Mediasteni invaze eden endobron?iyal inflamatuvar ps?dot?m?r olgusu
Ebru SULU, Ebru DAMADO?LU, Huriye BERK TAKIR, Hacer KUZU OKUR, Esra K?RO?LU, Adnan YILMAZ
1 SB S?reyyapa?a G???s Hastal?klar? ve G???s Cerrahisi E?itim ve Ara?t?rma Hastanesi, ?stanbul.
?ZET
Mediasteni invaze eden endobron?iyal inflamatuvar ps?dot?m?r olgusu
?nflamatuvar ps?dot?m?r, t?m akci?er t?m?rlerinin %1'den daha az?n? olu?turur. Endobron?iyal lokalizasyon, olgular?n % 12'sinden daha az?nda g?r?l?r. Bu t?m?rler mediastinal yap?lara invazyon g?sterebilir. Bu yaz?da, mediastene invazyon g?steren endobron?iyal inflamatuvar ps?dot?m?r olgusunu sunduk. Elli ya??nda erkek hasta, ?? ayd?r devam eden ?ks?r?k ve kanl? balgam yak?nmalar? ile Mart 2007 tarihinde merkezimize ba?vurdu. Arka-?n akci?er grafisinde sa? ?st zonda opasite saptand?. Sigara al??kanl??? d???nda ?z ge?mi?inde bir ?zellik yoktu. Tam kan say?m?, idrar tahlili ve biyokimyasal incelemeler normal s?n?rlarda idi. Bilgisayarl? toraks tomografisinde sa? ?st lob ile sa? alt lob superior segmenti tutan ve mediastene invazyon g?steren kitle rapor edildi. Fiberoptik bronkoskopi incelemesinde sa? ?st lob giri?ini tamamen kapatan kitle ve ara bron?a uzan?m g?steren infiltrasyon g?r?ld?. Bronkoskopik biyopsiler tan?sal de?ildi. PET-BT incelemesinde SUDmaks de?eri 18.8 olarak ?l??ld?. Solunum fonksiyon testinde FEV1 2.52 L (%70) ve FVC 2.94 L (%66) idi. Hastaya sa? torakotomi uyguland?. Torakotomide, kitlenin vena kava s?perior ve pulmoner arteri invaze etti?i saptand?. Biyopsi ?rnekleri al?nd?. Patolojik tan? inflamatuvar ps?dot?m?r olarak rapor edildi. Kortikosteroid tedavi ba?land?. Klinik ve radyolojik yan?t al?namayan hasta radyoterapi amac? ile onkoloji klini?ine sevk edildi. Hasta Kas?m 2007 tarihinde ?ld?.
Anahtar Kelimeler: ?nflamatuvar ps?dot?m?r, akci?er, mediasten, invazyon.
SUMMARY
A case of endobronchial inflammatory pseudotumor invading the mediastinum
Ebru SULU, Ebru DAMADO?LU, Huriye BERK TAKIR, Hacer KUZU OKUR, Esra K?RO?LU, Adnan YILMAZ
1 Sureyyapasa Chest Diseases and Chest Surgery Training and Research Hospital, Istanbul, Turkey.
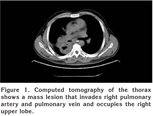
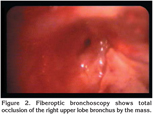
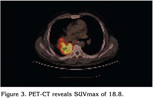
A 50-year-old-male was admitted to our hospital in March 2007, complaining of cough and hemoptysis for 3 months. Postero-anterior chest X-ray showed an opacity on right upper zone. Computed tomography of the thorax showed a mass lesion occupying the right upper lobe and superior segment of the lower lobe and invading the mediastinum. Fiberoptic bronchoscopy showed total occlusion of the right upper lobe bronchus by the mass and infiltration of the bronchus intermedius. Bronchoscopic biopsies were nondiagnostic. PET-CT revealed SUVmax of 18.8. Right thoracotomy was performed. Vena cava superior and right pulmonary artery was invaded by the mass. Biopsies were performed. Histopathologic examination demonstrated an inflammatory pseudotumor. Corticosteroid treatment was started. The tumor was clinically and radiologically unresponsive to corticosteroids. He was referred to oncology department for radiotherapy. The patient died on November 2007.
Key Words: Inflammatory pseudotumor, lung, mediastinum, invading.
Inflammatory pseudotumor is an uncommon, benign, essentially nonneoplastic, tumor-like process that usually occurs in children and young people (1). It consists of mixed components of collagen fibers, inflammatory cells, and mesenchymal cells (2). Since the initial report of this lesion by Brunn in 1939, it has also been called as plasma-cell granuloma, histiocytoma, xanthoma, xanthofibroma, xanthogranuloma, solitary mast-cell granuloma, fibrohistiocytoma, postinflammatory tumor, but the most commonly used terms include plasma-cell granuloma and inflammatory pseudotumor (3,4). It most commonly presents as a solitary pulmonary nodule, and the endobronchial presentation is uncommon (5). Although regarded as a benign lesion, it may have aggressive behavior (6). We presented a case of endobronchial inflammatory pseudotumor invading the mediastinum.
