Bir ya? alt? bebeklerde akci?er t?berk?lozu: Erken tan?n?n ?nemi
G?ls?m ?clal BAYHAN1, Ay?e Se?il EK??O?LU2, Bur?ak K?T?? ?EL?K1, G?n?l TANIR3
1 Dr. Sami Ulus Kad?n Do?um, ?ocuk Sa?l??? ve Hastal?klar? E?itim ve Ara?t?rma Hastanesi, ?ocuk Sa?l??? ve
Hastal?klar? Klini?i, Ankara,
2 Dr. Sami Ulus Kad?n Do?um, ?ocuk Sa?l??? ve Hastal?klar? E?itim ve Ara?t?rma Hastanesi, Radyoloji Bilim Dal?,
Ankara
3 Dr. Sami Ulus Kad?n Do?um, ?ocuk Sa?l??? Ve Hastal?klar? E?itim ve Ara?t?rma Hastanesi, ?ocuk ?nfeksiyon
Hastal?klar? Bilim Dal?, Ankara
?ZET
Bir ya? alt? bebeklerde akci?er t?berk?lozu: Erken tan?n?n ?nemi
T?berk?loz b?y?k ?ocuklarda iyi tan?mlanmakla birlikte infantil t?berk?loz ?ok iyi bilinmemektedir. Literat?rde infantil t?berk?loz ile ilgili ?ok az makale bulunmaktad?r. Bu ?al??mada ?ubat 2007-May?s 2009 tarihleri aras?ndaki infantil t?berk?loz olgular? retrospektif olarak incelendi. Pulmoner t?berk?lozlu 13 olgu saptand?. Hastalar?n en s?k semptomlar? ?ks?r?k (%72.4), gece terlemesi (%35.7) ve ate?ti (%21.4). D?rt hastada hi?bir semptom yoktu. On ?? hastan?n 12'sinin fizik muayenesi normaldi. T?m hastalar?n -akci?er grafisi normal olanlar?n da- toraks bilgisayarl? tomografilerinde patoloji saptand?. Hastalar?n t?m? antit?berk?loz tedaviyi iyi tolere etti ve tedavi ile d?zeldi. ?nfantil t?berk?lozun ?nlenmesi esas olarak aile i?i t?berk?lozlu olgular?n erken tespiti ve tedavisine dayan?r. Bu ?al??ma y?ksek ??phe, akci?er grafisi ve bilgisayarl? tomografinin do?ru kullan?m?yla infantil t?berk?lozun erken tan?s?n?n m?mk?n oldu?unu g?stermi?tir. Erken tan? ve tedavi hastal???n disseminasyonunu azaltabilir ve mortaliteyi d???rebilir; bu nedenle pediatristler infantil t?berk?loz konusunda uyan?k olmal?d?r.
Anahtar Kelimeler: ?nfantil t?berk?loz, erken tan?, t?berk?loz komplikasyonlar?.
SUMMARY
Pulmonary tuberculosis in infants less than one year old: implications for early diagnosis
G?ls?m ?clal BAYHAN1, Ay?e Se?il EK??O?LU2, Bur?ak K?T?? ?EL?K1, G?n?l TANIR3
1 Department of Children Health and Diseases, Dr. Sami Ulus Obstetrics, Children Health and Diseases,
Training and Research Hospital, Ankara, Turkey,
2 Department of Radiology, Dr. Sami Ulus Obstetrics, Children Health and Diseases, Training and Research
Hospital, Ankara, Turkey,
3 Department of Children Infectious Diseases, Dr. Sami Ulus Obstetrics, Children Health and Diseases,
Training and Research Hospital, Ankara, Turkey.
Tuberculosis in older children has been well described; however, its description in infants is very limited. There are a few studies of infants with tuberculosis in the literature. In this study from February 2007 to May 2009, cases of infantile tuberculosis investigated retrospectively. Thirteen patients with pulmonary tuberculosis detected. Mean age of the patients was 168.8 days. The most frequent symptoms were cough in 10 (72.4%) patients, night sweating in five (35.7%) and fever in three (21.4%). Four patients didn't have any symptoms. Physical examinations were normal in 12 patients. Thorax computerized tomography studies of all of the patients were abnormal included the cases with normal chest radiographies. Antituberculosis treatment was well tolerated by all of the patients and all of them improved. Prevention of tuberculosis in infants rest upon the early detection and treatment of tuberculosis of the infant's household members. This study demonstrates that with high index of suspicion and the correct use of chest radiographs and thorax computerized tomography, the disease diagnosed early in infants. Early diagnosis and treatment may prevent dissemination and may reduce mortality, so pediatrician should alert for tuberculosis in infants.
