Plevral
ef?zyonlar?n ay?r?c? tan?s?nda serum ve plevral s?v? N-Terminal-Pro-B-Tip
natri?retik peptid konsantrasyonunun yeri
Arzu
YORGANCIO?LU1, Aylin ?ZGEN ALPAYDIN1, Nesrin YAMAN2,
Fatma TANEL?3, ?zg?r BAYTURAN4,
Ay??n ?AKAR CO?KUN1, P?nar ?EL?K1
1 Celal Bayar ?niversitesi T?p Fak?ltesi, G???s Hastal?klar? Anabilim Dal?, Manisa,
2 SB G???s Hastal?klar? Hastanesi, Bal?kesir,
3 Celal Bayar ?niversitesi T?p Fak?ltesi, Biyokimya Anabilim Dal?, Manisa,
4 Celal Bayar ?niversitesi T?p Fak?ltesi, Kardiyoloji Anabilim Dal?, Manisa.
?ZET
Plevral ef?zyonlar?n ay?r?c? tan?s?nda serum ve plevral s?v? N-Terminal-Pro-B-Tip natri?retik peptid konsantrasyonunun yeri
Son y?llarda, plevral ef?zyonlar?n ay?r?c? tan?s?nda N-Terminal-Pro-B-Tip natri?retik peptid (NT-proBNP) gibi yeni belirte?lerin kullan?m? g?ndemdedir. ?al??mam?zda, NT-proBNP'nin ?zellikle kardiyak kaynakl? plevral ef?zyonlarda tan?sal de?erini ara?t?rmay? ama?lad?k. Plevral ef?zyonu olan 45 hasta ?al??maya dahil edildi. Hastalar?n serum ve plevral ef?zyonlar?nda NT-proBNP d?zeyleri ve Light kriterlerinde yer alan biyokimyasal belirte?ler analiz edildi. Klinik de?erlendirmeye g?re, gereken durumlarda plevral s?v?n?n k?lt?r?, ARB direkt muayenesi ve sitolojik tetkiki yap?ld?. Kardiyak patoloji d???n?len hastalarda, kardiyolojik de?erlendirme ve ekokardiyografi de yap?ld?. Light kriterlerine g?re plevral ef?zyonlar?n 38'i eks?da, yedisi trans?dayd?. Hastalar?n 13'?nde son tan? malign ef?zyon, 10'unda infeksiyon (t?berk?loz/pn?moni), 21'inde konjestif kalp yetmezli?i, birinde ise plevral ef?zyonla ilgili di?er hastal?kt?. Konjestif kalp yetmezli?i ile ili?kili plevral s?v?larda, medyan (25-75. ?eyrekler) NT-proBNP d?zeyleri serumda 4747 pg/mL (931-15754), plevral s?v?da ise 4827 pg/mL (1290-12430) idi. Kardiyak olmayan nedenlere ba?l? plevral s?v?larda ise bu d?zeyler serumda 183 pg/mL (138-444), plevral s?v?da 245 pg/mL (187-556) olarak saptand?. Konjestif kalp yetmezli?i olan hastalarda serum ve plevral s?v? NT-proBNP d?zeyleri anlaml? olarak y?ksekti (her ikisi i?in p< 0.001). Son tan?lar?na g?re d?rt grup kar??la?t?r?ld???nda serum ve plevral s?v? NT-proBNP d?zeyleri en y?ksek konjestif kalp yetmezli?inde g?zlendi, bunu malignite, infeksiyon ve di?erleri izlemekteydi (her ikisi i?in p< 0.001). Kardiyolojik de?erlendirme ile konjestif kalp yetmezli?i kabul edilen 21 hastan?n 14'?nde Light kriterlerine g?re eks?da mevcuttu. Trans?dalarda serum ve plevral s?v? NT-proBNP d?zeyleri istatistiksel anlaml? olarak y?ksekti (p= 0.009). Plevral s?v? NT-proBNP d?zeylerinin ?l??m? iyi bir yakla??md?r ve plevral s?v? NT-proBNP d?zeyleri kardiyak kaynakl? s?v?lar? Light kriterleri ve serum NT-proBNP d?zeylerine g?re daha iyi yans?t?r.
Anahtar Kelimeler: Plevral ef?zyon, BNP, NT-proBNP, kalp yetmezli?i.
