KOAH'da
semptomun g?nl?k de?i?kenli?ini, sabah aktiviteleri ?zerindeki etkisini ve
hastalar ile fizik tedavi uzmanlar?n?n terap?tik beklentilerini ara?t?rmak i?in
yap?lm??
kesitsel bir g?zlem ?al??mas?-SUNRISE ?al??mas?
T?lin
KuyucU1, Salih Zeki G??l?2, Beng? ?aylan3, Cahit Dem?r4, Tuncer ?enol5, Serdar G?ner6,
Ejder Koyuncu7, Ferit ?zen8, Sezai ?zt?rk9, Zeki Cang?l10, Semih A?ano?lu11, ?evket ?zkaya12,
Sevilay ?i?ek Ocak13, H?seyin Akkurt14, Yavuz Selim ?ntepe15, Merve G?lcan Bayrak16,
Tuncay G?ler17, Taha Tahir Bek??18, ?adan Soyy???t19, Salim Seyfett?n20, ?zhan Kula21,
Makbule ?zlem Akbay22, Beng? B?Y?KG?ZE23, G?khan Asal24, ?eyma Ba?lIlar3, Osman ?zt?rk25
(T?rkiye SUNRISE
?al??ma Grubu; ?al??maya al?nan hasta say?lar?na g?re isimler
s?ralanm??t?r).
1 S?reyyapa?a G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, ?stanbul,
2 ?zel Muayenehane, ?zmir,
3 ?mraniye E?itim ve Ara?t?rma Hastanesi, ?stanbul,
4 ?zel Vizyon Fizik Tedavi ve Rehabilitasyon Merkezi, Ankara,
5 ?zel Muayenehane, ?anl?urfa,
6 Turgutlu Devlet Hastanesi, Turgutlu, Manisa,
7 S?ke Fehime Kocag?z Devlet Hastanesi, S?ke, Ayd?n,
8 ?zel Muayenehane, Denizli,
9 ?stanbul G???s Hastal?klar? Merkezi, ?stanbul,
10 ?zel Muayenehane, ?stanbul,
11 Rize ?ar Hastanesi, Rize,
12 Rize E?itim ve Ara?t?rma Hastanesi, Rize,
13 Esenyurt Devlet Hastanesi, ?stanbul,
14 ?zel Muayenehane, Ankara,
15 Yozgat Devlet Hastanesi, Yozgat,
16 ?ar?amba Devlet Hastanesi, ?ar?amba, Ordu,
17 Bolu ?zzet Baysal Devlet Hastanesi, Bolu,
18 Konya E?itim ve Ara?t?rma Hastanesi, Konya,
19 Mustafa Yaz?c? G???s Hastal?klar? Hastanesi, Aksaray,
20 ?zel Muayenehane, Antakya,
21 ?zel Muayenehane, Bursa,
22 Bilecik Boz?y?k Devlet Hastanesi, Boz?y?k, Bilecik,
23 ?zel Muayenehane, Kocaeli,
24 Antalya ?zel Y?ld?z Andeva Hastanesi, Antalya,
25 Nall?han Devlet Hastanesi, Nall?han, Ankara.
?ZET
KOAH'da semptomun g?nl?k de?i?kenli?ini, sabah aktiviteleri ?zerindeki etkisini ve hastalar ile fizik tedavi uzmanlar?n?n terap?tik beklentilerini ara?t?rmak i?in yap?lm?? kesitsel bir g?zlem ?al??mas?-SUNRISE ?al??mas?
Bu ulusal, ?ok merkezli, kesitsel g?zlem ?al??mas?na, 25 merkezden toplam 514 kronik obstr?ktif akci?er hastal??? (KOAH) olan hasta dahil edildi. Hastalar?n demografik ?zellikleri, e?lik eden hastal?klar, KOAH ?yk?s? ve tedavisi, hasta ve hekimin tedavi beklentisine y?nelik veriler tek bir vizitte topland?. Hastalar?n ya? ortalamas? [standart sapma (SS)]? 64.1 (9.5) y?l; ya? aral??? 41-92 y?l, %50'si 65 ya??n alt?nda ve %91'i erkekti. Hastalar?n %80.2'si en az ilkokul mezunu; %54.3 (%30.4)'?nde kardiyovask?ler hastal?klar ba?ta olmak ?zere en az bir e?lik eden hastal?k bulunuyordu. KOAH hastal?k s?resi ortalama (SS) 5.4 (4.6) y?ld?. Hastalar?n ?o?unlu?u orta (%43.2) ve ?iddetli (%35.0) KOAH evresinde olup, %71'inde y?lda bir veya daha s?k alevlenme tespit edildi. ?nhale beta-2 agonistler (%84.2), inhale steroid (%76.3) ve uzun etkili inhale antikolinerjikler (%70.0) s?kl?kla kullan?lan ila?lard?. Dispne (%99.0), balgam ??karma (%92.8), ?ks?r?k (%92.0) ve h?r?lt?l? solunum (%90.5) olgularda en s?k g?zlenen semptomlar olup, dispne (%41.1), balgam ??karma (%61.0) ve ?ks?r?k (%53.5) en ?ok sabah saatlerinde de?i?kenlik g?steriyordu (p< 0.001). En ?ok etkilenen sabah aktivitesi merdiven inme/??kma (etki puan? 6.7), takiben ?orap/ayakkab? giyme (etki puan? 4.3) ve du? yapma/y?kanma (etki puan? 4.2) idi. Semptomlarda daha fazla rahatlama (%82.3) ve daha fazla hareket edebilme (%70.0), semptomlar?n daha h?zl? iyile?mesi (%61.1) ve sabah aktivitelerinde rahatlama (%59.3) hastalar?n; ya?am kalitesini art?rmak (%100.0) ve morbiditeyi azaltmak (%96.0) ise hekimlerin ba?l?ca tedavi beklentileri idi. Sigara i?meme, alevlenmeyi ?nleme amac?yla en s?k ?nerilen (%88.3) ve uygulanan (%67.9) ila?-d??? koruyucu yakla??md?. Sonu? olarak; bulgular?m?z KOAH'?n sadece ya?l? hastalara ?zg? olmay?p, semptomlar?n hasta ve hekim taraf?ndan atlanmas?na yol a?an yetersiz fark?ndal?k nedeniyle ?o?u zaman hastalar?n g?nl?k ya?amlar?n? bozan ?nemli bir sa?l?k sorunu oldu?una ve hastal?k y?netiminde hastalar?n ya?am ko?ullar?, hayat beklentileri, endi?eleri ve tercihlerini esas alan hasta merkezli yakla??m?n ?nemine i?aret etmektedir.