Key Words: Tuberculosis of infants, early diagnosis, complication of tuberculosis.
World Health Organization (WHO) estimates that 8 to 10 million people develop tuberculosis (TB) in the World every year. It is estimated that one-third of the World's population (2 billion people) is infected with the tubercle bacillus. Children less than 15 years of age constitute approximately 15% of the total TB case load in many developing communities. Approximately 1.3 million cases of TB disease and 400.000 tuberculous-related deaths occur annually among children younger than 15 years old (1,2). Incidence of TB was 30 per 100.000 population per year, prevalence of tuberculosis was 34 per 100.000 population in Turkey according to WHO records 2007 (3). Generally adult pulmonary TB cases are source of infection for children therefore childhood TB reflects continuing transmission in a community (4).
Morbidity and mortality of childhood TB is highest in infancy. The frequent occurrence of disseminated forms of tuberculosis such as miliary tuberculosis and tuberculous meningitis are partly responsible for poor prognosis (2,5,6,7,8). We evaluated retrospectively clinical and radiological features of 13 infants who were treated with anti-tuberculosis drugs with good outcome. The purpose of this study are to investigate the role of chest computerized tomography (CT) scan in the early diagnosis of infantil TB.
MATERIALS and METHODS
The Sami Ulus Obstetrics, Children's Health and Diseases Training and Research Center in Ankara is one of the largest children's hospital in Turkey. It is a tertiary-care teaching hospital with 400 beds and acts as a referral pediatric center for the entire country. From February 2007 to May 2009, 13 children who are under one year old were diagnosed as pulmonary TB.
The demographic characteristics, contact history with TB patient, medical status of adult index case, symptoms and physical examination findings of the patients were recorded on the standard forms. Screening of household contacts of patients was made by contact with tuberculosis dispensaries. Tuberculin skin test (TST) was done by putting 0.1 mL 5 TU purified protein derivate (PPD) solution under the top layer of skin on inner forearm. Test was checked at 72th hour by measure horizontal and vertical diameter by pen-point technique. TST 10 mm was evaluated as positive in patients who had not Bacille Calmette Guerin (BCG) vaccine, and TST 15 mm was evaluated as positive in patients who had BCG vaccine according to the Turkish Ministy of Health. Reference Book for Tuberculosis Control. The laboratory tests included erythrocyte sedimentation rate (ESR), TST and cerebrospinal fluid (CSF) examination findings. Chest radiography (CXR) was taken on the first application of the patients. All cases who had either suspicious findings on chest radiography or normal findings were undergone thoracal CT investigation. Two months after the end of the anti-tuberculosis treatment control chest radiography or thorax CT was taken if required. Digital chest roentgenograms were performed by using Definium 6000 PM, GE Medical Systems (95 kVp, 290 mAs). Helical CT examinations were performed by using Hitachi Radix Turbo on prone position (7-mm thickness, a 1 pitch, 120 kVp, 75 mAs). Intravenous contrast material lopromide was administered through to antecubital vein at a dose of 1.5 cc/kg. Early morning gastric aspirate samples collected from the patients on consecutive two days. 20 mL 0.9% isotonic saline with sodium carbonate injected to stomach by using a nasogastric tube and after 2-3 minutes gastric aspirate specimens were taken. Microbiologic examinations were made by Refik Saydam Hygiene Center Tuberculosis Reference Laboratory. Acid-fast bacilli (AFB) were detected by Ziehl-Nielsen stain. Samples were inoculated into Lowenstein?Jensen agar contain egg- potatoes using Modified Petrof technique according to the Guideline of Turkish Ministry of Health Tuberculosis Department.
Patients were treated with isoniazid, rifampin, pyrazinamide. Isoniazid was administered PO for 6 months at a dosage of 10 mg/kg per day. Rifampin was administered PO for 6 months at a dosage of 15 mg/kg per day. Pyrazinamide was administered p.o. for first 2 months at a dosage of 35 mg/kg per day. Patients had been treated in hospital at the beginning of treatment, and then they followed as outpatients.
The diagnosis of tuberculosis was established by a positive culture of gastric aspirates for M. tuberculosis or presence of more than two of the following three criteria: TST positivity; discovery of at least one family member with tuberculosis and finding that subsequent clinical or radiologic improvement from anti-TB treatment (9).
