Gebelikte spontan pn?motoraks: Olgu sunumu
Afshin MohamMadI1, Mohammad Ghasemi rad2, Kolsoom afrasiabi3
1 Urmiye ?niversitesi T?p Fak?ltesi, Radyoloji Anabilim Dal?, Urmiye, Bat? Azerbaycan, ?ran,
2 Urmiye ?niversitesi T?p Fak?ltesi, ??renci Ara?t?rma Komitesi, Urmiye, Bat? Azerbaycan, ?ran
3 Boschehr ?niversitesi T?p Fak?ltesi, ??renci Ara?t?rma Komitesi, Boschehr, ?ran.
?ZET
Gebelikte spontan pn?motoraks: Olgu sunumu
Gebelik s?ras?nda spontan pn?motoraks olduk?a nadirdir. Gen? gebe kad?nlarda, subplevral apikal b?l veya bleblerin r?pt?r? spontan pn?motoraks?n en s?k nedenleridir. Peripartum d?nemle ili?kili artm?? solunum aktivitesine ba?l? oldu?u d???n?lmektedir. ?lk gebeli?i olan 27 ya??nda spontan pn?motoraksl? bir kad?n hastay? sunuyoruz. Olgu, g???s t?p? ile ba?ar?l? ?ekilde tedavi edildi.
Anahtar Kelimeler: Spontan pn?motoraks, apikal b?l, gebelik.
SUMMARY
Spontaneous pneumothorax in pregnancy: a case report
Afshin MohamMadI1, Mohammad Ghasemi rad2, Kolsoom afrasiabi3
1 Department of Radiology, Faculty of Medicine, Urmia University, Urmia, West Azerbaijan, Iran,
2 Student Research Committee, Faculty of Medicine, Urmia University, Urmia, West Azerbaijan, Iran,
3 Student Research Committee, Faculty of Medicine, Boschehr University, Boschehr, Iran.
Spontaneous pneumothorax is an extremely rare condition during pregnancy. Rupture of a subpleural apical bulla or blebs are the most common cause of spontaneous pneumothorax in young pregnant women. It is believed to be due to increase respiratory activity associated peripartum period. We present 27-year-old primigravid female with spontaneous pneumothorax. She was treated successfully with chest tube placement.
Key Words: Spontaneous pneumothorax, apical bulla, pregnancy.
Case Report
A 27-year-old pregnant women (primigravida, 38 weeks' gestation) referred by a family physician to our hospital due to left-sided pleuritic chest pain. The pain had gradual onset two weeks prior to admission, was accompanied by mild dyspnea on exertion. The pain was exacerbated during last two days and was present even at rest.
She had no history of cough, fever, chills, trauma or hyperemesis gravidarum. Her medical history was unremarkable and had no history of smoking. She had no family history of pulmonary disease.
In physical examination she had mild respiratory distress. Blood pressure was 110/70 mmHg, heart rate 70 beats per minute, respiratory rate 18 breaths per minute, and temperature was 37.3?C. She developed amniotic membrane ruptured on admission with no effacement of Cervix on examination.
The breath sounds were decreased over left chest and on percussion was hyper resonance.
Ultrasound assessment revealed a single fetus with cephalic presentation. The growth parameters were compatible with 38 weeks of gestation, corresponding to a gestational age of 32 weeks.
Emergent posteroanterior (PA) chest radiograph with the abdominal shielded was obtained which revealed a complete pneumothorax of the left lung and shifting of mediastinum and heart to the right hemithorax.
The patient's dyspnea was worsened. A chest tube was placed emergently in the left hemithorax, 5th intercostal space and mid-maxillary line.
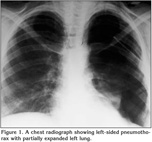
The patient partially improved and a control chest radiograph revealed partial re-expansion of the left lung and an opacity in the expanded left lung due to expansion pulmonary edema (Figure 1).
Emergent cesarean section was performed and a live fetus was delivered.
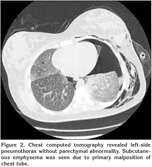
Computed tomography (CT) of the chest was performed after cesarean section that showed extensive pneumothorax with ground glass opacity in semi-expanded left lung without underlying parenchymal abnormality such as; bullae, blebs or cavitary tuberculosis (Figure 2).
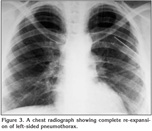
After seven days of chest tube insertion and supportive care, her condition improved and lung re-expansion was achieved (Figure 3).