Anahtar Kelimeler: KOAH, semptomlar, hasta profili, terap?tik beklentiler.
SUMMARY
A cross-sectional observational study to investigate daily symptom variability, effects of symptom on morning activities and therapeutic expectations of patients and physicians in COPD-SUNRISE study
T?lin
KuyucU1, Salih Zeki G??l?2, Beng? ?aylan3, Cahit Dem?r4, Tuncer ?enol5, Serdar G?ner6,
Ejder Koyuncu7, Ferit ?zen8, Sezai ?zt?rk9, Zeki Cang?l10, Semih A?ano?lu11, ?evket ?zkaya12,
Sevilay ?i?ek Ocak13, H?seyin Akkurt14, Yavuz Selim ?ntepe15, Merve G?lcan Bayrak16,
Tuncay G?ler17, Taha Tahir Bek??18, ?adan Soyy???t19, Salim Seyfett?n20, ?zhan Kula21,
Makbule ?zlem Akbay22, Beng? B?Y?KG?ZE23, G?khan Asal24, ?eyma Ba?lIlar3, Osman ?zt?rk25
(Turkey SUNRISE
Study Group; sites are listed in order of number of patients
included).
1 Sureyyapasa Chest Diseases and Chest Surgery Training and Research Hospital, Istanbul, Turkey,
2 Private Office, Izmir, Turkey,
3 Umraniye Training and Research Hospital, Istanbul, Turkey,
4 Private Vizyon Physical Therapy and Rehabilitation Center, Ankara, Turkey,
5 Private Office, Sanliurfa, Turkey,
6 Turgutlu Government Hospital, Turgutlu, Manisa, Turkey,
7 Soke Fehime Kocagoz Government Hospital, Soke, Aydin, Turkey,
8 Private Office, Denizli, Turkey,
9 Istanbul Chest Diseases Center, Istanbul, Turkey,
10 Private Office, Istanbul, Turkey,
11 Rize Sar Hospital, Rize, Turkey,
12 Rize Training and Research Hospital, Rize, Turkey,
13 Esenyurt Government Hospital, Istanbul, Turkey,
14 Private Office, Ankara, Turkey,
15 Yozgat Government Hospital, Yozgat, Turkey,
16 Carsamba Government Hospital, Carsamba, Ordu, Turkey,
17 Bolu Izzet Baysal Government Hospital, Bolu, Turkey,
18 Konya Training and Research Hospital, Konya, Turkey,
19 Mustafa Yazici Chest Diseases Hospital, Aksaray, Turkey,
20 Private Office, Antakya, Turkey,
21 Private Office, Bursa, Turkey,
22 Bilecik Bozoyuk Government Hospital, Bozoyuk, Bilecik, Turkey,
23 Private Office, Kocaeli, Turkey,
24 Antalya Private Yildiz Andeva Hospital, Antalya, Turkey,
25 Nallihan Government Hospital, Nallihan, Ankara, Turkey.
Chronic obstructive pulmonary disease (COPD) is a lung disease characterized with limitation of airflow that is not completely reversible, progressive deterioration of airways and systemic inflammation. This study has been planned to determine daily symptom variability of patients, expectations of patient and physicians from treatment and patient profiles. A total of 514 patients with COPD from 25 centers were included in this national, multicenter, cross-sectional observational study. Data regarding demographic features, concomitant diseases, history and treatment of COPD and expectations of patients and physicians were all obtained in a single visit. Mean [standard deviation (SD)] age of the patients was 64.1 (9.5) years; age range was 41-92 years, 50% of the patients were younger than 65 years and 91% were males. Educational level of the patients was at least primary school in 80.2%; and 54.3% (30.4%) of the patients had at least one concomitant disease, particularly a cardiovascular disease. Mean (SD) duration of having COPD was 5.4 (4.6) years. The majority of patients were at moderate (43.2%) and severe (35.0%) COPD stages and one or more exacerbations per year was determined in 71%. Inhaled beta-2 agonists (84.2%), inhaled steroids (76.3%) and inhaled long-acting anti-cholinergics (70.0%) were the most commonly used medications. Dyspnea (99.0%), sputum production (92.8%) and wheezing (90.5%) were the most common symptoms, and symptom variability for dyspnea (41.1%), sputum production (61.0%) and cough (53.5%) were seen the most in the morning hours (p< 0.001). Most commonly affected morning activity was climbing up/down the stairs (point of effect: 6.7), followed by wearing socks/shoes (point of effect: 4.3) and showering/bathing (point of effect: 4.2) by COPD. Major treatment expectations of patients were greater symptomatic relief (82.3%) and greater mobility (70.0%), faster symptomatic relief (61.1%) and improvement in morning activities (59.3%); while major treatment expectations of physicians included increased quality of life (100.0%) and decreased morbidity (96.0%). Quitting smoking was the most commonly recommended (88.3%) and implemented (67.9%) non-drug protective approach aimed at decreasing the frequency of exacerbations. Consequently, our results demonstrate that COPD is not a disease of only the elderly, is an important healthcare issue that often disrupt daily living of the patients due to inadequate disease awareness leading to overlooking of the symptoms by patient and physicians, and that a patient-centered approach based on the living standards, life expectancies and preferences of patients was crucial in patient management.