SUMMARY
Serum and pleural fluid N-Terminal-Pro-B-Type natriuretic peptide concentrations in the differential diagnosis of pleural effusions
Arzu YORGANCIO?LU1, Aylin ?ZGEN ALPAYDIN1, Nesrin YAMAN2, Fatma TANEL?3, ?zg?r BAYTURAN4, Ay??n ?AKAR CO?KUN1, P?nar ?EL?K1
1 Department of Chest Diseases, Faculty of Medicine, Celal Bayar University, Manisa, Turkey,
2 Chest Diseases Hospital, Balikesir, Turkey,
3 Department of Biochemistry, Faculty of Medicine, Celal Bayar University, Manisa, Turkey,
4 Department of Cardiology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey.
Currently, new biomarkers like N-Terminal-Pro-B-Type natriuretic peptide (NT-proBNP) have been used in the differential diagnosis of pleural effusions. In our study, we aimed to investigate the diagnostic value of NT-proBNP, especially in cardiac originated pleural effusions. Forty-five patients with pleural effusions were included in the study. NT-proBNP levels and biochemical markers involved in the Light's criteria were analyzed in pleural fluid and serums of the patients. Pleural fluid culture, AFB smear, cytology were performed where they were indicated according to the clinical evaluation. In patients, to whom cardiac pathology was considered to be; cardiological evaluation and echocardiography were also done. Thirty-eight pleural effusions were exudative and, 7 were transudative according to the Light's criteria. Final diagnosis were malignant effusion in 13, infection (tuberculosis/pneumonia) in 10, congestive heart failure in 21, and other conditions related with pleural effusion in 1 of the patients. Median (25th to 75th percentiles) NT-proBNP levels of serum and pleural fluid due to congestive heart failure (CHF) were 4747 pg/mL (931-15754) and 4827 pg/mL (1290-12.430) while median NT-proBNP levels of serum and pleural fluid related with non-cardiac reasons were 183 pg/mL (138-444) and 245 pg/mL (187-556) respectively. NT-proBNP levels of serum and pleural fluid were significantly high in CHF (p< 0.001 for both). When four groups were compared serum and pleural fluid NT-proBNP levels were highest in the CHF group which was followed by malignancy, infection and others (p< 0.001 for both). Fourteen of 21 patients who were accepted to have congestive heart failure as the final diagnosis by a cardiological evaluation had an exudative pleural fluid according to the Light's criteria. Serum and pleural fluid NT-proBNP levels were higher in transudates and this reached statistically significance for pleural fluid (p= 0.009). We suggest that measurement of pleural fluid NT-proBNP is a smart approach and pleural fluid NT-proBNP can reflect cardiac origin of effusions better than serum NT-proBNP and Light's criteria
Key Words: Pleural effusion, BNP, NT-proBNP, heart failure.
Determining the etiology of a pleural effusion is a diagnostic dilemma. The first step is; to perform pleurocentesis and pleural fluid analysis to establish the fluid nature; whether it is a transudate or an exudate. This discrimination is generally made by the criteria defined by Light which include; pleural fluid/serum protein ratio (cut-off, 0.5); pleural fluid lactate dehydrogenase (LDH) concentration more than two-thirds the upper normal reference serum value; and pleural fluid/serum LDH ratio (cut-off, 0.6). When any of these criteria are met, pleural fluid is considered to be an exudate (1,2). In a meta-analysis of 8 studies with 1448 patients, several other biochemical markers like pleural fluid cholesterol, albumin gradient, and serum/pleural fluid bilirubin ratio have been compared with Light's criteria and Light's criteria have been determined to possess the best discriminative properties (3). However, Light's criteria have been developed as a high sensitive tool for detecting exudative effusions and generally the underlying pathology is not discriminated. Up to 15% to 25% of transudates are misdiagnosed as exudates according to Light's criteria (4,5). Some studies have demonstrated that a considerable proportion of patients with pleural effusions due to heart failure especially after administration of diuretics were classified as exudates (6,7). Therefore a diagnostic approach for identifying pleural effusions related with heart failure need to be established.