CASE REPORT
A 50-year-old male presented on march 2007 with a three-month history of cough and hemoptysis. Postero-anterior chest X-ray showed an opacity on right upper zone. His past medical history was unremarkable except smoking. Complete blood count, urinalysis and blood biochemistry were normal. Computed tomography (CT) of the thorax revealed a mass lesion that invades right pulmonary artery and pulmonary vein and occupies the right upper lobe and upper segment of the lower lobe and measures 10.5 x 9.5 x 11 cm (Figure 1). Fiberoptic bronchoscopy showed total occlusion of the right upper lobe bronchus by the mass and infiltration of the bronchus intermedius (Figure 2). Bronchoscopic biopsies were nondiagnostic. PET-CT revealed SUVmax of 18.8 (Figure 3). FEV1 was 2.52 L (70%) and FVC was 2.94 L (66%). Right thoracotomy was performed. Vena cava superior and right pulmonary artery was invaded by the mass. Biopsies were performed. Histopathologic diagnosis was an inflammatory pseudotumor. Corticosteroid treatment was started. The tumor was clinically and radiologically unresponsive to corticosteroids. He was referred to oncology department for radiotherapy. The patient died on November 2007.
DISCUSSION
Inflammatory pseudotumor is a nonneoplastic process characterized by unregulated growth of inflammatory cells. Although its exact pathogenesis is not known at present, two opinions are held: one is that it is tumorous in origin because it presents with few symptoms, has tumorous expanding growth, and has a 10% occurrence rate. The other opinion is that it is inflammatory in origin, because it presents with intraalveolar organic lesions, a past history of respiratory tract infection, and it consists of a variety of inflammatory cells (7). A history of upper respiratory tract infection or pneumonia was reported in 28% of patients (8). This tumor can be associated with trauma, paraneoplastic syndrome or other inflammatory reactions (8,9). There was not any history of trauma or infection in our patient.
Exact incidence of pulmonary inflammatory pseudotumor is not known. It is reported to be 0.04-1.2% of all pulmonary tumors (8). Inflammatory pseudotumor of the lung is not sex related. The patients vary greatly in age (1-77 years), about 60% of patients are younger than 40 years of age, and 15% are between the ages of 1 and 10 years (1,10). Melloni et al. reported that all the patients in their series were adults and only 16% were younger than 40 years (8). We presented an older male patient. He had pulmonary symptoms including cough and hemoptysis. Most patients with inflammatory pseudotumor are asymptomatic and tumor is discovered by incidental findings on chest radiographs. However, 26-56% of these patients have been reported to show clinical symptoms such as cough, hemoptysis, dyspnea and chest pain (1,7). Symptoms are strictly related to lesion location: paranchymal or endobronchial (8). The endobronchial presentation is uncommon, accounting for less than 12% of the cases, and constitutes the most symptomatic form, which frequently leads to an early diagnosis (5,10). Our patient had endobronchial presentation.
Radiologically, the tumor usually presents as a well-circumscribed, solitary, round or ovoid peripheral pulmonary nodule or mass measuring 1 to 6 cm in diameter (10). Agrons and coworkers analyzed chest X-ray features in 60 patients with pulmonary inflammatory pseudotumor (11). Fifty-two (87%) patients had solitary peripheral lesions, of which 31 were a masses and 21 were a solitary pulmonary nodule. Three (5%) patients had multiple nodules. Secondary infiltration of hilum, mediastinum, and airways is proven in 16% of patients. In a previous report, CT of the thorax revealed well-circumscribed parenchymal lesions (nodules or masses) without signs of infiltration in 15 patients, whereas 3 patients presented an infiltration of the adjacent pleura (8). Radiographics can demonstrate calcification, cavitation, notch, spicula and pleural indentation in tumor but these features are unusual (1,7). In our case, CT showed a mass lesion 11 cm in diameter. There was no calcification in the tumor. PET-CT examination identified a high standardized uptake value. Higashi et al. reported that FDG PET showed a false-positive result in a case of inflammatory pseudotumor (12). Inflammatory pseudotumors are difficult to diagnose. Preoperative diagnostic methods such as percutaneous fine needle biopsy and bronchoscopy is considered insufficient for diagnosis. The diagnosis is made by surgical procedures such as video-assisted thoracoscopic surgery or open lung biopsy (1,7,8). In our patient, bronchoscopic biopsies were nondiagnostic, we established the diagnosis of inflammatory pseudotumor with open lung biopsy.
