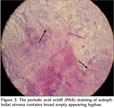
Histopathologic evaluation of resected tissue showed fragments of ciliated respiratory epithelium with underlying stroma, composed of congested and thrombosed dilated vessels and a piece of necrotic tissue plus hemorrhage. The periodic acid schiff (PAS) staining of subepithelial stroma contains broad empty appearing hyphea that are often twisted and collapsed with variable width. These hyphea characteristics are suggestive of mucormycosis (Figure 3).
Ten days laterpatients respiratory distress was worsened. A chest X-ray was obtained, which revealed left sided pleural effusion. We aspirated pleural effusion, which was compatible with exudative pleural effusion.
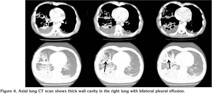
Bronchoscopy was normal and chest CT scan revealed a large thick wall cavity in right middle lobe with nodular and irregular inner borders suggestive of invasive necrotizing pneumonia (Figure 4).
A chest tube was inserted to drain right pleural effusion.
The patient status was deteriorating in spite of treatment and on 20th day after admission developed bradycardia and hypotension and expired due to massive hemoptysis and cardiopulmonary arrest.
Discussion
Mucormycosis is an infection caused by saprophytic fungal agents, which is present in soil, food, air and decaying materials. Most commonly the fungus gains entry to the body through the respiratory tract. The spores are presumably deposited in the nasal turbinate's and maybe inhaled into the pulmonary alveoli. They have filamentous hyphae, mostly non-septetwith right-angledbranching (5). They are usually opportunistic pathogens especially in immuncompromised patients such as; DM, solid-organ-transplant recipients, immunosuppressive therapy and hematologic disorder (1). Neutrophils are prominent components of the host response to the mucorales. It has been well established that hyperglycemia and acidosis predispose the patients to fungal growth (3). Serum obtained from patients with DKA is not inhibitory and may actually enhance fungal growth which can be explained by increase release of iron from transferring in acidosis and enhancementof hyphal growth (4). Like our patient, DM with ketoacidosis is the most common known predisposing factor for mucormycosis.
Mucormycosis can manifest as different clinical forms, namely rhinocerebral, pulmonary, disseminated, gastrointestinal, cutaneous, and other rare forms (2,3,4). The rhino-cerebral forms mainly occurs in patients with diabetes, particularly with the complication DM such as ketoacidosis. They mostly present with facial pain, headache, fever, and mental obtundation (4). Pulmonary mucormycosis present with the clinical features of pneumonia, the sputum might be blood-tinged or grossly bloodyin these patients. Massive hemoptysis has also been reported in isolated case reports and rarely may be fatal (4). Invasion of mucorales to pulmonary vessels and rupture of these vessels into necrotic bronchi may causes asphyxiation as it occurred in our patient (6). Pulmonary mucormycosis commonly involves the upper lobes, which have a better aeration. The endobronchialform is mainly found in patients with diabetes, presenting with bronchial obstruction and hemoptysis (1). A high index of suspicion is needed to avoid delay in diagnosis and treatment. Diagnosis of pulmonary mucormycosis is rarely made ante mortem because of acute nature and need for tissue to confirmdiagnosis (7). The diagnosis of disease is mainly based on history, high index of suspicious, diagnostic imaging and biopsy. Sputum culture is usually unremarkable but a positive culture is highly suggestive. Definite diagnosis requires demonstration of tissue invasion and necrosis with characteristic septet right angle branching hyphae (4).
Radiologic manifestation of mucormycosis may be nonspecific such as; consolidation, cavitery lung lesion and pleural effusion. The most common radiologic findings on chest imaging is consolidation (66%), cavitation occursin about 40% and usually after resolution of neutrophil function and their number like in our patient, radiologic manifestation primarily presented with pleural effusion followed by cavitation after treatment of ketoacidosis (8). Then mucormycosis can also be in a differential diagnosis of other cavitary pulmonary lesion (9).
Over the years intravenous amphotericin B and surgical debridement has been the mainstay of treatment (1,2,3,4). Most of patients with endobronchial form of mucormycosis are diabetic and may benefit from early aggressive surgical resection of involved lung tissue (1). In our patient bronchoscopy and radiologic manifestation did not show endobronchial form and surgical resection was not consideredin treatment.
Teder et al. showed that isolated pulmonary mucormycosis has 65% mortality, but in disseminated form mortality is up to 96% (6).
This case reinforces the concept that occasionally simple intervention such as dental extraction in immune compromised patients can causes fatal complication and awareness of potentially fatal complication such as mucormycosis in these patients may help in rapidly diagnosis and prevention of disease dissemination.
CONFLICT of INTEREST
None declared.
REFERENCES
- Hopkins MA, Treloar DM. Mucormycosis in diabetes. Am J Crit Care 1997; 6: 363-7. [?zet]
- Lewejohann J, Muhl E, Birth M, Kujath P, Bruch HP. Pulmonary zygomycosis--a rare angioinvasive fungal infection. Mycoses 2005; 48(Suppl 1): 99-107. [?zet]
-
Martin-Moro JG, Calleja JM, Garcia MB, Carretero JL, Rodriguez JG. Rhinoorbitocerebral
mucormycosis: a case report and literature review. Med Oral Patol Oral Cir
Bucal 2008; 13: E792-5.
[?zet] - Mandell GL, Dolin R. Principles and Practice of Infectious Disease. 6th ed. Philadelphia: Churchil Livingstone, 2005.
- Auluck A. Maxillary necrosis by mucormycosis a case report and literature review. Med Oral Patol Oral Cir Bucal 2007; 12: E360-4. [?zet]
- Tedder M, Spratt JA, Anstadt MP, Hegde SS, Tedder SD, Lowe JE. Pulmonary mucormycosis: results of medical and surgical therapy. Ann Thorac Surg 1994; 57: 1044-50. [?zet]
- Eucker J, Sezer O, Graf B, Possinger K. Mucormycoses. Mycoses 2001; 44: 253-60. [?zet]
- McAdams HP, Rosado de Christenson M, Strollo DC, Patz EF Jr. Pulmonary mucormycosis: radiologic findings in 32 cases. AJR Am J Roentgenol 1997; 168: 1541-8. [?zet] [PDF]
- Rahimi-Rad MH, Mohammadi A. Multiple bilateral traumatic pulmonary pseuodocysts in a 53 year-old male diagnosed retrospectively. Pneumologia 2010; 59: 84-6. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. Afshin Mohammadi,
Urmia, Modaress BLVD, Imam Hospital
URMIA - IRAN
e-mail: mohamadi_afshin@yahoo.com