Natriuretic peptide family plays an important role in major homeostatic mechanisms related with volume, osmosis and blood pressure regulation. Although, all natriuretic peptide family has vasodilator and venodilator effects and induces diuresis and natriuresis the degree of these features change from one peptide to another (8). B-type natriuretic peptide (BNP), a member of the natriuretic peptide family is a vasoactive cardiac neurohormone and is mainly excreted from ventricular myocytes by the stimulus of wall tension (9). Both inactive amino terminal fragment of the BNP prohormone (NT-proBNP) and biologically active BNP arises from pro-BNP which is the precursor molecule (10). NT-proBNP is a sensitive marker of cardiac dysfunction and increased levels of NT-proBNP have been shown to be useful in the diagnosis of congestive heart failure (CHF) (11,12). It has been recommended as a serum marker for the diagnosis of CHF including systolic and diastolic ventricular dysfunction and valvular diseases in American College of Cardiology/American Heart Association (ACC/AHA) guidelines (13,14). Recently, the diagnostic value of the NT-proBNP concentrations in pleural fluid has been evaluated and increased levels of NT-proBNP in the pleural fluid have been shown to be valuable in the discriminative diagnosis of pleural effusions related with cardiac disorders (15,16).
The aim of the present study was to investigate the usefulness of measuring NT-proBNP levels in serum and pleural fluid for the diagnosis of pleural effusions resulting from CHF.
MATERIALS and METHODS
This prospective study was performed between May 2007 and July 2008 in our pulmonary diseases clinic. Pleural fluid and serum samples of the patients presenting with pleural effusions were collected. Forty-five patients were consecutively selected according to the presence of diagnostic thoracentesis indication. Local ethics committee approval was obtained and each patient signed written informed consent before thoracentesis.
Inclusion criteria were; radiologically determined pleural effusion volume that could be drained by thoracentesis (> 10 mm in lateral decubitis graphy) and the necessity of diagnostic thoracenthesis. Exclusion criteria were; coagulopathy, thorax deformity interfering with thoracentesis and incorporation of the patients.
Demographic characteristics of the patients were recorded. Blood and pleural fluid specimens were collected to the standard vacuumed tubes simultaneously and centrifuged 15 minutes at 3500 rpm. Specimens were put into 2 mL tubes and stored at -80?C to be analysed later for NT-proBNP. Serum and pleural fluid LDH, total protein and albumin analysis were carried out on the same day within 4 hours after specimen collection. Analyses of these biochemicals were performed by enzymatic and timed end point methods with their original reactivates by Beckman Coulter Unicel DxC 800 Synchron Clinical System (Beckman Coulter Inc., Fullerton, CA, USA) analyzer. Pleura and pleural fluid NT-proBNP levels were measured altogether with the chemolusency method by original reactives Roche Elecsys 1010 Immunoassay System (Roche Diagnostics GmbH, Mannheim, Germany), on the same day after the specimen collection was ended. The performance characteristics of the reagents were performed and according to the manufacturer the test had an intra-assay coefficient variations of 4.2% at 44 pg/mL, 2.4% at 126 pg/mL, 1.3% at 2410 pg/mL concentrations. Inter-assay coefficient variations of the test were 4.6% at 44 pg/mL, 2.6% at 126 pg/mL, 1.8% at 2410 pg/mL concentrations.
Upon clinical judgment, pleural fluid specimens underwent to bacterial and fungal culture, acid-fast bacilli (AFB) smear and culture whereas cytological examinations were performed to all the specimens independently from the clinical presentation.
The diagnosis of congestive heart failure (CHF) was based on clinical grounds (history, physical examination, chest X-ray, electrocardiography, echocardiography and response to diuretic therapy) according to the AHA guidelines without taking account of NT-proBNP levels (13).
Pleural effusions were accepted to be malignant when malignant cells were determined on cytological examination. Positive pleural fluid or sputum AFB smear and/or culture or granulomatous inflammation on pleural biopsy, were accepted as tuberculosis pleuritis. In case of clinical findings compatible with pneumonia and response to antimicrobial treatment and/or positive culture results, the pleural effusion was accepted to be parapneumonic.
Pleural effusions were classified as transudate or exudates according to the Light's criteria. After the termination of the study, clinical diagnosis was made independently from biochemical criteria including the discrimination of the pleural fluid as transudate or exudate.
Statistical Analysis
Data of NT-proBNP levels were presented as median (25th to 75th percentiles). NT-proBNP levels of serum and pleural fluid were compared by t test. Median levels of NT-proBNP levels according to the clinical diagnosis were analyzed by Kruskal Wallis test. Mann-Whitney test was used to compare the levels of NT-proBNP between transudates and exudates as well as CHF and non-cardiac reasons. A correlation analysis was done with Spearman's correlation.