Key Words: COPD, symptoms, patient profile, therapeutic expectations.
Chronic obstructive pulmonary disease (COPD) is a progressive and life-threatening chronic lung disease characterized with limitation of airflow that is not completely reversible, progressive deterioration of airways and systemic inflammation, constitutional alterations (reconstruction of airways, emphysema) and mucociliary dysfunction (1,2).
According to World Health Organization (WHO), COPD is estimated to affect 210 million people worldwide, being one of the 12 most common causes of death worldwide and sixth most common cause of death, and it is estimated that COPD will become the third most common cause of death by the year 2030 (3).
COPD is a disease of significant individual, social and economical burden since it burdens patients in terms of symptom characteristics and associated functional limitation much more than the other chronic diseases, and treatment modalities other than quitting smoking provide only very limited symptomatic improvement rather than having an effect on disease progression (2,4,5,6). Additionally, contrary to several diseases leading to death and disability, the prevalence of COPD is expected to gradually increase parallel to the increase in smoking rates in several parts of the world and aging of the population (2).
Therapeutic objectives in the management of COPD include elimination of symptoms, improvement of overall health state, prevention and treatment of exacerbations, slowing down of disease progression and decreasing mortality (7,8). Parameters of treatment success in terms of the patients include symptomatic control that is directly associated with health status, daily living activities, survival and exacerbations (9).
COPD, is often encountered in the 5th decade of life in long-term smokers; however, other risk factors including occupational exposure to dust and chemicals plus in-door pollution secondary to poor ventilation have also been determined; and the disease might also be encountered at younger ages in individuals with serin protease alpha-1 anti-tripsin deficiency, i.e. the best documented genetic risk factor of the disease (2,10,11,12).
The diagnosis of this disease is associated with severe problems including limitation of air-flow which is a long termed process, in addition to often delayed and inadequate detection of disease (13). Another important issue complicating the management of this disease is the inadequacy of disease awareness and therefore delayed referral to physician, since existing symptoms are not often considered to be associated directly with COPD, but rather with smoking or advanced age (14). Similarly, physicians might also ignore the patient leading to delayed diagnosis until the symptoms have progressed significantly (15).
It has been suggested that measurement of pulmonary functions alone might remain inadequate in either demonstrating the burden COPD brings to patients or the efficacy of therapeutic interventions since this examination is not successful in demonstrating the progressive feature of the disease (16,17). Accordingly, the place of clinical and physiological examinations including dyspnea, functional state regarding degree of daily living activities and health state, in determining treatment response is understood better each day (17). Therefore, an examination based on self-reports of patients regarding their symptoms and health state is considered to be indispensible in determining treatment success (9).
Dyspnea, chronic cough, sputum production, wheezing and angina are the most common symptoms of COPD, and patients might also present with minimal symptoms in the early term due to inter-patient variability (2,11). Several screening questionnaires aimed at defining the patients have been developed for use in daily clinical practice; however, despite the significant symptomatic difficulty and functional impairments caused by this disorder, the number of empirical studies aimed at evaluating this disease of high prevalence are quite limited (11,18).
Contrary to the clinical importance of this disease, the number of studies aimed at developing diagnostic and therapeutic strategies has been very low until the last decade. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) that has provided an international consensus on COPD, has determined the preemptive issues regarding COPD and declared phenotypical characteristics and clinical course of the disease as preemptive topics of research (19).
Public information campaigns have been successful in increasing awareness on asthma; however COPD still remains to be a poorly and often falsely known disease; and due to the symptoms patient perceptions and clinical evaluation of physicians often differ significantly (4,20).
Symptoms of COPD including dyspnea have been defined as "persistent and progressive in nature"; however, patients experience "both good and bad days" other than the periods of exacerbation (2). Although symptom variability characterized with fluctuations in symptom during the day, days of the week and over more prolonged periods is one of the main features of COPD, it has not yet been investigated extensively (21,22).
Effects of symptom variability and symptoms on daily activities of the patient should be known and used to aid the disease management of stable COPD by patient needs (23,24,25).
This study has been performed to investigate daily symptom variability, determine effects of symptoms on morning activities, expectations of patient and physicians, the rate of use of non-drug protective approaches aimed at preventing exacerbations and patient profile in COPD and to obtain instructive data regarding the highlights of management of COPD patients in our country.
Materials and methods
This national, multi-centered, cross-sectional study was performed in a total of 25 centers including 15 secondary and three tertiary healthcare institutions and seven physician's offices. A total of 514 newly or previously diagnosed COPD patients referring to the related department and meeting the patient inclusion criteria were included regardless of disease severity. Study centers were selected among the healthcare institutions that were treating a high rate of COPD patients in order to obtain a good cross-section of real-life.
