Wilms t?m?r?n?n ba?vuru semptomu olarak rek?rren pulmoner t?mor embolisi ve ani ?l?m
Afshin MOHAMMADI
Urmiye ?niversitesi T?p Fak?ltesi, Radyoloji Anabilim Dal?, Urmiye, Bat? Azerbaycan, ?ran.
?ZET
Wilms t?m?r?n?n ba?vuru semptomu olarak rek?rren pulmoner t?mor embolisi ve ani ?l?m
B?brek t?m?rl? ?ocuklar?n sadece %4-6?s?nda ba?vuru s?ras?nda inferior vena kava veya sa? atriyal infiltrasyon bulunmaktad?r. T?m?r embolisi daha nadirdir ve Wilms t?m?r?nde ba?vuru semptomu olarak ani ?l?m ?imdiye kadar sadece sekiz olguda bildirilmi?tir. K???k pulmoner emboli ile ba?vuran ve sonras?nda masif pulmoner emboliye ba?l? ani ?l?m geli?en nadir bir Wilms t?m?rl? olguyu sunuyoruz. Tan? s?ras?nda, stabil hemodinami ve invaziv vask?ler infiltrasyonlu hastalarda acil cerrahi gerekli olabilir gibi g?r?nmektedir.
Anahtar Kelimeler: Wilms t?m?r?, pulmoner emboli, ani ?l?m.
SUMMARY
Recurrent pulmonary tumoral embolism and sudden death as the presenting symptom of Wilms? tumor
Afshin MOHAMMADI
Department of Radiology, Faculty of Medicine, Urmia University, Urmia, West Azerbaijan, Iran.???????
Only 4-6% of children with renal tumor show inferior vena caval or right atrial infiltration at presentation. Tumor emboli are even rarer, and so far, sudden death as the presenting symptom has only been described at presentation in Wilms? tumor in eight cases. We report a unique case of Wilms? tumor that presented with small pulmonary emboli and immediately after asthatwas diagnosed before deathby detection of small emboli and immediately after sudden death as massive pulmonary embolism. It seems that in cases of invasive vascular infiltration with a stable hemodynamic condition at diagnosis immediate surgery may be necessar
Key Words: Wilms? tumor, pulmonary embolism, sudden death.
Wilms? tumor is the most common urinary tract neoplasm of childhood (1). Only 4-6% of children with renal tumor show inferior vena caval (IVC) or right atrial infiltration at presentation (2,3,4). However, up to 40% of Wilms tumors have invaded the renal vein by the time of diagnosis (3). Tumor emboli are even rare, and sudden death as presenting symptom has only been described at presentation in WT in 8 cases so far (2). Although pulmonary metastases may already be present in up to one fourth of cases at the time of initial diagnosis, it is exceedingly rare for pulmonary emboli to develop as a first manifestation of WT (5,6). We report a unique case of recurrent pulmonary emboli that was diagnosed premortem by detection of small emboli and after sudden death due to massive pulmonary embolism.
CASE REPORT
A 8-year-old boy was in his usual state of good health until the day of admission when after vomiting he became pale and complained of shortness of breath.
Both lungs were clear to auscultation but in inspection mild intercostal retractions were obvious. Abdomen was distended and a firm abdominal mass was palpable at left side of abdomen measuring 10 x 10 cm that did not across through the midline of abdomen.
During first day of admission Arterial Blood Gas and other Laboratory data such as CBC & ESR, BUN, Cr, Na, K & PH was normal but there was microscopic hematuria in Urine analysis (8-10 RBC/hpf).
Chest X-ray was obtained at admission and showed mild right side pleural effusion without pulmonary consolidation or nodular opacity Figure 1.
Abdominal ultrasonography revealed a large well marginated hypoechoeic mass arising from lower pole of left kidney.
24 hours after admission the patient became tachypenic and complains from exacerbation of shortness of breath and chest pain.
In physical examination there was respiratory distress and intercostal retractions on inspection and pulmonary rales in right lower lobe of right lung on auscultation. Chest and abdominal computed tomography (CT) scan with intravenous and oral contrast was performed for further evaluation of abdominal mass and respiratory problem.
Chest CT showed several pleural based pulmonary nodules and a wedge shape confluence of perivascular pulmonary nodules in the right lower lobe of right lung and with lesser extend in left lower lobe (Figure 2). Chest CT also showed a filing defect that extended from IVC to right atrium (Figure 3), and small filing defect in the right pulmonary artery (Figure 4).
Abdominal CT with intravenous and oral contrast showed a huge left renal mass extending into left renal vein and IVC (Figure 5).
After 36 hours of admission the patient suddenly collapsed. Unfortunately, resuscitation was not successful.
Autopsy confirmed the diagnosis and showed a large left renal mass extending into left renal vein and inferior vena cava up to right atrium accompanying with a saddle mixed tumor and clot emboli in pulmonary artery bifurcation (Figure 6).