Statistical analyses were performed with SPSS 14.0 package program.
RESULTS
Mean age of the 45 patients included in the study was 58.95 ? 20.48. There were 28 males (62%) and 17 females (38%) in the study population. At the end of the routine diagnostic procedures, 13 patients were diagnosed to have malignant effusions, 10 had infectious effusions (parapneumonic n= 3, tuberculosis n= 7), while in 21 of the patients the pleural effusions were due to heart failure and in 1 it was due to pulmonary embolism.
Median (25th to 75th percentiles) NT-proBNP levels of serum and pleural fluid due to heart failure were 4747 pg/mL (931-15754) and 4827 pg/mL (1290-12430) while median NT-proBNP levels of serum and pleural fluid related with non-cardiac reasons were 183 pg/mL (138-444) and 245 pg/mL (187-556) respectively. NT-proBNP levels of serum and pleural fluid were significantly high in CHF (p< 0.001 for both). When four groups were compared serum and pleural fluid NT-proBNP levels were highest in the CHF group followed by malignancy, infection and others (p< 0.001 for both) (Figure 1, 2).
Serum and pleural fluid NT-proBNP levels were found to be related with each other (r= 0.879, p< 0.001).
Pleural fluid evaluation according to Light's criteria revealed exudates in 38 patients and transudates in 7 patients. Serum and pleural fluid NT-proBNP levels were higher in transudates and this reached statistically significance for pleural fluid (p= 0.009) (Figure 3, 4).
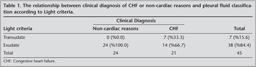
Twenty-one patients who were diagnosed as CHF had high NT-proBNP levels, however among them pleural effusions of 14 patients were classified as exudates according to Light's criteria. They were all on diuretics. Albumin gradient classification demonstrated that 4 out of these 14 patients' pleural effusions were transudates. The relationship between the clinical diagnosis of CHF and pleural effusion classification with respect to Light's criteria is shown in Table 1.
DISCUSSION
In our study, we investigated the diagnostic value of NT-proBNP levels in serum and pleural fluid for discriminating pleural effusions due to CHF. We found serum and pleural fluid NT-proBNP concentrations significantly higher in patients with CHF, than in patients with noncardiac pathologies.
Light's criteria which have been used widely in the diagnostic algorithm of the pleural effusions sometimes fail to discriminate transudative effusions (5). Therefore new biomarkers have been investigated in patients with CHF. NT-proBNP, with physiological effects as diuresis and natriuresis and vasodilatation has been shown to be useful as a serum biomarker of CHF (13,17). Serum BNP levels reflect the severity of CHF and decrease with decompensated heart failure treatment (18,19). Pleural fluid NT-proBNP has been suggested to derive from serum NT-pro BNP which can diffuse into the pleural space (20). Many studies have demonstrated high serum and pleural fluid NT-proBNP concentrations in patients presenting with pleural effusions due to decompansated heart failure (2,5,21). It has been recommended that in the diagnosis of pleural effusions due to CHF, especially in dual pathologies, increased NT-proBNP levels may be helpful in detecting the cardiac etiology (17). In our study, both serum and pleural fluid NT-proBNP levels were found to be increased in patients with CHF and the highest values were observed in cardiac pathologies among other causes as malignancy and infection. Median (25th to 75th percentiles) NT-proBNP levels of serum and pleural fluid due to heart failure have been reported to be between 3227-10791 pg/ml (267-20.263) and 6295-10.427 pg/mL (3342-21.844), while median NT-proBNP levels of serum and pleural fluid related with non-cardiac reasons have been shown to be between 236-989 (296-1691) pg/mL and 277-947 pg/mL (372-1937) respectively (2,5,15,16). Our results of NT-proBNP levels for pleural fluid and serum were also found in this range.
Kolditz and colleagues have shown that serum and pleural fluid NT-proBNP concentrations were more useful than Light's criteria in the differential diagnosis of cardiac and non-cardiac origins of pleural effusions. They have suggested that Light's criteria would still be used as an initial step in the diagnosis of pleural effusions; however NT-proBNP could be a supplementary tool for differential diagnosis, especially in transudative effusions (5). In many patients with CHF, usually at least one of Light's criteria is met and this leads to false positive results. One of the explanations of these false exudates is diuretic treatment which increases total protein and lactate dehydrogenase concentrations in pleural fluid (22). In our study, 14 patients were diagnosed as CHF clinically, however their pleural fluids were analyzed as exudates. In the scope of these findings; we think that as well as biochemical analysis of the Light's criteria, pleural fluid NT-proBNP analysis should be done especially when there is a suspicion of CHF.