Main inclusion criteria were being diagnosed with COPD and admitted to the study site as an outpatient for any cause, being older than 45 years (> 10 package/years) and providing consent for use of her/his medical data. Main exclusion criteria were ongoing exacerbation or history of exacerbation (deterioration in symptoms of COPD leading to antibiotic and/or short-termed oral steroid therapy and/or hospitalization or referral to emergency department) in the last three months, history of asthma and/or allergic rhinitis, lung presence of severe pulmonary diseases including lung cancer or bronchiectasy, lung fibrosis, interstitial lung disease, tuberculosis, or sarcoidosis, ongoing participation in another interventional clinical study and having already been included in this study once. Approval of the Directorate of Drug and Pharmacy, Ministry of Health was obtained prior to the onset of study procedures and patient's consent to use her/his medical data prior to inclusion of each patient.
There was no follow-up or treatment intervention in this study and data regarding demographic features, concomitant diseases, history of COPD and clinical condition (symptoms, symptom variability, effect of symptoms on daily activities), protective measures against exacerbation of COPD [quitting smoking, dietary limitations (salt, carbohydrate/protein etc.), avoiding crowded places and vaccination against influenza and pneumococci], treatment of COPD, treatment expectations of the patient and physician were obtained directly from the patient, medical records and physician in a single visit.
Statistical Analysis
All patients referring to the study centers within the inclusion period and meeting the inclusion criteria were planned to be included in this observational, cross-sectional study. Accordingly total number of patients was calculated as 500 estimating that 20 patients would be recruited from each center during the inclusion period. A total of 514 patients were included in the study during the patient inclusion period.
Data were expressed as mean [standard deviation (SD)] or n (%). Descriptive statistics were performed regarding the patient profile, COPD symptoms, symptom variability, effect of symptoms on morning activity, protective measures and treatment approaches, and treatment expectations. Patients and patient features, and subgroups of treatments were compared using the Chi-square test. Limit of statistical significance was determined as p< 0.05.
Results
Demographic Features and Concomitant Diseases
Mean age (SD) of study patients was 64.1 (9.5) years; age range was 41-92 years and 50% of the patients were younger than 65 years; about half of these consisting of 40-55 years old patients and 91% consisting of males (Table 1). Only 19.8% of the patients had never been to any school, while 80.2% was at least primary school graduate or higher (Table 1). The majority of patients (70.6%) had smoked previously, but quitted and the remaining patients (29.4%) were current smokers; mean amount of smoking (SD) was 46.5 (24.4) package-years.
There were 279 (54.3%) patients with at least one concomitant disease; the three most common concomitant diseases were cardiovascular diseases (30.4%), sleep disorders (20.2%) and hyperlipidemia (15.8%) (Table 1). Hypertension (n= 97) was reported as the most common cardiovascular disease (Table 1).
History of COPD
Mean duration after the diagnosis of COPD was 5.4 (4.6) years. The diagnosis of COPD had been established within the past year in 79 (15.4%) patients, and earlier than that in the remaining (84.6%) patients. Mean duration (SD) of living with COPD was 8.4 (6.9%) years among patients with history of COPD longer than one year. The diagnosis of COPD had been established following a mean duration (SD) of 5.4 (4.6) years (history shorter than one year in 172 patients (33.5%); equal to or longer than one year in the remaining (66.5%). The majority of patients were in moderate and severe (43.2% and 35.0%, respectively), and the remaining patients were in mild and very severe (9.0% and 12.8%, respectively) COPD stages.
Symptoms of COPD and Daily Symptom Variability
Symptoms of study patients included dyspnea in 99.0%, sputum production in 92.8%, cough in 92.0%, wheezing in 90.5% and tightness in the chest in 81.9%.
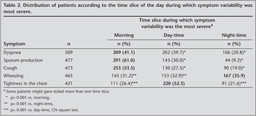
Table 2 demonstrates the peak time of variability of these symptoms during the day. Accordingly, variability in the symptoms of dyspnea (41.1%), sputum production (61.0%) and cough (53.5%) peaked in the morning hours (p< 0.001), whereas wheezing peaked at night (52.3%; p< 0.001), angina peaked during the day (35.9%; p< 0.001).
The most common COPD symptoms encountered in the morning hours was reported as dyspnea by 47.9%, cough by 25.1%, sputum production by 18.9%, wheezing by 4.7% and angina by 4.3% of the patients.
Effect of Symptoms on Morning Activities
Table 3 presents the scores given by patients to evaluate the effect of COPD symptoms on morning activities, aligned from the most extensively affected to no effect. Accordingly, the most adversely affected morning activity is climbing up/down the stairs (point of effect: 6.7), followed by wearing socks/shoes (point of effect 4.3) and showering/bathing (point of effect 4.2) (Table 3).
Treatment of COPD
Patients reported regular use of medications in 75.9%. The most commonly used medications included long-acting inhaled beta-2 agonists (84.2% of the patients), inhaled steroids (76.3% of the patients) and long acting anti-cholinergics (70.0% of the patients). A total of 60.3% of the patients received inhaled steroids + long-acting beta-2 agonists (oral or inhaled) + long acting anti-cholinergics (Table 4).
COPD Exacerbations and Use of Non-Drug Protective Approaches to Prevent Exacerbations
It has been noted that 71% of the patients experienced one or more exacerbations per year, 27.0% of the patients were hospitalized at least once due to exacerbation, referred to the emergency department in 45.3%, and used antibiotics or systemic steroid in higher rates (60.3%) (Table 5).
