Kronik b?brek yetmezli?inde t?berk?lozun de?erlendirilmesi
Aytekin AL?EL?K1, Elif ?ZT?RK2, Zerrin B?C?K3, Mustafa BEH?ET2, Abd?lkadir K???KBAYRAK4
1 Abant ?zzet Baysal ?niversitesi T?p Fak?ltesi, ?? Hastal?klar? Anabilim Dal?, Bolu,
2 D?zce ?niversitesi T?p Fak?ltesi, Mikrobiyoloji Anabilim Dal?, D?zce,
3 SB Kartal E?itim ve Ara?t?rma Hastanesi, Nefroloji B?l?m?, ?stanbul,
4 Abant ?zzet Baysal ?niversitesi T?p Fak?ltesi, ?nfeksiyon Hastal?klar? ve Klinik Mikrobiyoloji Anabilim Dal?, Bolu.
Patients with chronic renal failure (CRF) are at increased risk of tuberculosis. Most of these patients offer extrapulmonary presentation of tuberculosis (TB) (1). The symptomatology in renal patients is often insidious and nonspecific, mimicking uremic symptoms, whereas the localization is often extrapulmonary. Renal physicians should be aware of the unusual presentation and localization, and include TB in the differential diagnosis of any patient having nonspecific symptoms like anorexia, fever, and weight loss (2). We aimed to document the clinical profile, laboratory characteristics and outcome of TB in patients who were followed up in Duzce Medical Faculty Nephrology Department.
MaterialS and Methods
Since May 2002 up to May 2005, we have diagnosed 10 active TB patients. We have diagnosed the presence of TB infection with clinical and/or laboratory findings (microbiological, and/or biochemical, and/or histopathological). Acid-fast bacilli (AFB) examination was carried out by Ziehl-Neelsen stain. Lowenstein-Jensen Medium (Merk, Darmstadt-Germany) and/or Bactec 460 TB system (Becton Dickinson, Cockeysville, USA) were used for isolation of Mycobacterium tuberculosis. Antimicrobial susceptibility tests were performed by Bactec 460 TB system.
Results
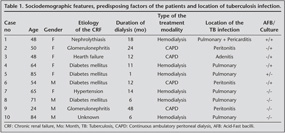
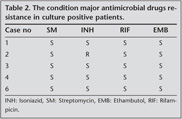
Sociodemographic and clinical features, predisposing factors of the patients and location of TB infection were showed at Table 1. The condition major antimicrobial drugs resistances in culture positive patients were showed at Table 2.
AFB was demonstrated in 2 of the 10 patients, and cultures for M. tuberculosis were positive in 5 of 10. In agreement with other studies from Turkey extrapulmonary TB was as dominant as pulmonary localisation in our affected patients (3,4,5). Pulmonary TB was seen in 5 of 10, pulmonary + extrapulmonary TB infection was seen in 1 of 10 patients and extrapulmonary TB infection was seen in 4 of 10 patients. However, in our patients group, TB was seen in mostly hemodialysis patients, tuberculosis has a great importance in CRF patient regardless treatment modality. In addition, diabetes may be a cofactor for developing TB (4 of 10 TB patients).
Discussion
Over the last few years, there has been a rising trend in the incidence of tuberculosis all over the world (6). Physicians must be alert to unusual presentations and localizations of the disease; TB must be strongly suspected in endemic regions.
Ates G, et al. retrospectively evaluated the frequency of TB in 779 dialysis patients at 13 hemodialysis centers in five different cities in Southeast Turkey. The incidence rate of TB in patients undergoing hemodialysis was 3.1%. Extrapulmonary TB occurred in 45.8% of cases, and the most common site of involvement was the lymph nodes (1). In our patients group, extrapulmonary TB occurred in 40% of cases. However, lymph nodes involvement was seen only 1 patient. Another evaluated the frequency and clinical progression of TB in 18 of 343 dialysis patients diagnosed with TB; extrapulmonary TB was more frequent (77.8%) than pulmonary TB (22.2%) (7).
CRF patients are susceptible to TB, especially to atypical TB with extrapulmonary presentation. Even TB cannot be demonstrated with AFB, M. tuberculosis cultures should be investigated in these populations. Also even if both of these microbiological examinations were negative clinically TB should be kept in mind. The clinical diagnosis may be supported biochemical and histopathological findings and response of the anti-tuberculosis treatment.
CONFLICT of INTEREST
None declared.
REFERENCES
- Ates G, Yildiz T, Danis R, Akyildiz L, Erturk B, Beyazit H, et al. Incidence of tuberculosis disease and latent tuberculosis infection in patients with end stage renal disease in an endemic region. Ren Fail 2010; 32: 91-5. [?zet]
- Hussein MM, Mooij JM, Roujouleh H. Tuberculosis and chronic renal disease. Semin Dial 2003; 16: 38-44. [?zet]
- Taskapan H, Utas C, Oymak FS, Gulmez I, Ozesmi M. The outcome of tuberculosis in patients on chronic hemodialysis. Clin Nephrol 2000; 54: 134-7. [?zet]
- Ozdemir FN, Guz G, Kayatas M, Sezer S, Turan M. Tuberculosis remains an important factor in the morbidity and mortality of hemodialysis patients. Transplant Proc 1998; 30: 846-7. [?zet]
- Cengiz K. Increased incidence of tuberculosis in patients undergoing haemodialysis. Nephron 1996; 73: 421-424.
- Lienhardt C, Sow S. The global challenge of tuberculosis. Lancet 1994; 344: 277-9.
- Sen N, Turunc T, Karatasli M, Sezer S, Demiroglu YZ, Oner Eyuboglu F. Tuberculosis in patients with end-stage renal disease undergoing dialysis in an endemic region of Turkey. Transplant Proc 2008; 40: 81-4. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. Aytekin AL?EL?K,
Abant ?zzet Baysal ?niversitesi T?p Fak?ltesi,
?? Hastal?klar? Anabilim Dal?,
BOLU - TURKEY
e-mail: aytekinalcelik@yahoo.com