In our study, serum and pleural fluid NT-proBNP concentrations were found to be significantly related. Kolditz and colleagues have pointed out that plasma and pleural fluid NT-proBNP levels had similar diagnostic accuracy, which confirmed another study that had demonstrated a high correlation also (5,16). Therefore, in case of risky diagnostic thoracenthesis, plasma NT-proBNP measurements could be used as a predictor of cardiac originated pleural effusions. Another finding supporting this suggestion is the lower concentrations of NT-proBNP in non-cardiac originated pleural transudates (15). We found serum and pleural fluid NT-proBNP levels to be higher in transudates and this reached statistically significance for pleural fluid (p= 0.009).
In patients with heart failure, blood brain natriuretic peptide levels have been reported to be greater than 500 pg/mL, while for levels under 100 pg/mL, usually no cardiac pathology can be determined (23). In a study with 64 patients, serum NT-proBNP levels of 520 pg/mL had a sensitivity of 97% and a specifity of 89%, while Kolditz have reported a sensitivity of 88% and a specifity of 93% for a cut off value of 4000 pg/mL for cardiac origin of effusions (2). The same study demonstrated similar sensitivity (92%) and specifity (93%) rates for pleural fluid NT-proBNP levels at 4000 pg/mL cut-off level and they have concluded that serum and pleural fluid NT-proBNP levels were closely correlated. In a series of 117 patients a cut of value of 1500 pg/mL for pleural fluid NT-proBNP levels had a sensitivity of %91 and a specifity of %93 for heart failure. In this series 10 patients were misclassified according to Light's criteria and had a NT-proBNP higher than 1500 pg/mL (15). Another study reported 100% sensitivity and 96.7% specifity for a cut off level of 2200 pg/mL (17). These different cut off points might be related with different BNP assays such as; research type enzyme linked immunoabsorbent assay (ELISA) kits or automated BNP assays, as well as biological variations, including gender, sex, obesity and renal functions (24). We couldn't determine a cut-off value for NT-proBNP which is one of the lacking points of our study.
In conclusion, measurement of pleural fluid NT-proBNP levels provide useful information in determining the cardiac origin of the effusions and it would be a smart approach to use this technique in company with Light's criteria. Larger prospective studies are required to confirm cut off points for NT-proBNP levels to be used as a discriminative marker of transudate of cardiac origin.
ACKNOWLEDGEMENT
Dr. Beyhan Cengiz Ozyurt contributed to statistical analyses and Dr. Nurhan Sarioglu helped in running out period of the study.
CONFLICT of INTEREST
None declared.
REFERENCES
- Light RW. Clinical practice. Pleural effusion. N Engl J Med 2002; 346: 1971-7.
- Gegenhuber A, Mueller T, Dieplinger B, et al. Serum B-type natriuretic peptide in patients with pleural effusions: preliminary observations. Chest 2005; 128: 1003-9. [?zet] [Tam Metin] [PDF]
- Heffner JE, Brown LK, Barbieri CA. Diagnostic value of tests that discriminate between exudative and transudative pleural effusions. Primary Study Investigators. Chest 1997; 111: 970-80. [?zet] [PDF]
- Porcel JM, Pe?a JM, Vicente de Vera C, Esquerda A. Reappraisal of the standard method (Light's criteria) for identifying pleural exudates. Med Clin (Barc) 2006; 126: 211-3. [?zet]
- Kolditz M, Halank M, Schiemanck CS, et al. High diagnostic accuracy of NT-pro BNP for cardiac origin of pleural effusions. Eur Respir J 2006; 28: 144-50. [?zet] [Tam Metin] [PDF]
- Gotsman I, Fridlender Z, Meirovitz A, et al. The evaluation of pleural effusions in patients with heart failure. Am J Med 2001; 111: 375-8. [?zet]
- Chakko SC, Caldwell SH, Sforza PP. Treatment of congestive heart failure. Its effect on pleural fluid chemistry. Chest 1989; 95: 798-802. [?zet] [PDF]
- Martinez Rumayor A, Richards AM, Burnett JC, Januzzi JL. Biology of the natriuretic peptides. Am J Cardiol 2008; 101(Suppl): 3A-8A. [?zet]
- Mukoyama M, Nakao K, Saito Y, et al. Human brain natriuretic peptide, a novel cardiac hormone. Lancet 1990; 335: 801-2.