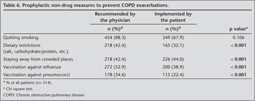
Table 6 demonstrates the rate of use of non-drug protective approaches aimed at preventing COPD exacerbations. Accordingly, quitting smoking was determined as the most commonly recommended and conformed measure. Quitting smoking had been recommended in 88.3% of the patients and 67.9% reported conformation to this recommendation. Significant differences were determined between the rate of recommendation and conformation to all recommendations other than quitting smoking, in favor of reluctance to perform the recommendation (Table 6).
Expectations of Patient and Physicians from
the Treatment
Table 7 summarizes the expectations of patients and physicians from an ideal COPD therapy. Accordingly, most of the patients reported that they expected greater relief of symptoms (82.3%), greater mobility (70.0%), faster improvement in symptoms (61.1%) and improvement in morning activities (59.3%) (Table 7). The main expectations of physicians were to improve quality of life of patients (96.1%), decrease morbidity (92.2%), decrease the rate of episodes (88.5%) and decrease mortality (88.5%) (Table 7).
Discussion
COPD has been defined by the American Thorax Society and European Respiration Association as a preventable and treatable disease characterized with incompletely reversible and progressive limitation of airflow in the lungs associated with an abnormal inflammatory response to toxic particles or gases (19). This definition emphasizes the treatable feature of the disease in terms of improvement of clinical findings and cease of progressive deterioration of lung functions, even if reversibility cannot be obtained with bronchodilators (7,14,26). GOLD consensus report has determined that the main treatment objectives valid in disease management include reduction of risk factors (cease of disease progression, improvement of pulmonary functions, improvement in exercise tolerance), evaluation and monitorization of the patient (improvement in health status, prevention and treatment of exacerbation and complications) and management of stable COPD and exacerbations (reduction of mortality, reduction of side effects of treatment) (26).
Forced expiratory flow rate in 1 seconds (FEV1) and the ratio between this volume and forced vital capacity (FEV1/FVC) are customary measures of pulmonary functioning associated with progressive limitation of airflow; however, recently favored notion is that the clinical course of COPD is also associated with several factors other than impairment of respiratory functions including cellular, organic, functional, clinical and social factors and therefore effective monitorization should be performed in terms of symptoms, exercise tolerance, quality of life and conformation to therapy (27,28). Accordingly, the COPD staging system developed by Celli et al. includes FEV1 in addition to dyspnea, 6 minutes walking distance and body mass index (29).
IBERPOC prevalence study has demonstrated that the development of COPD was more likely in male patients who smoked heavily, lived in the urban, presented with symptoms of chronic bronchitis, were older than 60 years (30). However, an analysis has been performed since 21.7% of the patients have previously been diagnosed with COPD and demonstrated that the possibility of establishment of a diagnosis was greater in patients aged between 55-64 years, presenting with wheezing, having another diagnosis of chronic respiratory disease and presenting with severe deterioration in terms of both lung functioning and quality of life (31). Therefore, it has been emphasized that the rate of suspecting COPD was rather low among physicians and the complaints of cough and sputum production that are common among smokers were considered natural and easily overlooked by both patient and physicians (31). The general notion that COPD prevalence is higher among male patients with history of heavy smoking has been confirmed in our study consisting of male patients in great majority (32). Contrary to the notion that COPD principally develops in elderly patients with long-termed history of smoking (10), our study data has demonstrated that this is a disease of the active individuals since 50% of study patients were younger than 65 years and almost half of these were younger than 40-55 years.
Similar to the literature reports stating that the most common symptoms of COPD include chronic cough, sputum production, wheezing and angina (2), 99.0% of our study patients presented with dyspnea, 92.0% with cough, 92.8% with sputum production, 90.5% with wheezing and 81.9% with angina (2).
Respiratory symptoms associated with COPD have similar prevalence in males and females ranging between 6 to 61 percent; however, the presence of symptoms is significantly associated with impairment in pulmonary functioning only in male patients (32). Interestingly, about half of the COPD patients had been diagnosed with severe or very severe COPD and duration of one year or longer had passed between the onset of symptoms and establishment of diagnosis in 66.5% of the patients in our study population consisting mainly of males.
A nihilistic approach is followed by healthcare providers due to the lack of a pharmacotherapeutic alternative to prevent disease progression and by patients due to hesitation of quitting smoking and adaptation to their functional limitations (26).
Questioning quality of life to increase the odds of early diagnosis of COPD and evaluating treatment response as a parameter associated with first referral, following referrals and mortality are crucial (31).
There is a complex relationship between health related quality of life (HRQoL) and functional state, and progression of COPD leads to physical deterioration and avoidance of daily living activities starting from the ones necessitating great effort (33).
Perception of an individual regarding his own clinical condition is directly associated with survival (34). One study evaluating the individual perceptions of COPD patients has demonstrated that disease severity is associated with more adverse healthcare events in males, whereas the main factor affecting disease scores was determined as perceptions of control in females (34).
Additionally, dyspnea, which is the main symptom of COPD is not directly related with the global health status; however, perception of fatigue has become an independent parameter of global health scores. This has been interpreted as the fact that similar to dyspnea, the perception of fatigue is a common perception deemed quite disturbing by the patients, with its degree increasing parallel to other symptoms (34).
Knowledge of the effect of symptom variability and effect of symptoms on daily activities of patients is a guiding parameter in the management of stable COPD and beneficial in manipulating the disease management process by the needs of the patient. A very novel observational study performed in the Europe has demonstrated that patients diagnosed with severe COPD often experienced symptom variability particularly in the symptoms of angina and dyspnea on weekly and daily basis, despite stabilization with effective therapies; and that patients with severe stable COPD perceived the weekly and daily variability in symptoms (23,24). In the study of Partridge et al. published in 2009 the majority of patients complained of the effect of COPD on morning activities, and therefore recommended physicians to question patients particularly in this respect (25). Similarly, we determined that dyspnea, sputum production and cough were the symptoms with greatest morning variability, angina was the symptom with the greatest daily variability and wheezing was the symptom with greatest nighttime variability. The most common COPD symptoms observed in the morning hours include dyspnea, cough, sputum production, wheezing and angina.