RESULTS
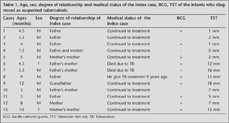
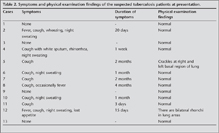
The patient age ranged from 1.5-12 months, days, mean age 5.6 months. The male to female ratio was 11/2. The sources of infection were identified in 12 of the 13 patients. The father of the eighth case had been given anti-TB treatment 9 years ago. The paternal grandmother of the sixth and seventh patients who are cousins had died some weeks before presentation of these patients. The cases are listed with the categories of age, sex, degree of relationship of the adult index cases with patients, medical status of index cases, BCG, TST in Table 1. The median duration of symptoms was 30 days that ranged between 1 week to 4 months. The most frequent symptoms were cough in 10 (72.4%) patients, night sweating in 5 (35.7%) and fever in 3 (21.4%). Four patients didn't have any symptoms. Physical examinations were normal in 11 patients. Symptoms of the patients at presentation and physical examination findings are given in Table 2.
Microbiological studies were performed in only five patients for practical reasons. AFB were negative in all of the five patients (cases 2,6,7,8,10). In culture, only in one of them five colonies of M. tuberculosis were yielded (case 6). The mean value of ESR 29 (29.8) mm/hour. CSF examination findings were normal in all of the patients. The diagnosis of tuberculosis was established by positive culture of gastric aspirates for M. tuberculosis in one patient in the remaining 12 patients, more than two of the following three criteria were met: TST positivity (three cases); discovery of at least one family member with tuberculosis (12 cases) and finding that subsequent clinical or radiologic improvement from anti-TB treatment (11 cases) (9).
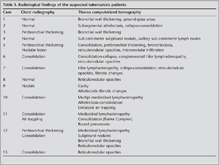
Thorax CT studies of all of the patients were abnormal included the cases with normal chest radiographies. Multiple radiographic findings were detected in patients by thorax CT. Radiological findings of the patients were given in Table 3. Treatment was completed at the end of 6 months in 10 children. One patient's treatment is at the second months. Two patients lost of follow-up. Treatment-related adverse effects didn't detect in any patients. Antituberculosis treatment was well tolerated by all patients. The mean follow-up duration after treatment had been completed was 115.6 (193.7) days. No infant had a relapse or recurrence of disease. TB related complication and death didn't occur. Follow-up CXR or CT performed after 2 months anti-TB medication completed. Control thorax CT performed in the patients who had normal or inconclusive CXR initially. Excellent clinical and radiological response to treatment was demonstrated in all of our patients with no progression.
DISCUSSION
Diagnosis of childhood TB is difficult. The sputum smears are positive in only 10%-15% and culture positivity is detected in only 30%-40% of the children (7,10,11,12). Gastric aspirate culture yielded M. tuberculosis from one of our five patients who could be tested. In the absence of positive cultures, TB diagnosis mainly based on clinical evaluation, laboratory and/or radiological evidence of TB disease and history of exposure to tuberculosis, and exclusion of other disease (13).
In our study all of the patients had history of contact with adult cases and TB investigated in these infants for this reason. TB control programs in developing countries aim mainly to detect and treat adults with sputum smear-positive tuberculosis, because they are the most infectious patients. Investigations of contacts and treatment of contacts with latent TB infection is a strategy in the control and elimination of TB in developed countries. In a study of 596 culture-confirmed childhoods TB from South Africa, a history of contact with an infectious pulmonary TB case was recorded in 295 (49.5%) children. The source case was a parent in 121 (41.0%), an uncle/aunt in 68 (23.1%), a grandparent in 26 (8.8%), an older sibling in 15 (5.1%), other household cases in 27 (9.2%), a neighbor in 19 (6.4%) and another or unknown case in 28 (9.5%). Twenty three children (7.8%) had more than one source case (4). We think that adult index case is an important clue for the diagnosis of infant tuberculosis.
It has been reported that TST might be positive up to two-thirds of HIV-uninfected children with TB in developing countries (14). In our study 30% of the infants with TB had a negative TST results. TST is an evidence of TB infection but a positive tuberculin reaction by itself does not indicate the presence or extent of TB disease (13,14).
The most frequent signs in children with TB are
1. A persistent non-remitting cough (> 2-3 weeks) not improving after a course of antibiotics,
2. Fever of unknown origin,
3. Wight loss or failure to gain weight (13). Cough, night sweating and fever were the most frequent symptoms in our patients. Interestingly four of our patients didn't have any symptoms or physical signs. TST positivity and history of contact were reasons for their medical evaluation and lead the diagnosis in these four cases.