- McCullough PA, Omland T, Maisel AS. B-type natriuretic peptides: a diagnostic breakthrough for clinicians. Rev Cardiovasc Med 2003; 4: 72-80. [?zet]
- Hobbs FD, Davis RC, Roalfe AK, et al. Reliability of N-terminal pro-brain natriuretic peptide assay in the diagnosis of heart failure: cohort study in representative and high risk community populations. BMJ 2002; 324: 1498. [?zet] [Tam Metin] [PDF]
- Steq PG, Joubin L, McCord J, et al. B-type natriuretic peptide and echocardiographic determination of ejection fraction in the diagnosis of congestive heart failure in patients with acute dyspnea. Chest 2005; 128: 21-9. [?zet] [Tam Metin] [PDF]
- Hunt SA, Baker DW, Chin MH, et al. American College of Cardiology/American Heart Association. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to revise the 1995 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 2001; 38: 2101-13. [Tam Metin] [PDF]
- Weber M, Arnold R, Rau M, et al. Relation of N-terminal pro B-type natriuretic peptide to progression of aortic valve disease. Eur Heart J 2005; 26: 1023-30. [?zet] [Tam Metin] [PDF]
- Porcel JM, Vives M, Cao G, et al. Measurement of pro-brain natriuretic peptide in pleural fluid for the diagnosis of pleural effusions due to CHF. Am J Med 2004; 116: 417-20.
- Tomcs?nyi J, Nagy E, Soml?i M, et al. NT-brain natriuretic peptide levels in pleural fluid distinguish between pleural transudates and exudates. Eur J Heart Fail 2004; 6: 753-6. [?zet] [Tam Metin] [PDF]
- Liao H, Na MJ, Dikensoy O, et al. Daignostic value of pleural N-terminal pro-brain natriuretic peptide levels in patients with cardiovasculer diseases. Respir 2008; 13: 53-7. [?zet]
- McCullough PA, Omland T, Maisel AS. B-type natriuretic peptides: a diagnostic breakthrough for clinicians. Rev Cardiovasc Med 2003; 4: 72-80. [?zet]
- Kazanegra R, Cheng V, Garcia A, et al. A rapid test for B-type natriuretic peptide correlates with falling wedge pressures in patients treated for decompansated heart failure: a pilot study. J Card Fail 2001; 7: 21-9. [?zet]
- Zemans RL, Chatterjee K, Matthay A. Diagnostic utility of B-type natriuretic peptide in patients with acute dyspnea or pleural effusions. Am J Med 2004; 116: 424-6.
- Porcel JM, Chorda J, Cao G, et al. Comparing serum and pleural fluid pro-brain natriuretic peptide (NT-proBNP) levels with pleural-to-serum albumin gradient for the identification of cardiac effusions misclassified by Light's criteria. Respirology 2007; 12: 654-9. [?zet]
- Romero-Candeira S, Fern?ndez C, Mart?n C, et al. Influence of diuretics on the concentration of proteins and other components of pleural transudates in patients with heart failure. Am J Med 2001; 110: 681-6. [?zet]
- Silver MA, Maisel A, Yancy CW, et al. BNP Consensus Panel 2004: a clinical approach for the diagnostic, prognostic, screening, treatment monitoring, and therapeutic roles of natriuretic peptides in cardiovascular diseases. Congest Heart Fail 2004; 10(Suppl 3): 1-30. [?zet]
- Porcel JM. The use of probrain natriuretic peptide in pleural fluid for the diagnosis of pleural effusions resulting from heart failure. Curr Opin Pulm Med 2005;11: 329-33. [?zet]
Yaz??ma Adresi (Address for Correspondence):
Dr. Aylin ?ZGEN ALPAYDIN,
Celal Bayar ?niversitesi T?p Fak?ltesi,
G???s Hastal?klar? Anabilim Dal?
45010 MAN?SA - TURKEY
e-mail: aylin.ozgen@yahoo.com