The most commonly affected morning activities of COPD patients were climbing up/down the stairs (point of effect 6.7), wearing socks/shoes (point of effect 4.3), showering/bathing (point of effect 4.2) and making the bed (point of effect 3.7).
Public information campaigns have been successful in increasing awareness on asthma; however COPD still remains to be a poorly and often falsely known disease (4); and due to the symptoms patient perceptions and clinical evaluation of physicians often differ significantly (20). Knowledge of patients' treatment expectations might provide better understanding of their priorities and lead the way to novel clinical studies (35).
Studies have demonstrated that adverse perceptions regarding the disease in addition to belief in future death due to the disease were more frequent among elderly patients compared to the younger patients with less concomitant disorders and greater rate of active smoking (35). Additionally, another study has demonstrated that patients tended to ignore their real morbidities, there was a significant discrepancy between the disease severity and the perceptional disease severity, and therefore it was crucial to determine treatment expectations of the patients (4).
The most important point in COPD has been reported to be the effect of disease on normal daily living activities that increased particularly during periods of exacerbation and rapid symptomatic relief (35). Similarly, the majority of our patients reported that they expected to experience greater relief (82.3%), greater mobility (70.0%), faster improvement of symptoms (61.1%) and improvement in morning activities (59.3%).
Observational studies performed with COPD patients in primary healthcare facilities have reported that annually patients experienced about two exacerbations and these exacerbations led to acceleration of the deterioration of pulmonary functions and regression in quality of life (35). Similarly, one or more exacerbations were reported per year in 71% of our study population; no exacerbations were observed in the last one year only in 29.0%; and 3 or more exacerbations were observed in 13.2%.
Treatment expectation to experience faster symptomatic improvement observed in our patient population was compatible with the literature (35). Therefore, choosing an antibiotic in the treatment of infective exacerbations should provide favorable results both in terms of rapid treatment of symptoms and prolongation of the duration in between exacerbations (36,37).
COPD patients are less mobile in their daily lives compared to their healthy peers and this lack of mobility becomes the most marked during periods of exacerbation (35). Parallel to that, greater mobility ranked among the first in the list of treatment expectations of the majority of our study population. However, major treatment expectations of physicians included increasing the quality of life (100.0%), decreasing morbidity (96.0%), decreasing the rate of episodes (92.1%) and mortality (92.1%) and loss of condition was reported as a treatment expectation by the majority of physicians (70.9%). Although physicians' expectations to increase the quality of life is compatible with that of patients; patients have greater anxiety for future events and physicians should deem both their own and patients expectations as priorities.
Time spent outside of house has positive effects on healthcare status and physical activity decreases the rate of re-referral to hospital and severe exacerbations. Obviously, strategies aimed at increasing the level of physical activity of COPD patients should have positive effects on survival (27,36). The most practical approach to evaluate and follow exercise capacity of COPD patients seems to be questioning the patients in this respect during consultation (26).
Pulmonary inflammation and systemic inflammation increase the prevalence of concomitant diseases including cardiovascular diseases (coronary artery disease, congestive heart failure, and other cardiovascular diseases), local malign neoplasm, neurological diseases, ulcer and gastritis among COPD patients (38). Compatible with the literature concomitant diseases were observed in 54% of our patients consisting of cardiovascular diseases in one third.
Literature studies have demonstrated that there was a significant difference not only in terms of treatment expectations, but also in perception between patient and physicians in terms of the annual number of COPD exacerbations and mean duration of an exacerbation, suggesting that physicians provide more optimistic figures (35).
Current guidelines suggest the use of long-acting inhaler bronchodilators in the management of symptomatic moderate and severe COPD and addition of inhaler corticosteroids to this treatment in patients experiencing repetitive exacerbations (9).
Bronchodilators used in the treatment of COPD include beta-2 agonists (short and long acting), anticholinergics (short and long acting) and methylxantines (2). Long termed studies performed on great patient populations have suggested that long acting beta-2 agonist, inhaler corticosteroid combinations reduce the symptoms, increase exercise tolerance, improve quality of life, decrease the number of episodes, decrease the number of deaths due to cardiovascular diseases (ISOLDE study), reduce the incidence of cardiovascular events (TORCH) and deaths due to COPD (ISOLDE), and slow down functional progression in lung functioning. Addition of a long acting anti-cholinergic to the treatment has also provided an improvement in quality of life, reduction in the number of episodes and decrease in mortality (UPLIFT). According to the frequently used guidelines, addition of inhaler corticosteroids to bronchodilator therapy is recommended in symptomatic COPD patients experiencing repetitive exacerbations (2). Accordingly, the most frequently used medications in our study population have been determined as long acting beta-2 agonists (by 84.2% of the patients), inhaler steroids (by 76.3% of the patients) and long acting anticholinergics (by 70.0% of the patients). Quitting smoking and indeed preventing the onset of the habit of smoking is not only a parameter of patient level, but also the most important parameter of economic and social levels, and out of all the known treatment modalities (ICS/LABA fix combination has led to a loss in annual FEV1 in COPD patients with FEV1< 60%, Celli study, TORCH, and GOLD guidelines have reported that ICS/LABA fix combination slowed down the progression), only quitting smoking has been effective in decreasing the rate of reduction in FEV1 (26). Accordingly, we investigated the rate of use of non-drug protective approaches by the patients in preventing COPD exacerbations and determined that quitting smoking was the most commonly recommended (88.3%) and conformed (67.9%) approach. Dietary limitation and keeping away from crowded places have been recommended in 42.4% of the patients and the latter has been more preferred by the patients (32.1% and 44.0%, respectively). Influenza vaccination, was both more commonly recommended by physicians (52.9 and 34.6%, respectively) and performed by patients (38.9% and 22.4%, respectively) compared to pneumococci vaccination. Currently used COPD guidelines are more FEV1 (stages of GOLD) and medicine treatment based rather than being based on clinical parameters including dyspnea, cough and reduced exercise tolerance (26).