The presence of lymphadenopathy on CXR is frequently used for diagnosing pulmonary TB in children. However, the low accuracy of CXR in assessing lymphadenopathy has been reported previously (15). Major problem is the quality of CXRs, e.g. poor inspiratory or rotated film might give an impression of a "widened mediastinum". It has been believed that caution should be exercised in using the presence of lymphadenopathy on CXR to diagnose tuberculosis in children (14,15). CT findings of pulmonary TB in children and to define indications for the use of CT were studied previously in infants and children. Mediastinal or hilar lymphadenopathy revealed as low-attenuation nodes with rim enhancement or calcification was reported as the most characteristic CT finding of pulmonary TB in children (16). It is well established that CT scans have advantages over CXR for detecting TB lymphadenopathy, the bronchogenic spread of TB and airway complications (2,16,17,18). In a 12-year study of 25 infants with TB whose age were between 2 to 12 months (mean age, 5.9 months), radiographic findings had been reviewed retrospectively. CXR were performed initially in all patients. In this study thorax CT scans were performed 1-10 days (mean 4 days) after initial CXR for one or more of the following reasons: to evaluate unusual findings on radiographs such as mass like lesions or widespread nodules; to find or confirm lymphadenopathy; and to detect or evaluate complications. Authors reported that, CXR showed mediastinal lymphadenopathy and parenchymal abnormality in 72% and 96% of patients, respectively, and the most frequent radiographic finding of pulmonary parenchymal lesions was consolidation. In four patients (24%) in this series, the diagnosis of tuberculosis was suggested only after a CT scan revealed enlarged lymph nodes with central necrosis (18). In our cases of 1, 3 and 13 had not apparent disease or abnormal chest X-ray (case 1), but they had a positive TST (case 13) or history of close contact, CT revealed peribronchial thickening, ground-glass areas and reticulonodular opacities suggesting TB disease. In a study that investigated CT findings in 41 children with confirmed TB, foci of nodular densities from 1 mm to 2 cm, were seen in 12 patients (29%) and bronchial wall thickening was seen in nine patients. Authors mentioned that although a similar appearance can be seen in patients with atypical mycobacterial or bacterial bnonchopneumonia, these CT findings, if present, can be helpful in diagnosing tuberculosis in children (18). Centrilobular nodules of ground-glass attenuation was reported among the CT findings with TB (9,19). Tuberculosis during early childhood, in particular, there is a continuum between tuberculosis infection and disease. When establishing the diagnosis in a child with suspected tuberculosis, the distinction between infection and disease frequently depends on the interpretation of the imaging studies. In our study, CT scan detected pathologic findings in four patients whose CXR completely normal. We detected also additional findings that we could not determine on CXR included subpleural nodules, mediastinal lymph nodes, bronchiectasia, parenchimal cavity, reticulonodular opacities, air trapping areas, round pneumonia, micronodular infiltration, athelectasia and concomitant collapse to consolidation. We think that, CT scans can be helpful in diagnosing tuberculosis when findings of CXR normal or inconclusive.
Overall the risk of TB diseases was highest in infants and in adolescents, with the lowest in children aged between 5 and 10 years. Risk of development of pulmonary TB following primary infection 30-40% in infants under one year of age, 10-20% in infants 1-2 years of age. Dissemination of TB (miliary TB or central nervous system TB) 10-20% in infants under 1 years of age, 2.5% in infants 1-2 years of age (2,5,6,7,8,10). The children who are 3 years of age and immune competent were described as low-risk children. After primary M. tuberculosis infection disease progression is rare in these children and is associated with the presence of persistent nonremitting symptoms. However the children who are 3 years of age and/or immune compromised progression of infection to disease and disease progression is more frequent and may disseminate more rapidly (11).
Treatment response will often be judged on clinical criteria such as symptom resolution, weight gain or improvement or regression of radiological findings (20).
Exposure to an adult index case, a positive TST and the presence of suggestive signs on chest radiograph are the classic triad of childhood TB. The prevalence of TB disease among household contacts of smear-positive TB cases is high. WHO advices active tracing and screening of children younger than 5 years old in household contact with a sputum smear-positive tuberculosis index case (21). The actively detected cases with contact investigation may have milder disease at early stage.
Guidelines for screening include tuberculin skin testing and CXR for purposes of either preventive chemotherapy or early diagnosis of childhood tuberculosis (22). In current study included infants that have only a contact history. Although some of them had positive TST, they had normal CXR. These cases could be misdiagnosed as latent TB infection in the absence of CT imaging. We concluded that, because of the higher dissemination risk in infants who exposed to an adult index, advanced imaging such as thorax CT can be applied but should be restricted to in this setting. CT scan can be a useful diagnostic technique for infant TB, as it can show parenchymal lesions, tuberculous lymphadenopathy better than CXR and can be abnormal while CXR is normal.