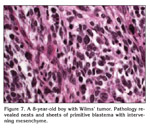
Histology revealed nephroblastoma, with diffuse anaplasia, stage 3.
DISCUSSION
WT is one of the most common tumors in infants and children. WT typically is manifested as an asymptomatic abdominal mass or abdominal pain, fever and hematuria (7).
WT is one of the successes of pediatric oncology, with an overall cure rate of over 85%, using relatively simple therapies. This excellent outcome has been the result of collaborative efforts among surgeons, pediatricians, pathologists and radiation oncologists. The results that have been achieved in children with WTs support the strong value of the multidisciplinary team approach to cancer (8).
The initial pulmonary tumor emboli causing sudden death as presenting symptom has only described at presentation in WT in 8 cases so far as Table 1 (2).
The low reported incidence of intravascular extention of tumor thrombosis (4-6%) may be due to imaging difficulties in the past years (24). In adults, sudden deaths have been reported in 11 cases associated with malignancies, like broncogenic carcinoma, pancreatic carcinoma, leukemia, gastric carcinoma, thyroid carcinoma, urinary bladder carcinoma, astrocytoma, and only once with renal tumor (9).
Pulmonary embolism in children and infants is one of the difficult diagnoses to make on the basis of clinical finding.
As WT patients often present without any symptom, it is unlikely to prevent from sudden death due to pulmonary tumor embolism as presenting symptom.
Most tumor cells which reach the lungs become trapped within pulmonary capillaries, many malignant cell trigger the coagulation cascade, obstruction of pulmonary vessels usually result from the presence of both tumor cells and associated clot. This secondary change may produce complete and irreversible obstruction of pulmonary vessels.
Some authors believe that a presumptive diagnosis, based an atypical presentation and exclusion of thromboembolic disease is adequate. Massive tumor emboli are a rare cause of acute respiratory distress in children. Five patients from case of WT embolization to the lung have been reported that occurred during intraoperative manipulation.
Although, it has been shown that chemotherapy before surgery downstages the WT and reduces the risk of tumor ruptures, it is clear that treatment decisions should be made based on the characteristics and stability of the individual patients especially for those with cardiac involvement (10).
CT scan is a valuable method for examining renal vein, IVC and right atrial invasion by WT.
This case demonstrate that WT can embolize preoperatively. We conclude that death due to pulmonary tumor emboli in pediatric renal tumors is rare and in the cases of invasive vascular infiltration at diagnosis with stable hemodynamic condition immediate start of surgery may be necessary.
CONFLICT of INTEREST
None declared.
REFERENCES
- Jia HM, Zhang KR, Shu H, Tian BL, Wang WL. Presacralextrarenal Wilms? tumor in a child. Urology 2009; 74: 308-10. [?zet]
- van den Heuvel-Eibrink MM, Lankhorst B, Egeler RM, Corel LJ, Kollen WJ. Sudden death due to pulmonary embolism as presenting symptom of renal tumors. Pediatr Blood Cancer 2008; 50: 1062-4. [?zet]
- Ceelen W, Kerremans I, Lutz-Dettinger N, Vandenbroeck P, de Hemptinne B. Wilms? tumour presenting as a pulmonary embolism. Acta Chir Belg 1997; 97: 148-50. [?zet]
- Giannoulia-Karadana A, Moschovi M, Koutsovitis P, Tolis G, Tzortzatou-Stathopoulou F. Inferior vena cava and right atrial thrombosis in children with nephroblastoma: diagnostic and therapeutic problems. J Pediatr Surg 2000; 35: 1459-61. [?zet]
- Zakowski MF, Edwards RH, McDonough ET. Wilms? tumor presenting as sudden death due to tumor embolism. Arch Pathol Lab Med 1990; 114: 605-8. [?zet]
- Bulas DI, Thompson R, Reaman G. Pulmonary emboli as a primary manifestation of Wilms? tumor. AJR Am J Roentgenol 1991; 156: 155-6. [?zet]
- Castellino SM, Martinez-Borges AR, McLean TW. Pediatric genitourinary tumors. Curr Opin Oncol 2009; 21: 278-83. [?zet]
- Spreafico F, Bellani FF. Wilms? tumor: past, present and (possibly) future. Expert Rev Anticancer Ther 2006; 6: 249-58. [?zet]
- Oeberst JL, Bernard JJ, Prahlow JA. Sudden death due to undiagnosed Wilms? tumor in adult. J Foresnic Sci 2002; 47: 638-9. [?zet]
- Pritchard-Jones K, Pritchard J. Success of clinical trials in Childhood Wilms? tumor around the world. Lancet 2004; 364: 1468-70.
Yaz??ma Adresi (Address for Correspondence):
Dr. Afshin MOHAMADI,
Urmia, Modaress BLVD, Imam Hospital
URMIA - IRAN
e-mail: mohamadi_afshin@yahoo.com