The commonly used BTS (38), ATS/ERS (7) and GOLD (18) guidelines should be improved for more effective patient management and national guidelines based on these improved versions should be prepared in order to be able to treat COPD that brings a significant burden both to patients and healthcare system and population (26).
Although there is no easily applicable monitorization parameter in the clinical management of COPD, it has been reported that parameters of hyperinflammation, symptoms, exercise intolerance, nutritional status and exacerbations should be measured correctly and evaluated indirectly for proper follow up of patients (26).
Consequently, our results demonstrated that COPD is not only a disease of the elderly, is a significant healthcare problem disrupting the daily living of patients due to inadequate awareness leading to overlooking of symptoms by both patient and physicians and that a patient centered approach should be followed based on patients' living conditions, life expectancies, anxieties and preferences. The main objective of treatment should be enabling patients to continue their active living and feel better. Accordingly, COPD management requires a multidisciplinary approach aimed at the extrapulmonary components that might affect the symptomatology in chronic diseases markedly; patients' symptoms, status of health, quality of life and treatment expectations should be questioned in addition to pulmonary function parameters in the processes of early diagnosis, effective treatment and monitorization; the treatment should be planned according to the clinical picture of the patient and guidelines reflecting the treatment expectations of both patient and physicians, and covering long term health, social and palliative support.
Acknowledgement and CONFLICT of INTEREST
This study has been performed under the sponsorship of Astra-Zeneca Turkey and medical writing support was obtained from Cagla Isman, M.D. and Sule Oktay, M.D., Prof. from Kappa Consultancy Education and Research Company (Istanbul) sponsored by Astra-Zeneca Turkey.
REFERENCES
- Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007; 176: 532-55. [?zet] [Tam Metin] [PDF]
- Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of Chronic Obstructive Pulmonary Disease. Executive Summary 2006.
- WHO. World Health Organization. Chronic respiratory diseases. Chronic obstructive pulmonary disease (COPD). 2010 [updated 2010; cited 2 June 2010]; Available from http://www.who.int/respiratory/copd/en/
- Rennard S, Decramer M, Calverley PMA, Pride NB, Soriano JB, Vermeire PA, et al. Impact of COPD in North America and Europe in 2000: subject's perspective of Confronting COPD International Survey. Eur Respir J 2002; 20: 799-805. [?zet] [Tam Metin] [PDF]
- Walke LM, Gallo WT, Tinetti ME, Fried TR. The burden of symptoms among community-dwelling older persons with advanced chronic disease. Arc Int Med 2004; 164: 2321-4. [?zet] [Tam Metin] [PDF]
-
Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest 2000; 117(Suppl 2):
5-9.
[?zet] [Tam Metin] [PDF] - Celli BR, MacNee W. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004; 23: 932-46. [Tam Metin] [PDF]
- GOLD. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. 2009 [updated 2009; cited 2 June 2010]; Available from http://www.goldcopd.org/Guidelineitem.asp?l1=2&l2=1&intId=2003
- Stull DE, Wiklund I, Gale R, Capkun-Niggli G, Houghton K, Jones P. Application of latent growth and growth mixture modeling to identify and characterize differential responders to treatment for COPD. Contemp Clin Trials. 2011 [Epub ahead of print] doi:10.1016/j.cct.2011.06.004. [?zet]
- American Thoracic Society. Standards for the diagnosis and care of patients with Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 1995; 152: 77-120.
- Cazzola M, Donner CF, Hanania NA. One hundred years of chronic obstructive pulmonary disease (COPD)-Republished article. Respir Med 2008; 4: 8-25.
- Stoller JK, Aboussouan LS. Alpha1-antitrypsin deficiency. Lancet 2005; 365: 2225-36. [?zet]
- Ant? JM, Vermeire P, Vestbo J, Sunyer J. Epidemiology of chronic obstructive pulmonary disease. Eur Respir J 2001; 17: 982-94. [?zet] [Tam Metin] [PDF]
- van Schayck CP, Loozen JM, Wagena E, Akkermans RP, Wesseling GJ. Detecting patients at a high risk of developing chronic obstructive pulmonary disease in general practice: cross sectional case finding study. BMJ 2002; 324: 1370-4. [?zet] [Tam Metin] [PDF]
- Murray CJL, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet 1997; 349: 1498-504. [?zet]
-
Cazzola M, MacNee W, Martinez FJ, Rabe KF, Franciosi LG, Barnes PJ, et al. Outcomes for
COPD pharmacological trials: from lung function to biomarkers. Eur Respir J
2008; 31: 416-69.