CONFLICT of INTEREST
None declared.
REFERENCES
- Jacobs RF, Starke JR. In: Long SS, Pickering LP, Prober CG (eds). Principles and Practice of Pediatric Infectious Diseases. Pennsylvania: Churchill Livingstone, 2003:? 791-810.
- Lighter J, Rigaud M. Diagnosing childhood tuberculosis: traditional and innovative modalities. Curr Probl Pediatr Adolesc Health Care 2009; 39: 61-88.
- Country Profil. Turkey. Surveillance and epidemiology. http://apps.who.int/globalatlas/predefinedReports/TB/PDF_Files/tur.pdf. Accessed September 18, 2009.
- Schaaf HS, Marais BJ, Whitelaw A, et al. Culture-confirmed childhood tuberculosis in Cape Town, South Africa: a review of 596 cases. BMC Infect Dis 2007; 7: 140. [?zet] [Tam Metin] [PDF]
- Cruz AT, Starke JR, Clinical manifestation of tuberculosis in children. Paediatr Rev 2007; 8: 107-17. [?zet]
- Maltezou HC, Spyridis P, Kafetsiz DA. Tuberculosis during infancy. Int J Tuberc Lung Dis 2000; 4: 414-9. [?zet]
- Newton SM, Brent AJ, Anderson S, et al. Paediatric tuberculosis. Lancet Infect Dis 2008; 8: 498-510. [?zet] [Tam Metin] [PDF]
- Schaaf HS, Gie RP, Beyers N, et al. Tuberculosis in infants less than 3 months of age. Arch Dis Child 1993; 69: 371-4. [?zet] [PDF]
- Ors F, Deniz O, Bozlar U, et al. High-resolution CT findings in patients with pulmonary tuberculosis: correlation with the degree of smear positivity. J Thorac Imaging 2007; 22: 154-9. [?zet]
- Marais BJ. Tuberculosis in children. Pediatr Pulmonol 2008; 43: 322-9. [?zet]
- Marais BJ, Gie RP, Hesseling AC, et al. A refined symptom-based approach to diagnose pulmonary tuberculosis in children. Pediatrics 2006; 118: 1350-9. [?zet] [Tam Metin] [PDF]
- Marais BJ, Pai M. New approaches and emerging technologies in the diagnosis of childhood tuberculosis. Paediatr Respir Rev 2007; 8: 124-33. [?zet]
- Rigouts L. Clinical practice: diagnosis of childhood tuberculosis. Eur J Pediatr 2009; 168: 1285-90. [?zet]
- Coulter JB. Diagnosis of pulmonary tuberculosis in young children. Ann Trop Paediatr 2008; 28: 3-12. [?zet]
- Swingler GH, du Toit G, Andronikou S, et al. Diagnostic accuracy of chest radiography in detecting mediastinal lymphadenopathy in suspected pulmonary tuberculosis. Arch Dis Child 2005; 90: 1153-6. [?zet] [PDF]
- Kim WS, Moon WK, Kim IO, et al. Pulmonary tuberculosis in children: evaluation with CT. AJR Am J Roentgenol 1997; 168: 1005-9. [?zet] [PDF]
- Bosch-Marcet J, Serres-Cr?ixams X, Zuasnabar-Cotro A, et al. Comparison of ultrasound with plain radiography and CT for the detection of mediastinal lymphadenopathy in children with tuberculosis. Pediatr Radiol 2004; 34: 895-900. [?zet]
- Kim WS, Choi JI, Cheon JE, et al. Pulmonary tuberculosis in infants: radiographic and CT findings. AJR Am J Roentgenol 2006; 187: 1024-33. [?zet] [Tam Metin] [PDF]
- Okada F, Ando Y, Yoshitake S, et al. Clinical/pathologic correlations in 553 patients with primary centrilobular findings on high-resolution CT scan of the thorax. Chest 2007; 132: 1939-48. [?zet] [Tam Metin] [PDF]
- Donald PR, Schaaf HS. Old and new drugs for the treatment of tuberculosis in children. Paediatr Respir Rev 2007; 8: 134-41. [?zet]
- World Health Organization: Guidance for national tuberculosis programmes on the management of tuberculosis in children. WHO, Geneva, WHO/HTM/TB/2006 371.
- Marais BJ, Gie RP, Hesseling AC, et al. Radiographic signs and symptoms in children treated for tuberculosis: possible implications for symptom-based screening in resource-limited settings. Pediatr Infect Dis J 2006; 25: 237-40. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. G?ls?m ?clal BAYHAN,
Mahmur Esat Bozkurt Caddesi
Dedeefendi Sokak No: 12/3 Kolej