Although pulmonary inflammatory pseudotumors are regarded as a benign lesion, they may have aggressive features, and they may encase bronchi or invade chest wall, mediastinal structures, the spine and vessels. Multiple recurrences and metastatic spread can also be seen (6,10,11,13). Corneli et al. reported that the tumor invaded the mediastinal pleura, the pericardium, the esophagus, the thoracic aorta and the diaphragm (6). The treatment of choice of these tumors is surgery. Wedge resection, if radical, is suitable for curative purposes. When wedge resection is not feasible, the lesion is removed with major resections such as lobectomy or pneumonectomy. Nonsurgical treatment modalities including radiotherapy, chemotherapy, and steroids may have a place in the setting of incomplete surgical resection, multifocal disease, tumor recurrence, or contraindication to lung resection (6,8,10,14). The prognosis of patients with completely resected inflammatory pseudotumors is excellent: 78% to 100% of patients were in complete remission after an average follow-up of 3.3 years after surgical resection. Intrathoracic recurrence was seen in 5% of cases (10). The tumor may be fatal. Bahadori and Liebow reported the fatal outcome of a patient with involvement of esophagus and superior vena cava (15). In our case, the tumor invaded the mediastinum. Because the patient was inoperable, he was treated with corticosteroids followed by radiotherapy. The tumor was aggressive and our patient died 8 months after diagnosis.
In conclusion, pulmonary inflammatory pseudotumor is rare. The preoperative diagnosis of this tumor is difficult. Although it is considered as benign, it may have aggressive behavior and poor prognosis.
CONFLICT of INTEREST
None declared.
REFERENCES
- Alexiou C, Obuszko Z, Beggs D, Morgan WE. Inflammatory pseudotumors of the lung. Ann Thorac Surg 1998; 66: 948-50. [?zet] [Tam Metin] [PDF]
- Zennaro H, Laurent F, Vergier B, et al. Inflammatory myofibroblastic tumor of the lung (inflammatory pseudotumor): uncommon cause of solitary pulmonary nodule. Eur Radiol 1999; 9: 1205-7. [?zet]
- Park SH, Choe GY, Kim CW, et al. Inflammatory pseudotumor of the lung in a child with mycoplasma pneumonia. J Korean Med Sci 1990; 5: 213-23. [?zet] [PDF]
- Tun??zg?r B, ?st?nsoy H, Bak?r K, et al. Inflammatory pseudotumor of the lung. Thorac Cardiovasc Surg 2000; 48: 112-3. [?zet]
- Sanchez PG, Madke GR, Pilla ES, et al. Endobronchial inflammatory pseudotumor: a case report. J Bras Pneumol 2007; 33: 484-6. [?zet]
- Corneli G, Alifano M, Parri SF, et al. Invasive inflammatory pseudotumor involving the lung and the mediastinum. Thorac Cardiovasc Surg 2001; 49: 124-6. [?zet]
- Kobashi Y, Fukuda M, Nakata M, et al. Inflammatory pseudotumor of the lung: clinicopathological analysis in seven adult patients. Int J Clin Oncol 2006; 11: 461-6. [?zet]
- Melloni G, Carretta A, Ciriaco P, et al. Inflammatory pseudotumor of the lung in adults. Ann Thorac Surg 2005; 79: 426-32. [?zet] [Tam Metin] [PDF]
- Hosler GA, Steinberg DM, Sheth S, et al. Inflammatory pseudotumor: a diagnostic dilemma in cytopathology. Diagn Cytopathol 2004; 31: 267-70. [?zet]
- Kim TS, Han J, Kim GY, et al. Pulmonary inflammatory pseudotumor (inflammatory myofibroblastic tumor): CT features with pathologic correlation. J Comput Assist Tomogr 2005; 29: 633-9. [?zet]
- Agrons GA, de Christerson R, Kirejczyk WM, et al. Pulmonary inflammatory pseudotumor: radiologic features. Radiology 1998; 206: 511-8. [?zet]
- Higashi K, Ueda Y, Sakuma T, et al. Comparison of [(18)F]FDG PET and (201)Tl SPECT in evaluation of pulmonary nodules. J Nucl Med 2001; 42: 1489-96. [?zet] [Tam Metin] [PDF]
- Akman C, Dincbas FO, Oz B, et al. Unusual cause of dysphagia: inflammatory pseudotumor of the lung. Southern Med J 2005; 98: 665-8. [?zet]
- Cerfolio RJ, Allen MS, Nascimento AG, et al. Inflammatory pseudotumors of the lung. Ann Thorac Surg 1999; 67: 933-6. [?zet] [Tam Metin] [PDF]
- Bahadori M, Liebow A. Plasma cell granulomas of the lung. Cancer 1973; 31: 191-208.
Yaz??ma Adresi (Address for Correspondence):
Dr. Ebru SULU,
Feyzullah Mahallesi Lale Oralo?lu Sokak
?akar Apartman? No: 5 Daire: 4
Maltepe 34843 ?STANBUL - TURKEY
e-mail: ebrusulu@hotmail.com