[?zet] [Tam Metin] [PDF] - Jones P, Lareau S, Mahler DA. Measuring the effects of COPD on the patient. Respir Med 2005; 99(Suppl B): 11-8. [?zet]
- Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS, GOLD Scientific Committee. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001; 163: 1256-76. [Tam Metin] [PDF]
- Ries AL. Impact of chronic obstructive pulmonary disease on quality of life: the role of dyspnea. Am J Med 2006; 119 (10A): S12-S20. [?zet]
- Williams SJ. Chronic respiratory illness. In: Titzpatrick R, Newman S (eds). The Experience of Ilness Series. London: Routledge, 1993.
- Gilbert C, Martin ML, Hareendran A, Bushnell DM, Patrick DL, Sch?nemann HJ. Capturing Individual Variation in the Experience of Symptoms Reported by Patients with COPD. Poster ATS 2007.
-
Kessler R, Cazzola M, Miravitlles M, Partridge MR, Vogelmeier C, Leynaud D, et al.
Variability of symptoms is common in severe COPD: a pan-European
cross-sectional study. European Respiratory Society, Annual Congress, Vienna
Sept 12-16, 2009 [Eur Resp J 2009; 34(Suppl 53)].
[?zet] [Tam Metin] [PDF] - Partridge MR, Cazzola M, Kessler R, Miravitlles M, Vogelmeier C, Leynaud D, et al. Diurnal variation of symptoms and impact on morning activities in severe COPD: a pan-European cross-sectional study. European Respiratory Society, Annual Congress, Vienna Sept 12-16, 2009 [Eur Resp J 2009;34(Suppl 53)].
- Partridge MR, Karlsson N, Small IR. Patient insight into the impact of chronic obstructive pulmonary disease in the morning: an internet survey. Curr Med Res Opin 2009; 25: 2043-8. [?zet]
- Van Schayck CP, Bindels PJE, Decramer M, Dekhuijzen PNR, Kerstjens HAM, Muris JWM, et al. Making COPD a treatable disease-an integrated care perspective. Respir Med 2007; 3: 49-56.
- Garcia-Aymerich J, G?mez FP, Ant? JM; en nombre del Grupo Investigador del Estudio PAC-COPD. Phenotypic characterization and course of chronic obstructive pulmonary disease in the PAC-COPD Study: design and methods. Arch Broncopneumol 2009; 45: 4-11. [?zet]
- Bellamy D, Bouchard J, Henrichsen S, Johansson G, Langhammer A, Reid J, et al. International primary care respiratory group (ICPRG) guidelines: management of chronic obstructive pulmonary disease (COPD). Prim Care Respir J 2006; 15: 48-57. [?zet] [PDF]
- Celli BR, Cote DG, Mar?n JM, Casanova C, Montes de Oca M, M?ndez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med 2004; 350: 1005-12. [?zet] [Tam Metin] [PDF]
- Sobradillo Pena V, Miravitlles M, Gabriel R, Jime?nez-Ruiz CA, Villasante C, Masa JF, et al. Geographical variations in prevalence and underdiagnosis of COPD. Results of the IBERPOC multicentre epidemiological study. Chest 2000; 118: 981-9. [?zet] [Tam Metin] [PDF]
- Miravitlles M, Ferrer M, Pont A, Luis Viejo J, Fernando Masa J, Gabriel R, et al. Characteristics of a population of COPD patients identified from a population-based study. Focus on previous diagnosis and never smokers. Respir Med 2005; 99: 985-95. [?zet]
- Watson L, Vonk JM, L?fdahl CG, Pride NB, Pauwels RA, Laitinen LA, et al; European Respiratory Society Study on Chronic Obstructive Pulmonary Disease. Predictors of lung function and its decline in mild to moderate COPD in association with gender: results from the Euroscop study. Respir Med 2006; 100: 746-53. [?zet]
- Voll-Aanerud M, Eagan TM, Wentzel-Larsen T, Gulsvik A, Bakke PS. Respiratory symptoms, COPD severity, and health related quality of life in a general population sample. Respir Med 2008; 102: 399-406. [?zet]
- Nguyen HQ, Donesky-Cuenco D, Carrieri-Kohlman V. Associations between symptoms, functioning, and perceptions of mastery with global self-rated health in patients with COPD: a cross-sectional study. Int J Nurs Stud 2008; 45: 1355-65. [?zet]
- Miravitlles M, Anzueto A, Legnani D, Forstmeier L, Fargel M. Patient's perception of exacerbations of COPD-the PERCEIVE study. Respir Med 2007; 101: 453-60. [?zet]
- Miravitlles M, Llor C, Naberan K, Cots JM, Molina J. Variables associated with recovery from acute exacerbations of chronic bronchitis and chronic obstructive pulmonary disease. Respir Med 2005; 99: 955-65. [?zet]
- Wilson R, Jones P, Schaberg T, Arvis P, Duprat-Lomon I, Sagnier PP. Antibiotic treatment and factors influencing short and long term outcomes of acute exacerbations of chronic bronchitis. Thorax 2006; 61: 337-42. [?zet] [Tam Metin] [PDF]
- Wouters EF, Breyer MK, Rutten EP, Graat-Verboome L, Spruit MA. Co-morbid manifestations in COPD. Resp Med 2007; 3: 135-51.
- The National Collaborating Centre for Chronic Conditions. National clinical guideline on management of COPD in adults in primary and secondary care. Thorax 2004; 59(Suppl 1): 1-232.
Yaz??ma Adresi (Address for Correspondence):
Dr. T?lin Kuyucu,
SB S?reyyapa?a G???s Hastal?klar? ve
G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi,
2. G???s Hastal?klar? Klini?i,
Ba??b?y?k Mahallesi
34844 Maltepe ?STANBUL - TURKEY
e-mail: tnkuyucu@yahoo.com