Discussion
The presence of air in the pleural space is defined as pneumothorax. Spontaneous pneumothorax in pregnancy is extremely rare, with only 57 cases reported in English and other languages till now (1,2,3).
Rupture of a subpleural apical bulla or bleb, pulmonary lymphangiomatosis and cavitary TB are the most common cause of spontaneous pneumothorax in pregnancy (1,4). Spontaneous pneumothorax occurred during the perinatal period in 53.3% and during the first or second trimester in 46.7% of cases (4).
Review of literature showed that the mean age of pregnant women with spontaneous pneumothorax was 26.7 years the same as patients without pregnancy (1,2,3,4,5).
We treated our patient successfully with tube thoracostomy. In the previous collected data of the patients with spontaneous pneumothorax in pregnancy by Garg et al. initial treatment was observation in 29.6%, tube thoracostomy in 66.6%, and in only 3.8% of pregnant patients thoracotomy was performed (1).
Our patient presented with chest pain and dyspnea started two weeks prior to admission. According to previous reports the most common presenting symptom of spontaneous pneumothorax in pregnancy was chest pain and dyspnea (1,2,3,4,5).
Chest radiographs are necessary to confirm diagnosis and the potential risk and benefits associated with a radiologic examination must be compared. It is safe to perform the standard chest radiography when pneumothorax is suspected in a pregnant patient, even during first trimester, if the abdomen is shielded (1).
If it is necessary, shielded CT could also be performed as a useful imaging technique to clarify the underlying pathologic condition and to help in operative planning if indicated (6).
If pneumothorax is diagnosed in a term pregnancy, cesarean section under a general anesthetic should be avoided because the positive pressure ventilation can lead to tension pneumothorax (7). According to previous literature the safest approach for termination is elective assisted deliveries; such as forceps assist delivery to shorten the second stage of delivery. Even if emergent cesarean section is indicated due to obstetric considerations, it should be performed under spinal anesthesia rather than a general anesthesia (8).
The risk of recurrent pneumothorax in these patients is 30-40% particularly during labor (2).
Pulmonary lymphangioleiomyomatosis (LAM) is another differential diagnosis, which should be kept in mind in the young pregnant female presenting with pneumothorax.
In conclusion, although, the rates of pregnancy related pulmonary embolism have been increasing, pneumothorax should be considered in any young pregnant woman with chest pain and/or dyspnea, which should be confirmed radiographically.
CONFLICT of INTEREST
None declared.
REFERENCES
-
Garg R, Sanjay, Das V, Usman K, Rungta S, Prasad R. Spontaneous pneumothorax: an
unusual complication of pregnancy; a case report and review of literature. Ann
Thorac Med 2008; 3: 104-5.
[?zet] [Tam Metin] - Jain P, Goswami K. Recurrent spontaneous pneumothorax during pregnancy: a case report. J Med Case Reports 2009; 3: 81. [?zet] [Tam Metin] [PDF]
- Annaiah TK, Reynolds SF. Spontaneous pneumothorax-a rare complication of pregnancy. J Obstet Gynaecol 2011; 31: 80-2.
- Tanase Y, Yamada T, Kawaryu Y, Yoshida M, Kawai S. A case of spontaneous pneumothorax during pregnancy and review of the literature. Kobe J Med Sci 2007; 53: 251-5. [?zet] [PDF]
-
Wong MK, Leung WC, Wang JK, Lao TT, Ip MS, Lam WK, et al. Recurrent pneumothorax in
pregnancy: what should we do after placing an intercostals drain. Hong Kong Med
J 2006; 12: 375-80.
[?zet] [PDF] -
Van Winter JT, Nichols FC 3rd, Pairolero PC, Ney JA, Ogburn PL Jr.
Management of spontaneous pneumothorax during pregnancy: report and review of
the literature. Mayo Clin Proc 1996; 71: 249-52.
[?zet] - Harris EA. Tension pneumothorax in a parturient undergoing cesarean delivery. Anesth Analg 2000; 90: 1173-4. [?zet] [Tam Metin]
- Lal A, Anderson G, Cowen M, Lindow S, Arnold AG. Pneumothorax and pregnancy. Chest 2007; 132: 1044-8. [?zet] [Tam Metin] [PDF]
Yaz??ma Adresi (Address for Correspondence):
Dr. Afshin MohamMadi,
Urmia, Modaress BLVD, Imam Hospital
Urmia - IRAN
e-mail: mohamadi_afshin@yahoo.com